["febbf75bc7e34711993632af61fa8780045b476e"]
Breast Augmentation
breast
augmentation
implant types
implant selection
surgical approaches
postoperative treatment
complications
12223
12223
Chapter reads
1
1
Chapter likes
8/10
Evidence score
18
18
Images included
04
4
Videos included
01
Breast Augmentation with Breast Implants
Breast Augmentation with Breast Implants
This chapter focuses on comparing and analyzing randomized controlled studies to allow evidence-based knowledge about breast implants. In the field of plastic surgery, designing these studies is much more challenging than in other medical fields. Here, we analyze recent randomized controlled studies (RCT) in the field of aesthetic augmentation with breast implants tempting to provide a high-level evidence-based chapter. Despite the central role of aesthetic breast reconstruction, the best implants to use have rarely been studied in the context of large sample size RCTs. Though some RCTs have been performed representing the best evidence currently available34, they are often underpowered being inconsistent in their findings making conclusions difficult.
Breast augmentation is one of the most commonly performed aesthetic procedures with breast implants being a mainstay of modern medicine. The key to success of the perfect implant placement is careful preoperative patient selection, incision location, implant type and keeping the implant in the accurate position. Choosing implant shape and texture is one of the most essential yet controversial decisions in aesthetic breast augmentation.
Additionally, this chapter covers postoperative treatment methods, complications and surgical side infection as well as recommendations for the use of antibiotics (Figure 1). After aesthetic breast augmentation, up to 2.9% of women develop infection5.
For the first time, we will depict several RCTs about aesthetic breast augmentation with implants while our experts will debate about the outcome and practicability of these trials. This chapter will meta-analyze previous clinical trials to investigate the role of breast implants in augmentation patients and will provide optimized surgical procedures.
Breast augmentation is one of the most commonly performed aesthetic procedures with breast implants being a mainstay of modern medicine. The key to success of the perfect implant placement is careful preoperative patient selection, incision location, implant type and keeping the implant in the accurate position. Choosing implant shape and texture is one of the most essential yet controversial decisions in aesthetic breast augmentation.
Additionally, this chapter covers postoperative treatment methods, complications and surgical side infection as well as recommendations for the use of antibiotics (Figure 1). After aesthetic breast augmentation, up to 2.9% of women develop infection5.
For the first time, we will depict several RCTs about aesthetic breast augmentation with implants while our experts will debate about the outcome and practicability of these trials. This chapter will meta-analyze previous clinical trials to investigate the role of breast implants in augmentation patients and will provide optimized surgical procedures.
02
Introduction
Introduction
Breast augmentation is one of the most commonly performed aesthetic procedures with breast implants being a mainstay of modern medicine.
There is ample evidence that inadequate breast appearance can adversely affect self-esteem and body image, and this can be improved with augmentation mammoplasty6. First of all, for aesthetic reasons, there is implant-based breast augmentation. Implants are classified in different types depending on shape, surface and consistence. Many surgeons choose implants based on personal experience or expert opinion. Cheng et al. and Hidalgo et al. independently performed meta-analyses and RCTs stating no aesthetic superiority of anatomical implants compared to round implants78.
Regarding the surgical procedure, classifications depend on incisional technique, implant pocket placement and inframammary fold positioning. A Level of Evidence II study showed atrophy of the breast parenchyma after subglandular breast augmentation, but not following submuscular breast augmentation. In contrast, submuscular breast augmentation caused atrophy of the pectoralis major muscle9. Capsular fibrosis (CF) is the main long-term complication of breast implants. Combined data from previous RCTs suggest that the use of textured implants decreases the risk of this foreign body complications but (macro-)textured implants might be associated to an increased risk of breast implant–associated anaplastic large cell lymphoma (BIA-ALCL)1011.
Recent retrospective long-term studies have demonstrated negligible difference between textured and smooth implants with regard to the occurrence of CF13. Randomized controlled trials are required for a definitive understanding of the efficacy of surface texturing as there are no existing randomized controlled trials of modern smooth vs textured implants in the last 20 years.After aesthetic breast augmentation, up to 2.9% of women develop infection, with an incidence rate of 1.7% for acute infections and 0.8% for late infections5. Guidelines by the Centers for Disease Control (CDC) recommend surgical wounds be covered with a sterile dressing for 24 to 48 hours. An RCT performed in 2018 emphasized application of postoperative dressings play a key role in risk reduction.
In primary augmentation, a single dose of intravenous weight-based cefazolin given 60 min before skin incision appears to be adequate. Clindamycin or vancomycin are recommended for patients with β-lactam allergies. In secondary breast surgery, fluoroquinolones and vancomycin should be given 120 min before first incision (Figure 1). Using these principles of the 14-point plan by Adams et al. to minimize the bacterial load at the time of surgery, the development of subclinical infection and capsular fibrosis may be reduced significantly. No one approach suits every patient, and surgeons must be versed in many techniques to best serve individual variations in anatomy, surgeon and patient goals. The simple choice of implant size has been replaced with the objective measurement and planning of a detailed and patient-specific operation.
There is ample evidence that inadequate breast appearance can adversely affect self-esteem and body image, and this can be improved with augmentation mammoplasty6. First of all, for aesthetic reasons, there is implant-based breast augmentation. Implants are classified in different types depending on shape, surface and consistence. Many surgeons choose implants based on personal experience or expert opinion. Cheng et al. and Hidalgo et al. independently performed meta-analyses and RCTs stating no aesthetic superiority of anatomical implants compared to round implants78.
Regarding the surgical procedure, classifications depend on incisional technique, implant pocket placement and inframammary fold positioning. A Level of Evidence II study showed atrophy of the breast parenchyma after subglandular breast augmentation, but not following submuscular breast augmentation. In contrast, submuscular breast augmentation caused atrophy of the pectoralis major muscle9. Capsular fibrosis (CF) is the main long-term complication of breast implants. Combined data from previous RCTs suggest that the use of textured implants decreases the risk of this foreign body complications but (macro-)textured implants might be associated to an increased risk of breast implant–associated anaplastic large cell lymphoma (BIA-ALCL)1011.
Recent retrospective long-term studies have demonstrated negligible difference between textured and smooth implants with regard to the occurrence of CF13. Randomized controlled trials are required for a definitive understanding of the efficacy of surface texturing as there are no existing randomized controlled trials of modern smooth vs textured implants in the last 20 years.After aesthetic breast augmentation, up to 2.9% of women develop infection, with an incidence rate of 1.7% for acute infections and 0.8% for late infections5. Guidelines by the Centers for Disease Control (CDC) recommend surgical wounds be covered with a sterile dressing for 24 to 48 hours. An RCT performed in 2018 emphasized application of postoperative dressings play a key role in risk reduction.
In primary augmentation, a single dose of intravenous weight-based cefazolin given 60 min before skin incision appears to be adequate. Clindamycin or vancomycin are recommended for patients with β-lactam allergies. In secondary breast surgery, fluoroquinolones and vancomycin should be given 120 min before first incision (Figure 1). Using these principles of the 14-point plan by Adams et al. to minimize the bacterial load at the time of surgery, the development of subclinical infection and capsular fibrosis may be reduced significantly. No one approach suits every patient, and surgeons must be versed in many techniques to best serve individual variations in anatomy, surgeon and patient goals. The simple choice of implant size has been replaced with the objective measurement and planning of a detailed and patient-specific operation.
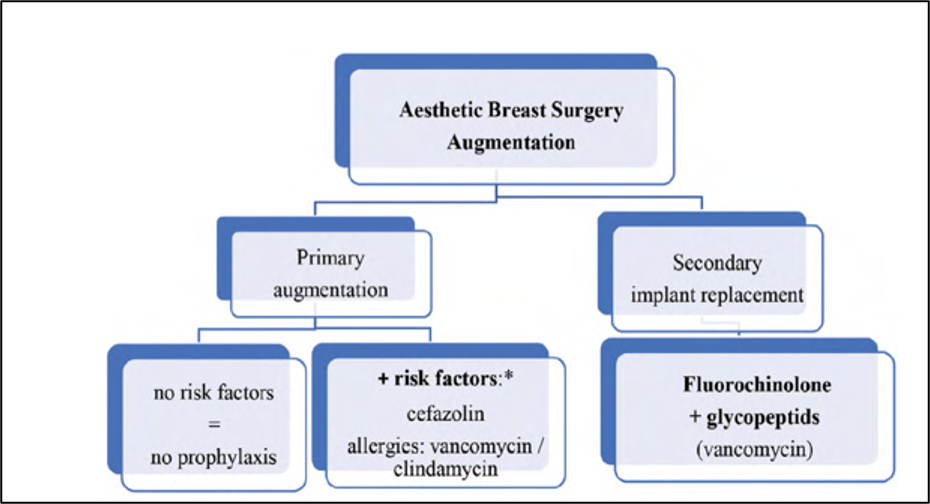
Figure 1 Algorithm for the choice of antibiotics in aesthetic breast surgery augmentation.
03
Definition
Definition
Breast augmentation (=augmentation mammoplasty) uses breast implants or fat transfer to increase the size, change the shape/volume, and alter the texture of females´ breasts.
04
Classification / Types of Breast Implants
Classification / Types of Breast Implants
Most commercially available breast implants feature some degree of elastomer surface modifications to increase surface roughness. However, manufacturing processes of breast implants differ from company to company, including a differently used taxonomy, complicating valid scientific comparisons between breast implants of different companies.
Two basic types: Silicone and Saline Breast Implants
Silicone Breast Implants
Saline Breast Implants
Silicone shell filled with plastic gel (=silicone)
Silicone shell filled with sterile salt water (=saline)
First introduced in 1964, approved by the FDA in November 2006
First introduced in 1970s, approved by the FDA in May 2000
Natural appearance, lower risk of rippling
Can be inserted empty to minimize incision, diffusion of salt water
Come in different sizes and profile
Come in different sizes and profiles
Can have either smooth or textured shell
Can have either smooth or textured shell
If ruptured, silicone gel will remain within the implant shell and implant will not collapse
If ruptured, implant will collapse, and saline will be absorbed
Silicone gel implants vary in terms of gel cohesivity and form stability. Various degrees of gel cohesivity are obtained by varying the density of crosslinking between silicone polymers17. Less cohesive gels are less crosslinked, are more elastic, and have a softer feel while more cohesive gels more crosslinked, are less elastic, and have a firmer feel. Silicone gel filled implants have been improved since their introduction and nowadays fourth and fifth-generation gel devices are available1819.
Shape of Breast Implants
Round Shaped Breast Implants
Anatomic (Tear Drop) Shaped Breast Implants
Come in different sizes and profiles
Come in different sizes and profiles
Can be filled with saline or silicone gel
Can be filled only with silicone gel
Good choice for women who want a full upper pole, or upper portion of the breast
Good choice for women who want to correct mild sagging or ptosis
Provide more lift and cleavage
Thinner upper area than bottom, gradually sloping to a fuller and more projected fullness below the nipple
Less likely to wrinkle
Mimics natural breast
Completely symmetrical shape
Asymmetric shape
Lower risk of rotating
Higher risk of rotating
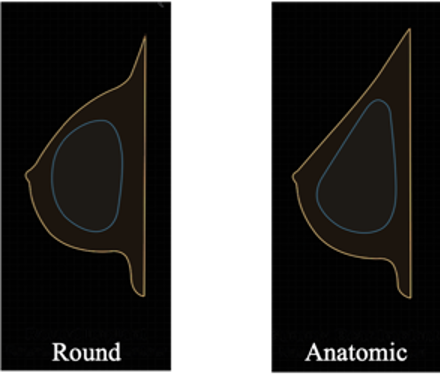
Figure 2 Different shapes of breast implants
One result of anatomically shaped breast implants combined with a more cohesive gel is that collapse and wrinkle formation of breast implants can be prevented.
Profile Types of Breast Implants
Implant “profile” is not the same as implant projection. Implant projection is a quantifiable linear measurement of the anterior–posterior dimension of the implant, whereas implant “profile” is a vendor-driven assessment that currently lacks universal standardization. Until “profile” assessments are standardized across vendors, it behooves us to be cognizant of their limitations as primary variables used to guide implant selection.
The confusion between implant “profile” and projection arises from the occasional misuse of the 2 terms interchangeably. Commonly, implant “profile” is inadvertently referred to as its “projection” (i.e., calling a “high profile” implant a “high projection” implant). Implant projection is the linear measurement of the anterior–posterior dimension of an implant. It is a single, numerical dimension, whereas “profile” is a 3-dimensional descriptor of implant projection (and hence, volume) relative to its base diameter. In essence, “profile” encompasses a permutation of all 3 implant dimensions, whereas projection represents only a single dimension20.
Nowadays, we have an inconsistent use of “profile“ classifications, where multiple manufacturers have independent control over their implant classifications, what holds true for a high-profile implant from a certain vendor may not hold true for a similarly classified implant from another. Adding to the confusion is the variety of descriptors that have been added to the traditional profile types, such as low-plus, moderate-classic, moderate-plus, moderate-high, midrange, full, extra-full, and ultra-high profiles (Figure 3).
The confusion between implant “profile” and projection arises from the occasional misuse of the 2 terms interchangeably. Commonly, implant “profile” is inadvertently referred to as its “projection” (i.e., calling a “high profile” implant a “high projection” implant). Implant projection is the linear measurement of the anterior–posterior dimension of an implant. It is a single, numerical dimension, whereas “profile” is a 3-dimensional descriptor of implant projection (and hence, volume) relative to its base diameter. In essence, “profile” encompasses a permutation of all 3 implant dimensions, whereas projection represents only a single dimension20.
Nowadays, we have an inconsistent use of “profile“ classifications, where multiple manufacturers have independent control over their implant classifications, what holds true for a high-profile implant from a certain vendor may not hold true for a similarly classified implant from another. Adding to the confusion is the variety of descriptors that have been added to the traditional profile types, such as low-plus, moderate-classic, moderate-plus, moderate-high, midrange, full, extra-full, and ultra-high profiles (Figure 3).

Figure 3 Different profiles of breast implants
Surface of Breast Implants
Surface texture of a breast implant influences tissue response and ultimately device performance. Smooth implants can move around within the capsule, but this does not cause a change in appearance the way textured implants do when they move. Texturing is considered a requirement to provide friction and reduce malposition. To mitigate the risk of capsular fibrosis (CF), the implant´s shells were textured based on the theory that an irregular shell surface would prevent the parallel alignment of collagen fibers thus, by extension, preventing CF21. Preliminary studies supported this theory with an observed reduction in CF rates23 but recent implant studies have demonstrated negligible differences in contracture rates between textured and smooth styles1213.
Recent research has suggested a reproducible association between textured implants and the development of breast implant-associated anaplastic large cell lymphoma (BIA-ALCL), a potentially fatal T-cell lymphoma (see section Complications: BIA-ALCL).
Conclusively, Polyurethane-coated implants (PU) have the highest surface area and were an attempt to reduce capsular fibrosis but were prone to degrade. Thus, resulting in a thin, pliable shell that was more susceptible to visible folds, rupture, silicone leakage and late presumably CF2425.
Recent research has suggested a reproducible association between textured implants and the development of breast implant-associated anaplastic large cell lymphoma (BIA-ALCL), a potentially fatal T-cell lymphoma (see section Complications: BIA-ALCL).
Conclusively, Polyurethane-coated implants (PU) have the highest surface area and were an attempt to reduce capsular fibrosis but were prone to degrade. Thus, resulting in a thin, pliable shell that was more susceptible to visible folds, rupture, silicone leakage and late presumably CF2425.
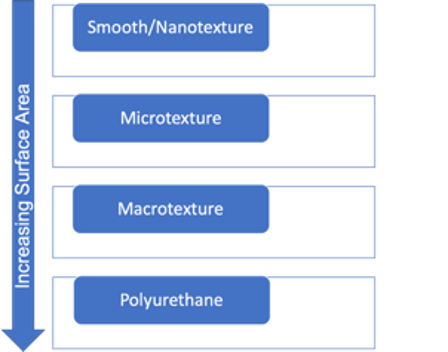
Figure 4 Different surfaces of breast implants
05
The Ideal Breast
The Ideal Breast
Is there an ideal breast?
Beauty is in the eye of the beholder-this proverb is as old as it is true.
The authors of this chapter can´t agree more, especially when it comes to the perfect aesthetic breast.
There rarely have been objective data in the plastic surgical literature to define an aesthetically pleasing template for the ideal breast that everybody agrees upon.
Mallucci et al. propose that the perfect breast with universal appeal has an upper pole-to lower pole ratio of 45:55 (slightly fuller lower pole than upper pole), an upward pointing nipple (20-degree mean angle), a straight/mildly concave upper pole slope and a smooth lower pole convexity26 (Figure 5). The breasts’ overall aesthetic appeal is more important than their size.
Beauty is in the eye of the beholder-this proverb is as old as it is true.
The authors of this chapter can´t agree more, especially when it comes to the perfect aesthetic breast.
There rarely have been objective data in the plastic surgical literature to define an aesthetically pleasing template for the ideal breast that everybody agrees upon.
Mallucci et al. propose that the perfect breast with universal appeal has an upper pole-to lower pole ratio of 45:55 (slightly fuller lower pole than upper pole), an upward pointing nipple (20-degree mean angle), a straight/mildly concave upper pole slope and a smooth lower pole convexity26 (Figure 5). The breasts’ overall aesthetic appeal is more important than their size.
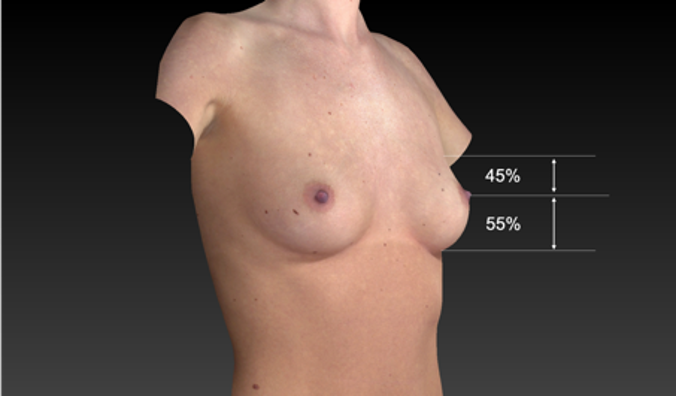
Figure 5 45:55 ratio of ideal breast (modified after Mallucci et al., 2012., breast image: Canfield Vectra)
Here, we try to identify some key parameters as the basis for the design of ideal breast proportions by combining recent studies that have tried to identify some key parameters that nearly everyone agrees upon and show our own best practice. The most important consideration when it comes to breast augmentation is the patient´s own personal goals for the procedure.
06
Preoperative Key Measurements - Placement of Breast Implants
Preoperative Key Measurements - Placement of Breast Implants
Including step-by-step photos and videos of preoperative markings
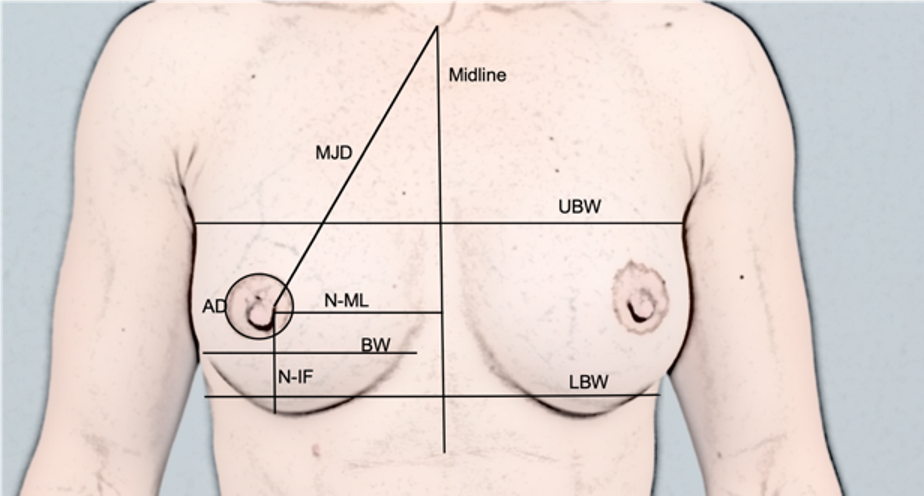
Figure 6 MJD: Mamille-Jugulum-Distance, UBW: Upper Breast Width, LBW: Lower Breast Width, AD: Areola Diameter, BW: Breast Width, N-MF: Nipple to Midline, N-IF: Nipple to Inframammary Fold (IFM)
MJD: 19-21cm
N-ML: 9-11cm
N-IF: 7-8cm
BW (= breast base): 11-14cm
AD: 3.5-4.5cm
Nipple diameter: 0.5-0.8cm
Nipple projection: 0.4-0.6mm
Breast projection out of the thorax line: 1-3cm
Predicting the final position of the inframammary fold is critical to determining the placement of all breast incisions, but especially the inframammary incision.
In the High Five System analysis28, variables are analyzed including implant volume, patient’s base width, implant base width, anterior pulled skin stretch, and nipple-to-fold distance under maximal stretch. Based on the selected implant, a reference chart provides the desired nipple-to-fold distance, which if longer than the measured distance, will require IMF lowering (Figure 7).
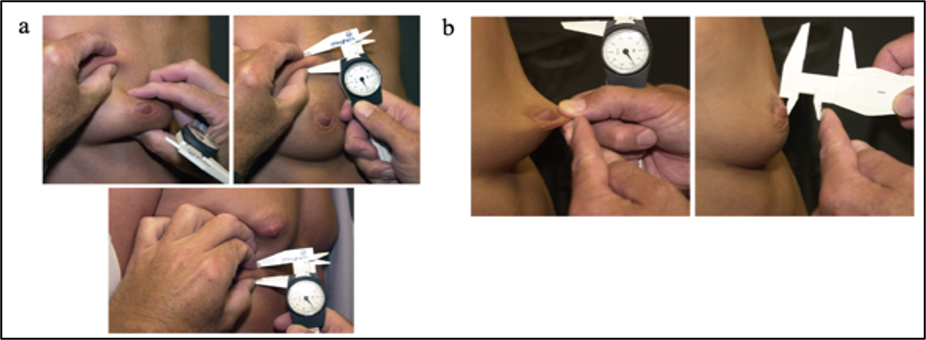
Figure 7 Pinch test of upper and lower pole (a) and stretch test of the nipple (b) (Tebbetts et al., 2005)
IMF and Implant Volume
Identify new IMF by marking the new IMF with the patient´s arms lowered AND elevated
Pinch Test/Skin Stretch: Identifies the dermis and subcutaneous fat ratio which helps to choose the right implant basis and placement
If pinch thickness 3 cm: + 30cc
Nipple-to-inframammary fold distance (N:IMFMaxSt), measured under maximal stretch
Parenchymal fill (percentage of skin envelope filled)
Based on our experience, we think that the best way to identify the new IMF is with patient’s arms lowered and secondly elevated (see above "IMF and Implant Volume"). But there are many different ways to identify the new IMF.
Dr. Bradley Calobrace for example recommends the following: “The true fold, the best predictor of where the fold will lie postoperatively, is assessed by autorotation of the breast inferiorly to identify the inferior extent of the fascial attachments at the fold.”29.
Key Measurements in Achieving Customized Ideal Breast Augmentation with Breast Implants – Details:
Identify Midline: identify Jugular notch and draw a straight line along the Xiphoid process down to the umbilicus CAVE: thorax deformation and belly fat, for better orientation palpate the Proc. xiphoideus sterni and identify the linea nigra
Measure MJD (no need to mark it)
Identify N-ML: is the distance symmetric?
Identify natural IFM (mark with dots)
Identify new IFM and location of the incision:Mark the nipple position with lowered AND the new position with elevated arms. Then mark the new nipple position as the half diameter of the implant base. The new IMF will be placed on this horizontal line.Control it with the length of “D” (=N-IF) by stretching the skin.
Cave: If the distance “D” is too short, a smaller implant is selected plus lowering of IMF is recommended. Here, the new IMF is created using a blunt technique, if the distance between old and new IMF is about 1cm. Is this distance greater than 1cm (e.g. tubular breast), additional fixation sutures are necessary.
Mark the new IFM from its medial and lateral ends. Measure distance from the medial end to the ML and transfer exactly the same distance to the other breast to achieve the most symmetric distance to the sinus.
Make sure the medial and lateral ends have the same distance to the new IMF.
Identify Breast Base (width and height).
Identify location of nipple: is nipple central? If the nipple is more lateralized, the implant needs to be place more lateral If the nipple is more medialized, the implant needs to be placed more medial.
Choose your incision type:
Periarealor Incision: Big NAC (Nipple-Areola-Complex), implant size up to 250cc
Inframammary Incision: Breast feeding, incision is done: 1/3 medial and 2/3 lateral (with NAC being the center). See Photos 1 - 4 for a detailed, step-by-step photo instruction of preoperative marking. Incision length varies according to implant size:
Implant size
Incision Length
200cc
4cm
250cc
4.5cm
300cc
5cm
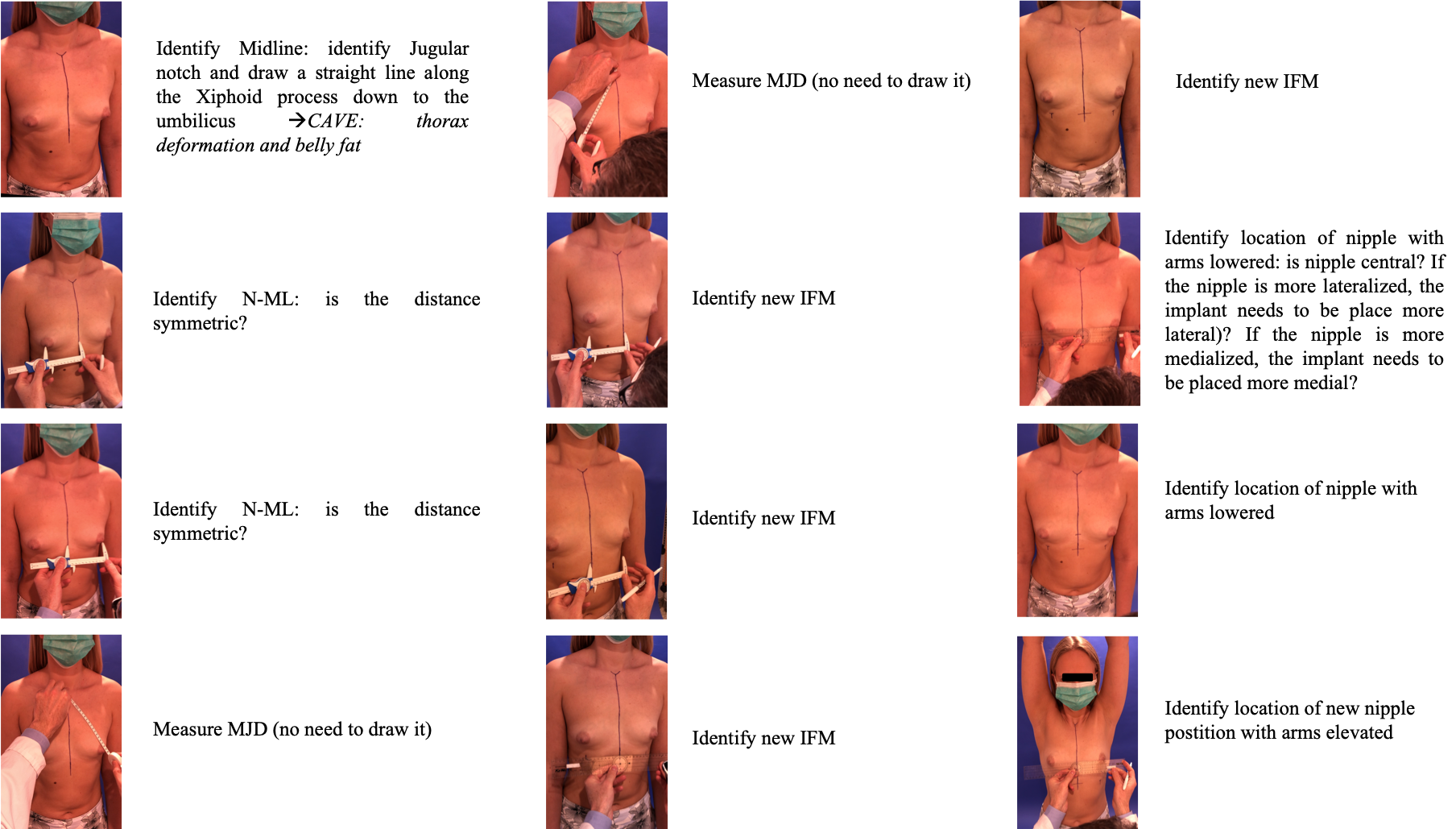
Photo Collage, Part 1
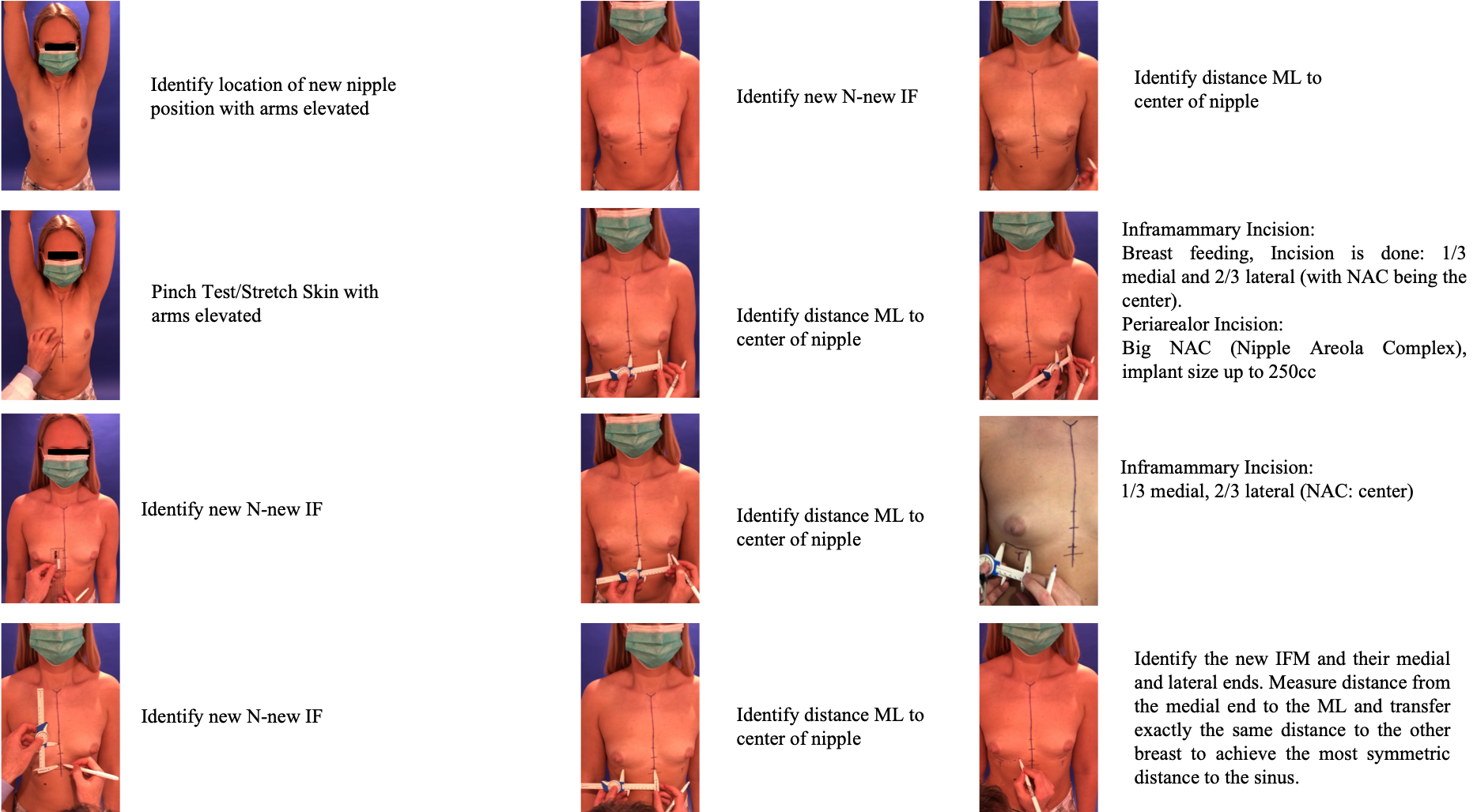
Photo Collage, Part 2
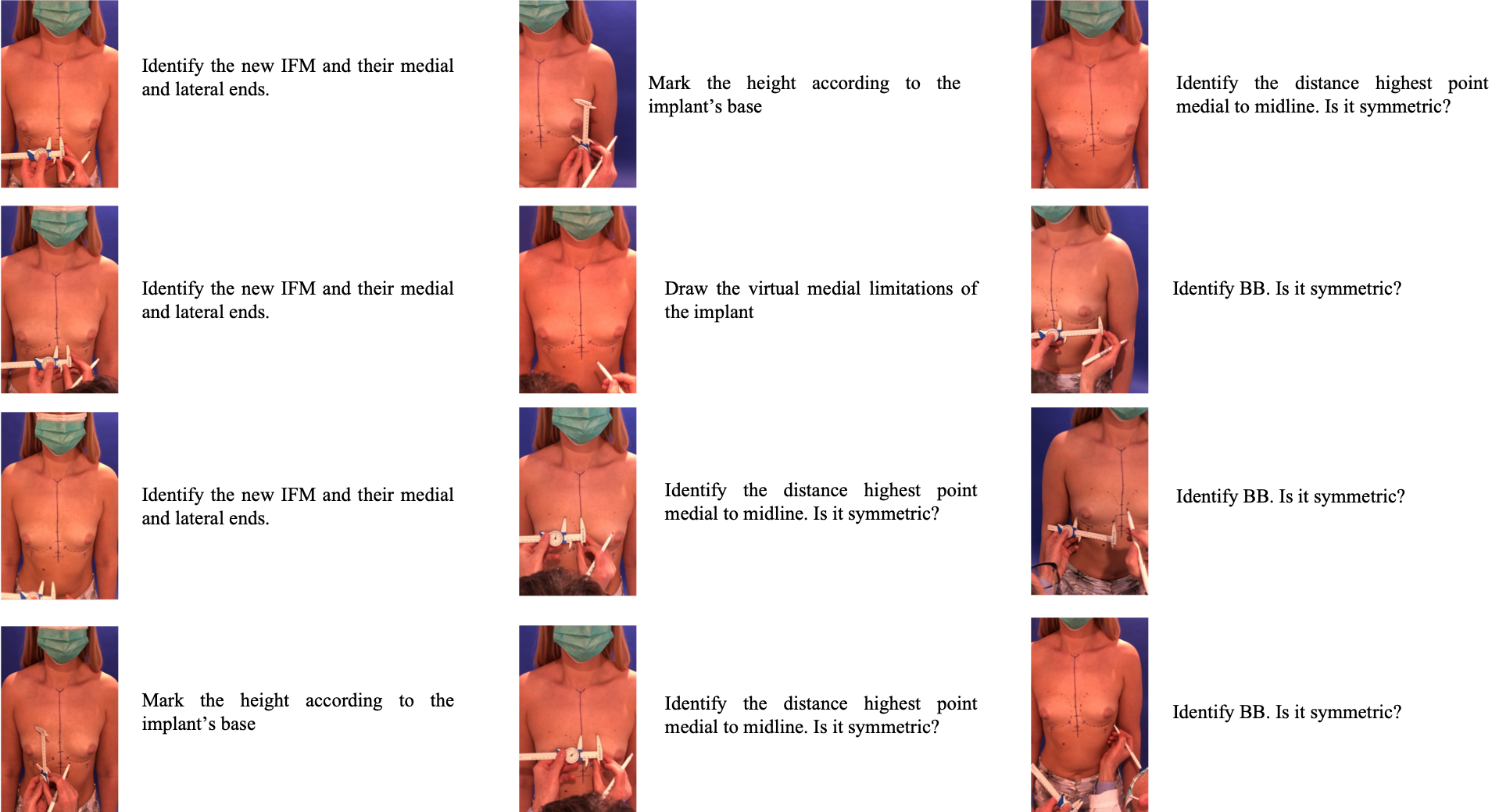
Photo Collage, Part 3
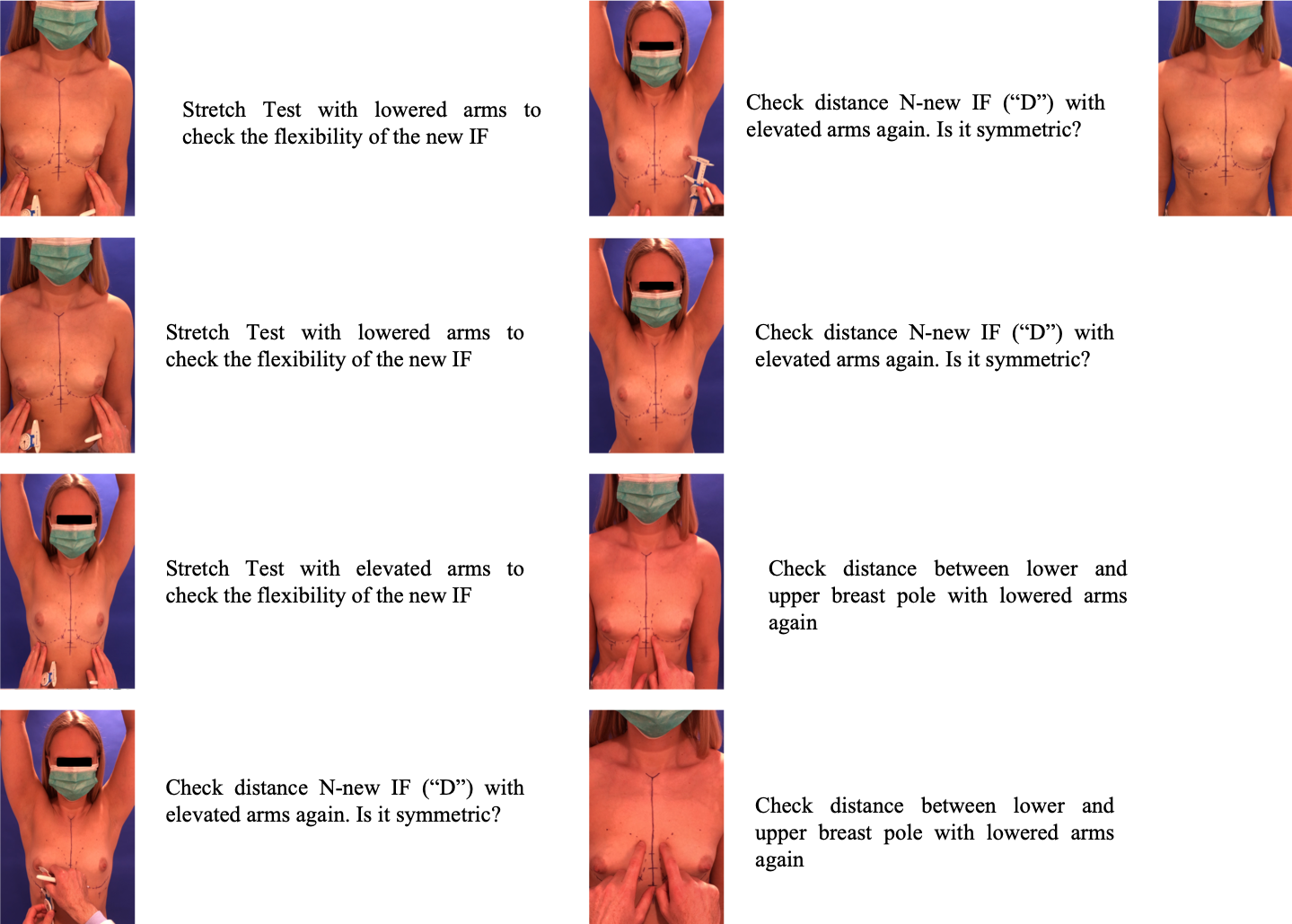
Photo Collage, Part 4
Patient positioning on the operating table
Supine position
Arms are secured either at the patient’s side or outstretched on an arm-board, positioned at 45° to stabilize the patient in the upright position
CAVE
Do NOT overextend patient´s arms: M. pectoralis needs to be relaxed in order to provide a more accurate assessment of the implant position and to re-drape the breast tissue overlying it.
Placing the arms by the patient’s side is a useful alternative.
DON´T: Arms outstretched at 90°: this position can lead to misinterpretation of the breast–implant relationship due to breast elevation when placed in this position.
07
Implant Selection
Implant selection
Key Measurements and Calculations
As always, there is no single unique and absolutely correct technique but each system contributes significant critical detail to the breast surgeon’s ability to provide reproducibly, beautiful and safe results.
Using Anatomic Implants
Estimated Volume
N-IF
200
7
250
7
275
7.5
300
8
325
8
350
8.5
375
9
400
9.5
The “Number Y”
The selection of the implant height should follow the patient’s breast implantation base, which is highly influenced by the body type. With this assumption, the “number Y” was developed30. It correlates the suprasternal notch-to-nipple distance with the thoracic perimeter and reveals the shape of the optimum breast implant base in the particular patient. The number Y can help to rationalize the selection of the implant height in breast augmentation.
Number Y = Thoracic perimeter / Suprasternal notch-to-nipple distance
Implant Selection
BW and N-IF are the most important measurement parameters
Measure with arms down AND arms up
Use Pinch Test and Stretch Test (skin)
Implant Volume
Most women do not know their accurate cup size!
Calculation according an average body-size woman with thorax circumference of about 75cm (Modified from Botti G et al.):
Cup Size
Implant Size (cc)
AA
50-100
A
200
B
~350
C
500
D
650
Per larger size
Increase of 150cc
Implant Incision
Inframammary Incision: Best way to visualize the pocket, allows shortening of N-IMF distance
Periareolar Incision: Areolar diameter > 3.5cm and breast implant < 300cc, allows adjustment of IMF
Transaxillary Incision
Transumbilical Incision
Implant Position
The breast implant pocket should be slightly larger than the footprint of the implant
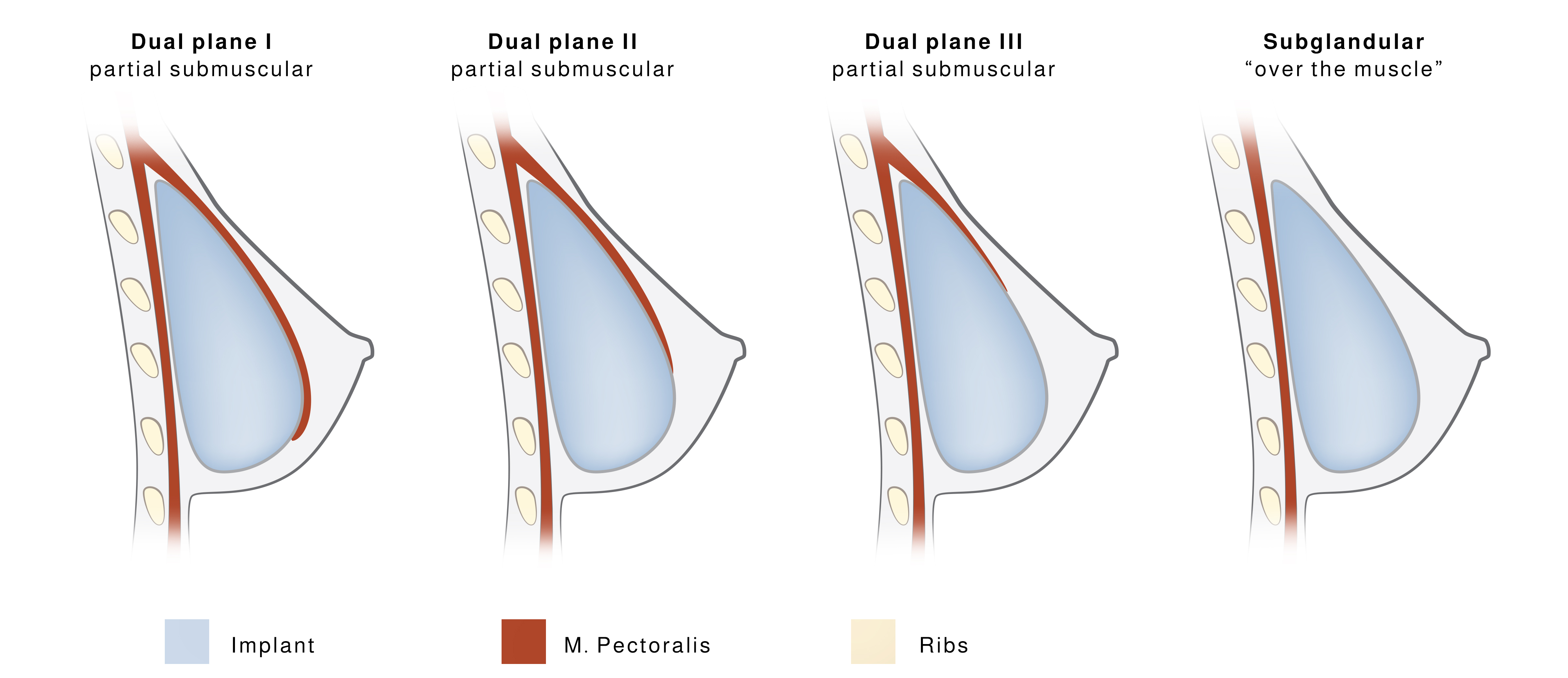
Figure 8 Different breast implant positions
It can be clinically challenging to precisely perform Dual Plane I – III: M. pectoralis tends to bounce up once being released
Subglandular (if Pinch Test > 2cm)
Implant is placed over the Musculus pectoralis (breast muscle) but beneath the skin, fat and glandular tissue of the breast
Increased risk of visible edges, rippling, wrinkling
In slim patients with little subcutaneous fat tissue: Dissect through the caudal third of the gland
Subfascial (if Pinch Test > 2 cm)
Implant is placed pocket between the fascia and the M. pectoralis major muscle
Better tissue coverage with less visible edges, rippling, wrinkling
Careful preparation of the fascia, in some patient is really thin
Dual Plane
Dual Plane I = Submuscular
Implant is partially placed submuscular with only a minimal amount of overlying breast parenchyma is released from the lower attachments of the M. pectoralis major
Dual Plane I breast augmentation describes the classic partial submuscular with the origin of the M. pectoralis major is divided from its origin at the level of the IMF
Dual Plane II
Implant is partially placed submuscular with a greater release of the M. pectoralis at the level of the nipple and the overlying breast parenchyma is released partway up to the nipple
Improves very slight sagging
Dual Plane III
Implant is partially placed submuscular with the greatest release of M. pectoralis at the level of the nipple and the overlying breast parenchyma may be released all the way up to the nipple
Improves minor sagging
Unique “Submuscular-Attached-to-Fascia” technique Regensburg
Compared to the dual plane technique: M. pectoralis is NOT divided, only released
Inframammary incision along IMF, 2/3 of the incision are placed laterally the nipple
Dissect through deep Scarpa's fascia until pectoralis fascia is identified
Lower subglandular dissection until lateral border of the M. pectoralis major is identified
Separate loose connective tissue under M. pectoralis major from M. pectoralis minor
Don’t dissect implant pocket too far lateral! - Place patient in sitting position to 90°!
Lower to Medial Curvature Release: Release pectoralis major (similar to Dual Plane II) at the lower IMF until subcutaneous fat tissue is visible (medial limit)
Medial Areola to Cranial Release: Continue until areola (limit), then switch and JUST release muscle including its perforators (medial intercostal perforator (3rd-4th ICS) should carefully be coagulated) but LEAVE several adhesions of the muscle/fascia to avoid symmastia. This release can be continued until the cranial end of the implant´s pocket, so the sinus can be narrowed
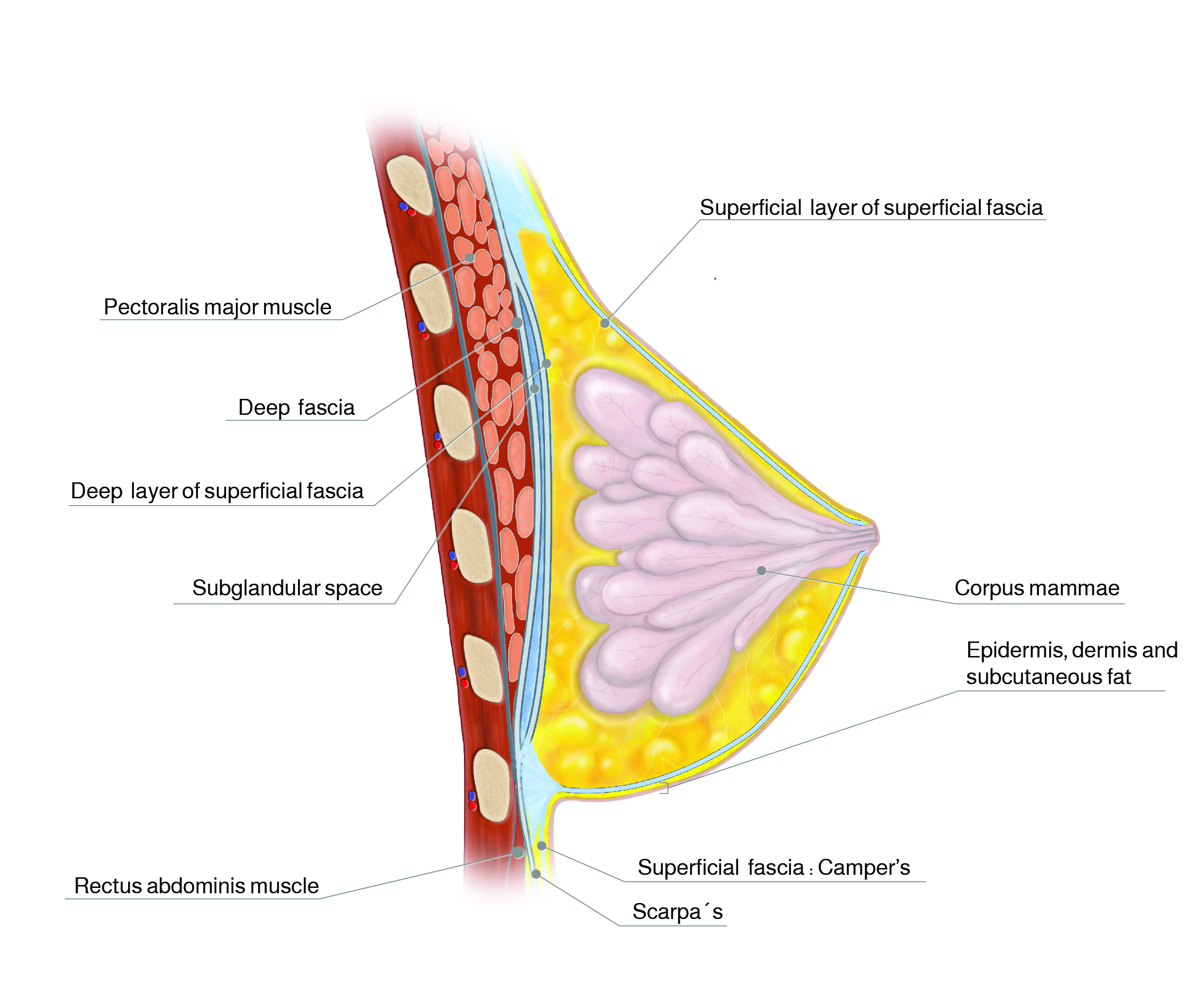
Figure 9 Superficial fascial system; sagittal view. The corpus mammae is bounded by two layers of fascia and fat (from Gilbert S; Rehnke RD, 2018.)
08
Algorithm Flow Chart Aesthetic Breast Augmentation
Algorithm Flow Chart Aesthetic Breast Augmentation
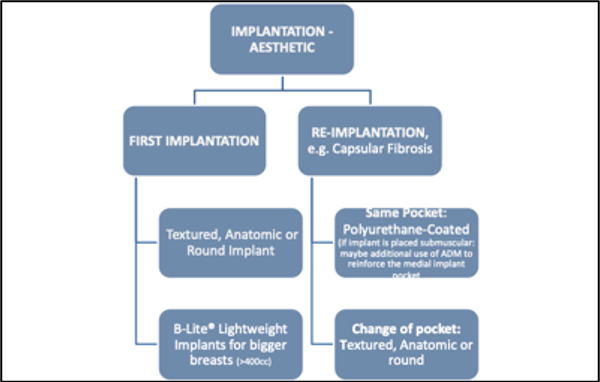
Figure 10 Algorithm flow chart for aesthetic breast implant augmentation (Regensburg)
09
Standardized Surgical Procedure
Standardized Surgical Procedure for Aesthetic Breast Augmentation with Implants (in Accordance to Flow Chart Regensburg)
First Aesthetic Implantation of Breast Implants
Textured anatomic implants or round implants, personalized to each individual patient
Thin patients/Pinch Test: subpectoral implantation of implant, other than that: subglandular positioning of the breast implant
Breast volume >400cc desired/applicable: (B-Lite) Lightweight Breast Implants
Re-Implantation/Revision Aesthetic Implantation of Breast Implants
Explantation of breast implant
If same breast pocket is used: PU-coated breast implants. If implant will be placed subpectoral within the same pocket: additional use of ADM (acellular dermal matrix) may be considered due to reinforce the medial implant pocket
Use of ADM
ADMs were first introduced for use in revisional aesthetic surgery
Aesthetic reasons to use ADM include
Transection of M. pectoralis during Dual Plane with M. pectoralis bouncing up
Correction of implant rippling
Symmastia
Soft tissue deficits
If change of breast pocket is performed: see First Aesthetic Implantation of Breast Implants
10
Breast Implant Registry Form - Template Regensburg
Breast Implant Registry Form - Template Regensburg
Scandals concerning breast implants confuse patients, medical doctors and the public. Until now legally binding consequences are missing despite repeated requests. Since 2013 we have developed and implemented an own breast implant template for the daily clinic routine in Regensburg to increase the patient's safety and the assessment of implants in course of time31. The breast implant template optimizes the quality of surgical treatment and outcomes, quickly reveals complications, allows valuable tracing of breast implants and improves the consultation of patients.
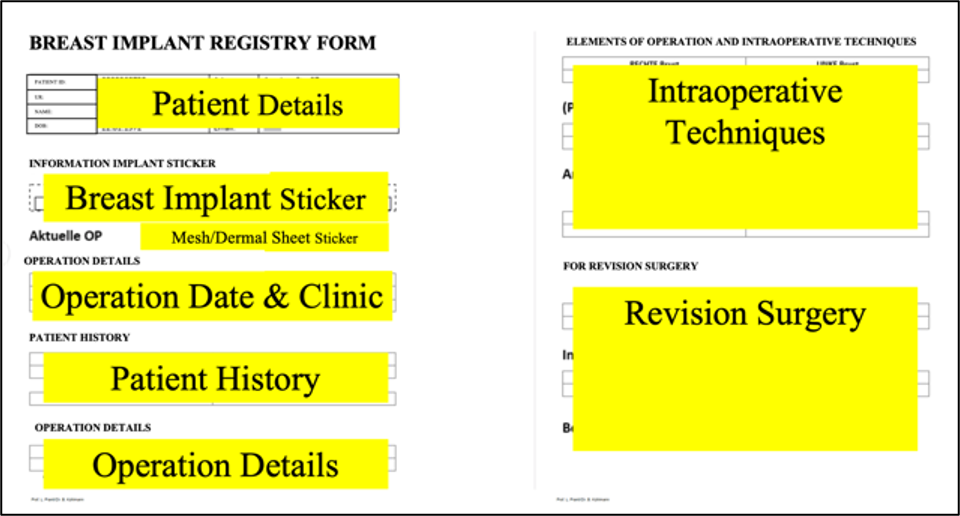
Figure 11 Breast template for every breast implant augmentation –augmentation and revision
11
Postoperative Management and Complications
Postoperative Management
Control of seroma, hematoma
Check blood level (hemoglobin)
If drain was placed, remove drain <40cc
Special sports bra for 4-6 week
Postoperative follow-ups at 7 days, 3 weeks, 3 months and one year postoperatively
2D- or 3D- photographic documentation and critical evaluation of surgical outcomes
Complications
Bottoming Out and Double-Bubble Deformities
Bottoming out and double-bubble represent common iatrogenic deformities for revision surgery in breast augmentation with breast implants.
Both are a malposition of the implant. While bottoming out is an inferior implant displacement with a high riding nipple, resulting in the lower pole being longer than it should be, double bubble is clinically characterized by double convexity of the lower pole due to the visible indentation of the old inframammary fold (IMF) that sits in the middle of the two convexities. Several clinical studies have been done to face this complication.
Both are a malposition of the implant. While bottoming out is an inferior implant displacement with a high riding nipple, resulting in the lower pole being longer than it should be, double bubble is clinically characterized by double convexity of the lower pole due to the visible indentation of the old inframammary fold (IMF) that sits in the middle of the two convexities. Several clinical studies have been done to face this complication.
A comprehensive understanding of IMF anatomy and the key surgical maneuvers to avoid these complications must be taken into account for each route of dissection.
Double-Bubble Deformity Type A (“waterfall deformity”)
Implant is above breast mound
Implant is held high on chest wall by total pectoral coverage or contracture. Loose parenchyma slides off M. pectoralis major inferior to axis of the implant
Double-Bubble Deformity Type B
Implant is below breast mound:
With significant overdissection of IMF, implant can slide caudal to the breastmound and create a second IMF below the native IMF and breast mound
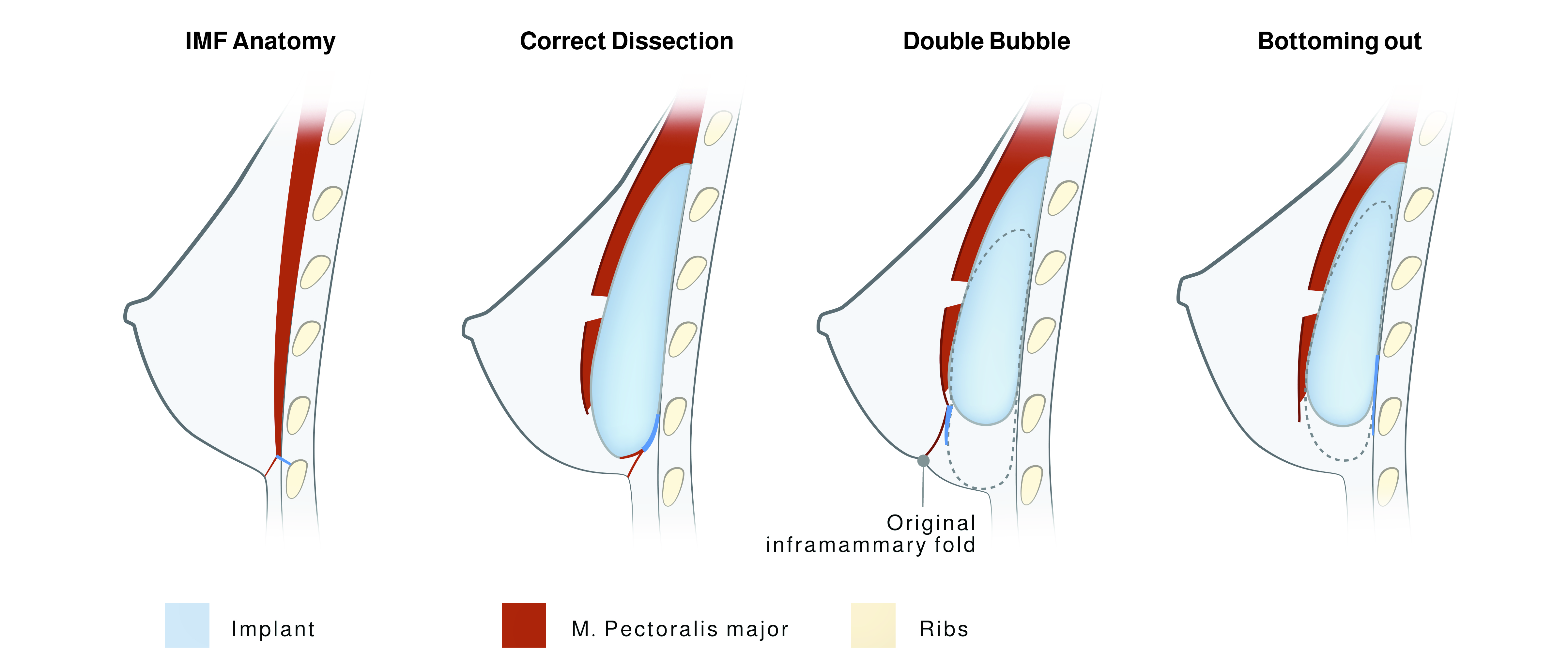
Figure 12 Diagrams of sagittal breast axis of normal IMF anatomy (above, left) where the dotted line arrow indicates the full-thickness incision of the breast tissue to reach the PM with the periareolar approach; implant positioning in a correct dissection route (above, right); double bubble characterized by the presence of a groove or indentation which creates a double convexity (below, left); and bottoming out characterized by a too lowered implant, without any double convexity and with an unaesthetic lengthening of the nipple to fold distance (below right) deformities (Salgarello et al., 2017)

Figure 13 Different types of breast that bear risks of bottoming out and doubble-bubble (Salgarello et al., 2017)
Salgarello et al. performed an anatomical and clinical study of women who underwent breast augmentation. They state that deformities can be avoided if an anatomical approach is used during pocket dissection at the level of the IMF, paying attention to avoid disrupting the superficial and deep attachments of the superficial pectoralis fascia at the IMF32.
Capsular Fibrosis
Capsular fibrosis around breast implants is the most common long-term complication. This complex foreign body response will be discussed in detail in Chapter: Implant Diagnostic.
Symmastia
Symmastia is the migration of one or both implants across the midline, leaving (almost) no natural sinus. Symmastia can be the result of:
Extremely large breast implants
Overdissection of the medial pocket (one breast or both breasts)
Disproportion between breast implants’ width and chest wall
Special Complication/Concern
BIA-ALCL
Recent research has suggested a reproducible association between textured implants and the development of breast implant–associated anaplastic large cell lymphoma (BIA-ALCL), a possibly fatal T-cell lymphoma. Although rare, the presence of a textured breast implant is thought to increase the risk of developing breast ALCL by an estimated 67 to 421 times33. Late-onset seroma and periprosthetic effusion are a rather common presentation, and few patients present with a firm mass. Thus, any delayed seroma occurring more than one year after implantation not explainable by infection or trauma might potentially be associated with BIA-ALCL and should therefore be investigated through fine-needle aspiration, flow cytometry, and CD30/ALK immunohistochemistry3435.
Concerns for causing malignancy in elective surgical patients have led the plastic surgery community to prioritize BIA-ALCL investigation, with numerous recent publications on the topic and the creation of a national registries in different countries313637383940. Since the first reported case in 199741, the incidence of patients with BIA-ALCL has been rapidly increasing, possibly due to an increased awareness. The U.S. Food and Drug Administration has been tracking and investigating ALCL and has released a report linking ALCL to textured implants42.
NCCN guidelines on BIA-ALCL have been recognized by the US Food and Drug Administration. Consensus guidelines have helped create a treatment standardization for BIA-ALCL at all stages of disease. NCCN guidelines are evidence-based where possible and utilize expert consensus opinion to fill in gaps that may exist. Recommendations focus on parameters for achieving reliable diagnosis and disease management and emphasize the critical role for complete surgical ablation. Suggestions for adjunct treatments and chemotherapy regimens are included for advanced BIA-ALCL with lymph node involvement.
Plastic surgeons must weigh many variables and consider all risks and benefits when selecting implants for each individual patient.
Concerns for causing malignancy in elective surgical patients have led the plastic surgery community to prioritize BIA-ALCL investigation, with numerous recent publications on the topic and the creation of a national registries in different countries313637383940. Since the first reported case in 199741, the incidence of patients with BIA-ALCL has been rapidly increasing, possibly due to an increased awareness. The U.S. Food and Drug Administration has been tracking and investigating ALCL and has released a report linking ALCL to textured implants42.
NCCN guidelines on BIA-ALCL have been recognized by the US Food and Drug Administration. Consensus guidelines have helped create a treatment standardization for BIA-ALCL at all stages of disease. NCCN guidelines are evidence-based where possible and utilize expert consensus opinion to fill in gaps that may exist. Recommendations focus on parameters for achieving reliable diagnosis and disease management and emphasize the critical role for complete surgical ablation. Suggestions for adjunct treatments and chemotherapy regimens are included for advanced BIA-ALCL with lymph node involvement.
Plastic surgeons must weigh many variables and consider all risks and benefits when selecting implants for each individual patient.
12
Future Perspective
Breast Implants of the Future
Since the introduction of the breast implants in 1962, breast augmentation has become one of the most frequently performed operations in plastic surgery. As we strive for perfect results, it is important to continue to gather and review data evaluating innovative techniques and devices43. Now we even have more options available for breast augmentation, whether we use them in combination or alone. By combining all of the available options (acellular dermal matrix products, silicone implant, fat grafting), "bioengineered breasts" can be created with high patient and surgeon satisfaction.
Biodegradable breast implants could be a novel and future approach for breast reconstruction using 3D-printed implants. Several companies are currently developing porous, biocompatible and absorbable breast scaffolds where absorbable polymer technology is used and after implantation, aims to enable regeneration of natural breast tissue. The scaffold aims to guide the growth of natural tissue with the use of patient's own body fat harvested via routinely practiced liposuction procedure and injected into the customized 3D-printed implant. Over time, this implant absorbs leaving solely the injected fat tissue in a naturally shaped breast form.
Biodegradable breast implants could be a novel and future approach for breast reconstruction using 3D-printed implants. Several companies are currently developing porous, biocompatible and absorbable breast scaffolds where absorbable polymer technology is used and after implantation, aims to enable regeneration of natural breast tissue. The scaffold aims to guide the growth of natural tissue with the use of patient's own body fat harvested via routinely practiced liposuction procedure and injected into the customized 3D-printed implant. Over time, this implant absorbs leaving solely the injected fat tissue in a naturally shaped breast form.
13
Conclusion
Conclusion
Aesthetic Augmentation is an extremely challenging but also gratifying procedure
Preoperative consult must precisely determine goals and outcomes of the patient
Several measurements are essential during preoperative evaluation, including implantbase width, IMF, N-IMF, breast implant volume, pinch and stretch test, pocket preparation and implant selection
Pay special attention to the new IMF: Be careful with lowering of the IMF because this can lead to distortion
Using a smaller implant can help to reduce the risk of fold distortion
Visualization tools such as external bra sizers, computer-generated images, and virtualreality technology can help to ensure physicians better understand their patients’ goals and expectations
The use of antibiotic and irrigation can help to reduce capsular fibrosis
Always be prepared in advance:
PREOPERATIVE PLANNING AND MARKING ARE KEY
KNOW YOUR PATIENTS AND THEIR INDIVIDUAL ANATOMIC PITFALLS
EVERY BREAST AND CHEST WALL ARE DIFFERENT, INCLUDING ASYMMETRY
14
Preoperative Checklist - Breast Implants
Preoperative Checklist - Breast Implants
Video Preoperative Markings and Sheet Preoperative Checklist Breast Implants
This video contains useful information how to perform individual preoperative planning and essential markings on a patient (breast augmentation with breast implants).
This sheet will be useful for every surgeon to quickly check the most important landmarks when it comes to optimized breast implant selection. Use it as a sheet that easily fits in your doctor´s coat´s pocket (Figure 14).
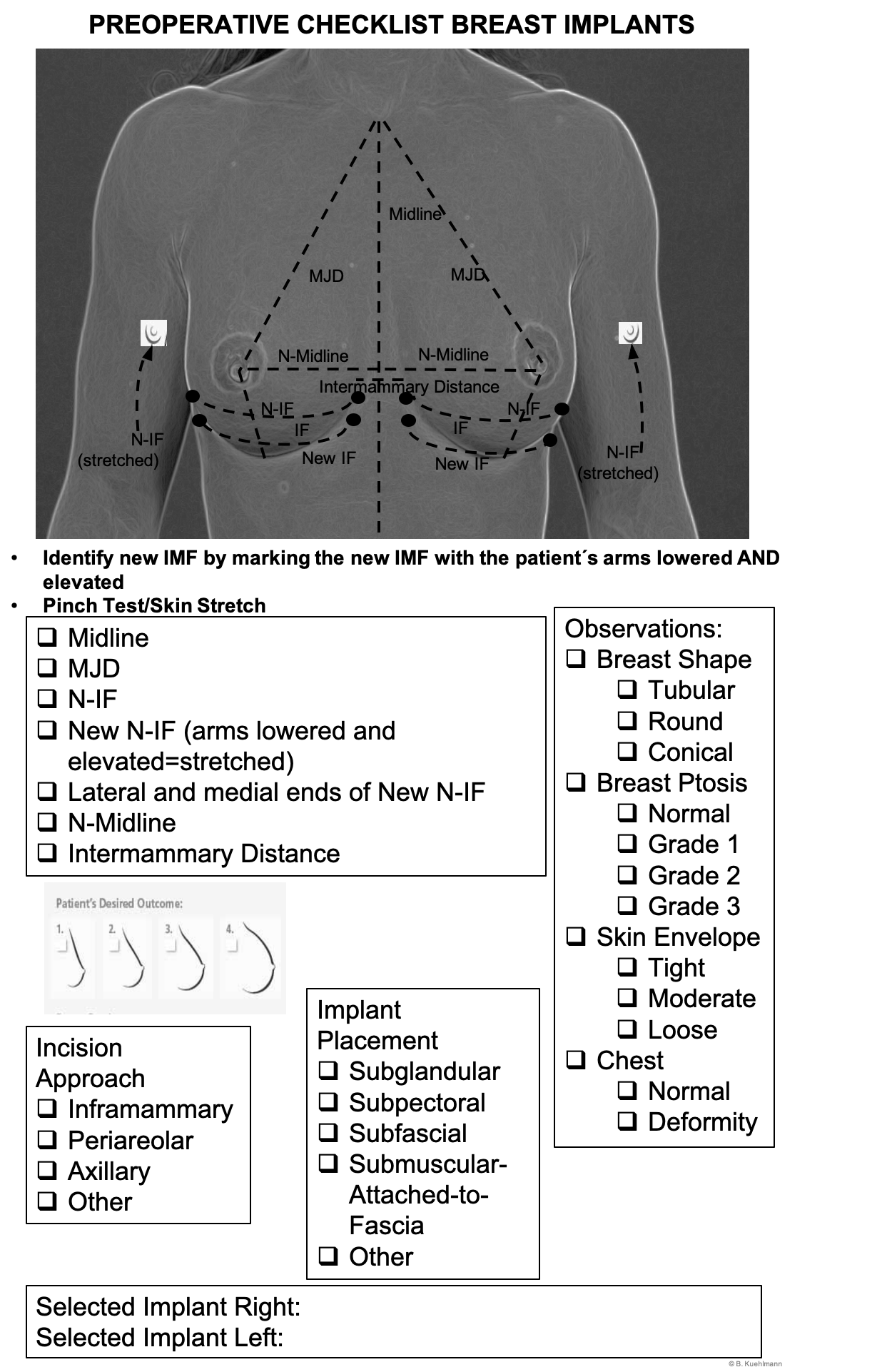
Preoperative Checklist_Breast Augmentation with Breast Implants
Images
Figure 2 Different shapes of breast implants
Figure 3 Different profiles of breast implants
Figure 4 Different surfaces of breast implants
Figure 5 45:55 ratio of ideal breast (modified after Mallucci et al., 2012., breast image: Canfield Vectra)
Figure 6 MJD: Mamille-Jugulum-Distance, UBW: Upper Breast Width, LBW: Lower Breast Width, AD: Areola Diameter, BW: Breast Width, N-MF: Nipple to Midline, N-IF: Nipple to Inframammary Fold (IFM)
Figure 7 Pinch test of upper and lower pole (a) and stretch test of the nipple (b) (Tebbetts et al., 2005)
Figure 8 Different breast implant positions
Figure 9 Superficial fascial system; sagittal view. The corpus mammae is bounded by two layers of fascia and fat (from Gilbert S; Rehnke RD, 2018.)
Figure 10 Algorithm flow chart for aesthetic breast implant augmentation (Regensburg)
Figure 11 Breast template for every breast implant augmentation –augmentation and revision
Figure 12 Diagrams of sagittal breast axis of normal IMF anatomy (above, left) where the dotted line arrow indicates the full-thickness incision of the breast tissue to reach the PM with the periareolar approach; implant positioning in a correct dissection route (above, right); double bubble characterized by the presence of a groove or indentation which creates a double convexity (below, left); and bottoming out characterized by a too lowered implant, without any double convexity and with an unaesthetic lengthening of the nipple to fold distance (below right) deformities (Salgarello et al., 2017)
Figure 13 Different types of breast that bear risks of bottoming out and doubble-bubble (Salgarello et al., 2017)
Photo Collage, Part 1
Photo Collage, Part 2
Photo Collage, Part 3
Photo Collage, Part 4
Figure 1 Algorithm for the choice of antibiotics in aesthetic breast surgery augmentation.
Preoperative Checklist_Breast Augmentation with Breast Implants
Videos
Intraoperative Checklist Incision and medial pocket
Breast Implants-Submammary incision and medial muscle release
Breast Implants Areolaplasty
Preoperative Checklist Breast Augmentation with Breast Implants
References
[1]
The statistical basis of meta-analysis, Fleiss JL, Stat Methods Med Res, 1993
[2]
Users' Guides to the Medical Literature: XXV. Evidence-based medicine: principles for applying the Users' Guides to patient care. Evidence-Based Medicine Working Group, Guyatt GH, Haynes RB, Jaeschke RZ, Cook DJ, Green L, Naylor CD, Wilson MC, Richardson WS, JAMA, 2000
[3]
Recommendations for the Use of Antibiotics in Primary and Secondary Esthetic Breast Surgery, Prantl L, Momeni A, Brebant V, Kuehlmann B, Heine N, Biermann N, Brix E, Plast Reconstr Surg Glob Open, 2020
[4]
Breast augmentation motivations and satisfaction: a prospective study of more than 3,000 silicone implantations, Gladfelter J, Murphy D, Plast Surg Nurs, 2008
[5]
Round versus Anatomical Implants in Primary Cosmetic Breast Augmentation: A Meta-Analysis and Systematic Review, Cheng F, Cen Y, Liu C, Liu R, Pan C, Dai S, Plast Reconstr Surg, 2019
[6]
Intraoperative Comparison of Anatomical versus Round Implants in Breast Augmentation: A Randomized Controlled Trial, Hidalgo DA, Weinstein AL, Plast Reconstr Surg, 2017
[7]
Volumetric Evaluation of the Mammary Gland and Pectoralis Major Muscle following Subglandular and Submuscular Breast Augmentation, Roxo AC, Nahas FX, Salin R, de Castro CC, Aboudib JH, Marques RG, Plast Reconstr Surg, 2016
[8]
Do textured breast implants decrease the rate of capsular contracture compared to smooth implants?, Cifuentes I, Dagnino B, Rada G, Medwave, 2017
[9]
Breast Implants and the Risk of Anaplastic Large-Cell Lymphoma in the Breast, de Boer M, van Leeuwen FE, Hauptmann M, Overbeek LIH, de Boer JP, Hijmering NJ, Sernee A, Klazen CAH, Lobbes MBI, van der Hulst RRWJ, Rakhorst HA, de Jong D, JAMA Oncol, 2018
[10]
Evolving Trends in Textured Implant Use for Cosmetic Augmentation in the United States, Tandon VJ, DeLong MR, Ballard TN, Clemens MW, Brandt KE, Kenkel JM, Cederna PS, Plast Reconstr Surg, 2018
[11]
Capsular contracture around saline-filled fine textured and smooth mammary implants: a prospective 7.5-year follow-up, Fagrell D, Berggren A, Tarpila E, Plast Reconstr Surg, 2001
[12]
The Science of Cohesivity and Elements of Form Stability, Gabriel A, Maxwell GP, Plast Reconstr Surg, 2019
[13]
Breast implant design, Maxwell GP, Gabriel A, Gland Surg, 2017
[14]
History of breast implants and the food and drug administration, Spear SL, Parikh PM, Goldstein JA, Clin Plast Surg, 2009
[15]
Making Sense of Implant "Profile" in Breast Augmentation, Wan D, Rohrich RJ, Plast Reconstr Surg Glob Open, 2017
[16]
Capsular contracture: what is it? What causes it? How can it be prevented and managed?, Adams WP Jr, Clin Plast Surg, 2009
[17]
In vitro and in vivo investigation of the influence of implant surface on the formation of bacterial biofilm in mammary implants, Jacombs A, Tahir S, Hu H, Deva AK, Almatroudi A, Wessels WL, Bradshaw DA, Vickery K, Plast Reconstr Surg, 2014
[18]
Ten-year review of a prospective randomized controlled trial of textured versus smooth subglandular silicone gel breast implants, Collis N, Coleman D, Foo IT, Sharpe DT, Plast Reconstr Surg, 2000
[19]
Evolving Trends in Textured Implant Use for Cosmetic Augmentation in the United States, Tandon VJ, DeLong MR, Ballard TN, Clemens MW, Brandt KE, Kenkel JM, Cederna PS, Plast Reconstr Surg, 2018
[20]
Capsular contracture around saline-filled fine textured and smooth mammary implants: a prospective 7.5-year follow-up, Fagrell D, Berggren A, Tarpila E, Plast Reconstr Surg, 2001
[21]
The evolution of breast implants, Maxwell GP, Gabriel A, Clin Plast Surg, 2009
[22]
Breast implant research: where we have been, where we are, where we need to go, Young VL, Watson ME, Clin Plast Surg, 2001
[23]
Concepts in aesthetic breast dimensions: analysis of the ideal breast, Mallucci P, Branford OA, J Plast Reconstr Aesthet Surg, 2012
[24]
Five critical decisions in breast augmentation using five measurements in 5 minutes: the high five decision support process, Tebbetts JB, Adams WP, Plast Reconstr Surg, 2005
[25]
Plastic Surgery: Volume 5: Breast, Nahabedian M, Neligan P, Elsevier, 2017
[26]
Selecting the implant height in breast augmentation with anatomical prosthesis: the "number Y", del Yerro JL, Vegas MR, Fernandez V, Moreno E, Sanz I, Puga S, Vecino MG, Biggs TM, Plast Reconstr Surg, 2013
[27]
Need for a German Breast Implant Registry - Pilot Project Breast Implant Template, Kuehlmann B, Prantl L, Handchir Mikrochir Plast Chir, 2016
[28]
Staying Out of Double-Bubble and Bottoming-Out Deformities in Dual-Plane Breast Augmentation: Anatomical and Clinical Study, Salgarello M, Visconti G, Aesthetic Plast Surg, 2017
[29]
U.S. Epidemiology of Breast Implant-Associated Anaplastic Large Cell Lymphoma, Doren EL, Miranda RN, Selber JC, Garvey PB, Liu J, Medeiros LJ, Butler CE, Clemens MW, Plast Reconstr Surg, 2017
[30]
MBN 2016 Aesthetic Breast Meeting BIA-ALCL Consensus Conference Report, Nava MB, Adams WP Jr, Botti G, Campanale A, Catanuto G, Clemens MW, Del Vecchio DA, De Vita R, Di Napoli A, Hall-Findlay E, Hammond D, Heden P, Mallucci P, Martin Del Yerro JL, Muti E, Rancati A, Randquist C, Salgarello M, Stan C, Rocco N, Plast Reconstr Surg, 2018
[31]
How to Diagnose and Treat Breast Implant-Associated Anaplastic Large Cell Lymphoma, Clemens MW, Brody GS, Mahabir RC, Miranda RN, Plast Reconstr Surg, 2018
[32]
Need for a German Breast Implant Registry - Pilot Project Breast Implant Template, Kuehlmann B, Prantl L, Handchir Mikrochir Plast Chir, 2016
[33]
Breast implant-associated anaplastic large cell lymphoma: a systematic review, Gidengil CA, Predmore Z, Mattke S, van Busum K, Kim B, Plast Reconstr Surg, 2015
[34]
Anaplastic large cell lymphoma occurring in women with breast implants: analysis of 173 cases, Brody GS, Deapen D, Taylor CR, Pinter-Brown L, House-Lightner SR, Andersen JS, Carlson G, Lechner MG, Epstein AL, Plast Reconstr Surg, 2015
[35]
The Dutch Breast Implant Registry: Registration of Breast Implant-Associated Anaplastic Large Cell Lymphoma-A Proof of Concept, Becherer BE, de Boer M, Spronk PER, Bruggink AH, de Boer JP, van Leeuwen FE, Mureau MAM, van der Hulst RRJW, de Jong D, Rakhorst HA, Plast Reconstr Surg, 2019
[36]
Australian Breast Device Registry: breast device safety transformed, Hopper I, Ahern S, Best RL, McNeil J, Cooter RD, ANZ J Surg, 2017
[37]
Breast Implant-Associated Anaplastic Large Cell Lymphoma in Australia and New Zealand: High-Surface-Area Textured Implants Are Associated with Increased Risk, Loch-Wilkinson A, Beath KJ, Knight RJW, Wessels WLF, Magnusson M, Papadopoulos T, Connell T, Lofts J, Locke M, Hopper I, Cooter R, Vickery K, Joshi PA, Prince HM, Deva AK, Plast Reconstr Surg, 2017
[38]
Anaplastic T-cell lymphoma in proximity to a saline-filled breast implant, Keech JA Jr, Creech BJ, Plast Reconstr Surg, 1997
[39]
US FDA Breast Implant Postapproval Studies: Long-term Outcomes in 99,993 Patients, Coroneos CJ, Selber JC, Offodile AC 2nd, Butler CE, Clemens MW, Ann Surg, 2019
[40]
Possible future development of implants and breast augmentation, Maxwell GP, Gabriel A, Clin Plast Surg, 2009