["18952ef1cbdccf0cbb8e5a4952a65eee68d20ce3","8fd1f5b2498973137139e086c070361db55230aa","b0ab6e5115bfe017e3e5c8db4af9ff8793a02316"]
Eyelid surgery
blepharoplasty
periorbital
eyelid
oculoplastic
ophthalmic plastic surgery
8411
8411
Chapter reads
3
3
Chapter likes
7/10
Evidence score
03
3
Images included
07
7
Videos included
01
An Evidence-based approach to blepharoplasty
AN EVIDENCE-BASED APPROACH TO BLEPHAROPLASTY
There is little high level evidence in blepharoplasty literature. A literature search of PubMed, Medline and Cochrane libraries was performed to obtain the best available evidence on blepharoplasty, with emphasis on studies regarding attractiveness of the eye.
Evidence on the “ideal or attractive eye”
“Beauty is in the eye of the beholder” may be true in certain circumstances, but there is evidence that many attributes of beauty are intuitive and unlearned reference01reference02. Eyes are considered among the most attractive facial elements in women and men and are also among the first features to show signs of aging reference03reference04. Early approaches to assess physical attractiveness were done by measuring specific distances in faces, having these faces rated for attractiveness and comparing the facial distances to these ratings. With a focus on the eye and periorbita as a whole, studies have shown that a positive canthal tilt is considered attractive in both men and women, with the lateral canthus positioned slightly superior to the medial canthus reference07. The angle of this tilt is slightly increased in women, at 2° to 4°, compared with men at 1° to 2°, and is considered a hallmark of a beautiful eyereference08. There is also a strong correlation between the attractiveness of the eye and age. The younger a person’s eye, the more beautiful it is perceived. Other authors have also described correlations between eye form and perceived age; reference09reference10reference11 the youthful eye is apparently characterized by a long narrow palpebral fissure or an “almond-shaped” eye form. Large eyes have been mentioned in many studies as traits of “babyness” reference12reference13. Consistent with these theories the lateral eye angle is also correlated with attractiveness and youth. The larger the angle the more attractive is the eye.reference12 The upper eyelid is full in youth, without sagging or bulging of tissues. In Caucasians, the upper lid has a well-defined supratarsal crease, typically 7 to 10 mm from the palpebral margin reference08. The notion of an attractive upper lid has changed significantly over the past decades. Contrary to the traditional perception of attractiveness with a high lid crease and a deep hollow sulcus, Fagien points out the importance of a lower upper eyelid crease in combination with volume preservation in order to achieve a youthful appearance reference10. The arc of the upper lid has its peak on the medial aspect of the lid in the youthful face in both men and women reference14.There is less variation in the ideal lower lid. In youth, the lower lid is typically inconspicuous, it is with age that the lower lid lengthens, and pseudoherniation of fat appears, drawing unwanted attention to this facial feature. The information regarding attractiveness obtained from clinical studies conducted under controlled settings, e.g. attractiveness ratings, age estimations etc., seem to have enormous relevance for proper planning of surgical interventions. But without undermining the scientific base of periorbital surgery, the age, race, gender and desires of the particular patient have to be considered.
02
Local anatomy
Local anatomy
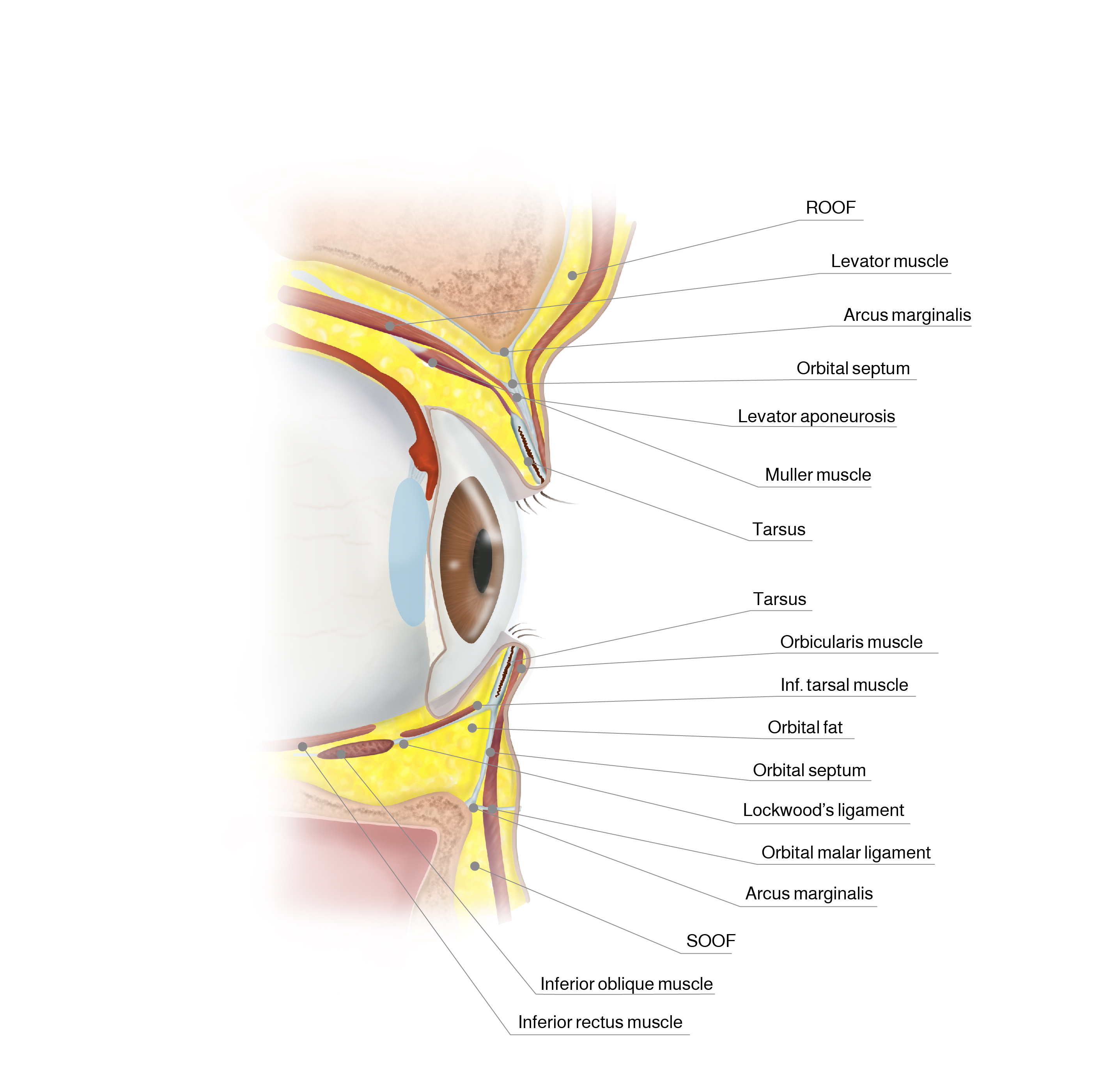
Transverse section of the eye
The upper and the lower eyelids are composed of three lamellae. In transcutaneous blepharoplasty the first structure to be incised is the anterior lamella. It is composed of skin and orbicularis muscle. The orbicularis muscle is divided into pretarsal, preseptal and periorbital areas based on the underlying structures. The tarsal plate gives vertical support to the respective eyelid. The retractors of the lids insert in the respective tarsal plates and constitute the posterior lamella together with the conjunctival inner lining of the lid, fornix and eye globe. The anterior and posterior lamellae merge on the tarsus. In between is the middle lamella with the orbital septum which is a fibrous membrane that covers the periorbital fat. The arcus marginalis is the insertion of the orbital septum onto the osseous orbital rim.
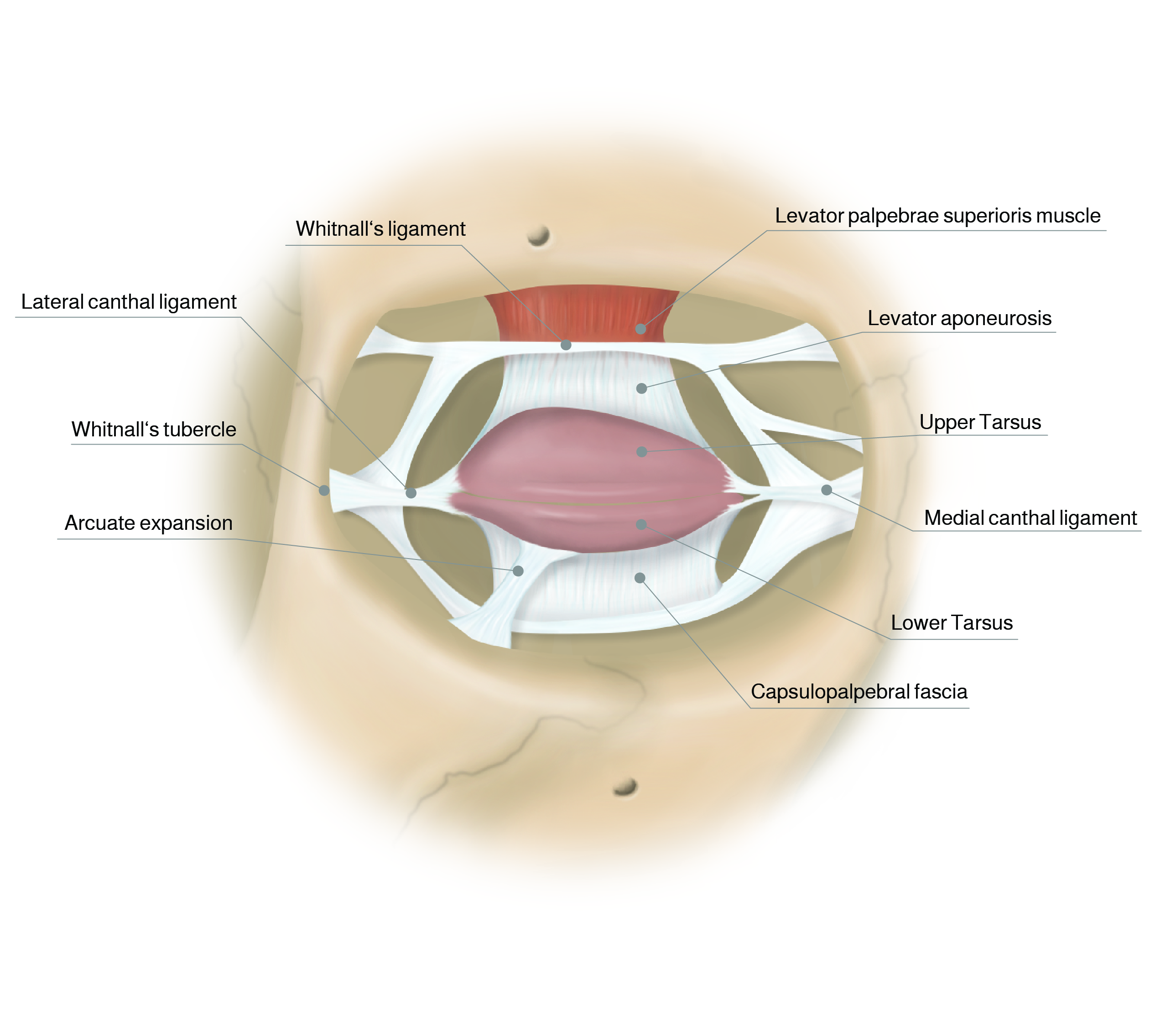
Ligaments and tendons of the eye
Upper lid elevation is possible due to the voluntary levator palpebrae superioris muscle and the Mueller’s muscle (inervated by the sympathetic nervous system). The levator muscle inserts in the apex of the orbit in the lesser wing of the sphenoid bone and after crossing the orbita horizontally changes to a vertical direction at Whitnall’s ligament fanning out into the levator aponeurosis.
Whitnall’s ligament runs horizontally and connects the trochlea medially with Whitnall’s tubercle laterally, dividing the lacrimal gland into palpebral and orbital lobes.
The levator aponeurosis has two distinct layers reference19. The anterior layer inserts on the orbital septum, the posterior layer inserts onto the tarsal plate and the subcutaneous tissue. The supratarsal crease is created by the fusion of the levator aponeurosis with the orbital septum and the insertion of the fascia of the orbicularis oculi into the dermis reference11.
The medial and lateral canthal tendons suspend the tarsal plates in the orbit. The lateral canthal tendon (LCT) can be separated into a superficial and a deep component. The anterior reflection of the lateral canthal tendon inserts on the anterior surface of the lateral orbital rim and the orbital raphe. The posterior reflection is the main lateral canthal tendon, which inserts on Whitnall’s tubercle and consists of a superior and inferior crus. Superiorly, the lateral canthal tendon is contiguous with the lateral horn of the levator aponeurosis.
In the upper lid the nasal and central (preaponeurotic) fat compartments are separated by the superior oblique muscle and the interpad septum. The nasal fat pad contains fat that has a distinctly white color when compared to the other fat compartments of the eyelid.
The lower eyelid contains three postseptal fat compartments. These are the nasal, central, and lateral fat pads. The inferior oblique muscle separates the nasal and central fat pads. The central and lateral fat pads are separated by the arcuate expansion, a thickening in the orbital septum.
Under the orbicularis muscle overlying periosteum is a plane of nonseptate fat called the suborbicularis oculi fat (SOOF). This fat is analogous to the superiorly located retro-orbicularis oculi fat (ROOF), which is situated under the eyebrow.
The Tear Trough, also referred to as the nasojugal groove, is created by the attachment of the orbital retaining ligament, or orbital malar ligament, to the skin. This ligament originates from the inferior orbital rim and runs from the medial canthus to the medial corneoscleral limbus.
The motor nerve supply to the upper eyelids is from the buccal, zygomatic, and frontal branches of the facial nerve.
Whitnall’s ligament runs horizontally and connects the trochlea medially with Whitnall’s tubercle laterally, dividing the lacrimal gland into palpebral and orbital lobes.
The levator aponeurosis has two distinct layers reference19. The anterior layer inserts on the orbital septum, the posterior layer inserts onto the tarsal plate and the subcutaneous tissue. The supratarsal crease is created by the fusion of the levator aponeurosis with the orbital septum and the insertion of the fascia of the orbicularis oculi into the dermis reference11.
The medial and lateral canthal tendons suspend the tarsal plates in the orbit. The lateral canthal tendon (LCT) can be separated into a superficial and a deep component. The anterior reflection of the lateral canthal tendon inserts on the anterior surface of the lateral orbital rim and the orbital raphe. The posterior reflection is the main lateral canthal tendon, which inserts on Whitnall’s tubercle and consists of a superior and inferior crus. Superiorly, the lateral canthal tendon is contiguous with the lateral horn of the levator aponeurosis.
In the upper lid the nasal and central (preaponeurotic) fat compartments are separated by the superior oblique muscle and the interpad septum. The nasal fat pad contains fat that has a distinctly white color when compared to the other fat compartments of the eyelid.
The lower eyelid contains three postseptal fat compartments. These are the nasal, central, and lateral fat pads. The inferior oblique muscle separates the nasal and central fat pads. The central and lateral fat pads are separated by the arcuate expansion, a thickening in the orbital septum.
Under the orbicularis muscle overlying periosteum is a plane of nonseptate fat called the suborbicularis oculi fat (SOOF). This fat is analogous to the superiorly located retro-orbicularis oculi fat (ROOF), which is situated under the eyebrow.
The Tear Trough, also referred to as the nasojugal groove, is created by the attachment of the orbital retaining ligament, or orbital malar ligament, to the skin. This ligament originates from the inferior orbital rim and runs from the medial canthus to the medial corneoscleral limbus.
The motor nerve supply to the upper eyelids is from the buccal, zygomatic, and frontal branches of the facial nerve.
03
Anatomic key structures of the periorbita and their changes with age
Anatomic key structures of the periorbita and their changes with age
Despite its universality, facial aging is still not well understood. In an effort to create statistically significant visual representations of facial aging, Lambros analyzed comparative three-dimensional image transitions of young and old faces. Among the myriad changes visible in these images are the narrowing of the eyelid aperture. The lateral canthal angle moves medially, and the upper and lower lid approach each other. The average lower lid rises slightly with age. The net effect is to reduce the size of the medial and lateral scleral triangles, thus diminishing the eyelid aperture and making the eyes look smaller. reference22
Furthermore, with age, the eyelid skin loses its elasticity, the dermis becomes atrophic, wrinkles, rhytids or pigmentary changes appear reference23. The orbital septum weakens and some fat protrusion may occur into the lids. The levator aponeurosis may become attenuated, stretch and lose its firm attachment to the tissues of the upper lid, especially to the tarsal plate, resulting in ptosis. The supratarsal crease often migrates caphalad as the eye ages reference25. Regarding the lower lid Fezza and Massry showed that for each decade, there was an almost linear increase in lower lid length. The average 20 year old lower lid almost doubles its length when becoming 90 year old reference15reference16. The descent of the visible lid–cheek junction occurs primarily as a result of the descent of the midfacial soft tissues and the malar fat pad, causing a visibly longer lower lid. reference03Bone loss in the periorbital and malar regions contributes to the overall volume loss associated with aging and loss of projection of the orbital rim reference17. In addition, Oh and Colleagues showed that in patients >70 years of age, the medial fat pad becomes prominent whereas the central fat pad atrophies reference24. This is the driving factor in the hallowed look of the superior periorbital region. Thus, camouflaging the lid–cheek junction and creating the appearance of a shorter lid gives the appearance of a youthful lid. Additional changes secondary to aging can include ectropion, lagophthalmos, and dermatochalasis.
Furthermore, with age, the eyelid skin loses its elasticity, the dermis becomes atrophic, wrinkles, rhytids or pigmentary changes appear reference23. The orbital septum weakens and some fat protrusion may occur into the lids. The levator aponeurosis may become attenuated, stretch and lose its firm attachment to the tissues of the upper lid, especially to the tarsal plate, resulting in ptosis. The supratarsal crease often migrates caphalad as the eye ages reference25. Regarding the lower lid Fezza and Massry showed that for each decade, there was an almost linear increase in lower lid length. The average 20 year old lower lid almost doubles its length when becoming 90 year old reference15reference16. The descent of the visible lid–cheek junction occurs primarily as a result of the descent of the midfacial soft tissues and the malar fat pad, causing a visibly longer lower lid. reference03Bone loss in the periorbital and malar regions contributes to the overall volume loss associated with aging and loss of projection of the orbital rim reference17. In addition, Oh and Colleagues showed that in patients >70 years of age, the medial fat pad becomes prominent whereas the central fat pad atrophies reference24. This is the driving factor in the hallowed look of the superior periorbital region. Thus, camouflaging the lid–cheek junction and creating the appearance of a shorter lid gives the appearance of a youthful lid. Additional changes secondary to aging can include ectropion, lagophthalmos, and dermatochalasis.
04
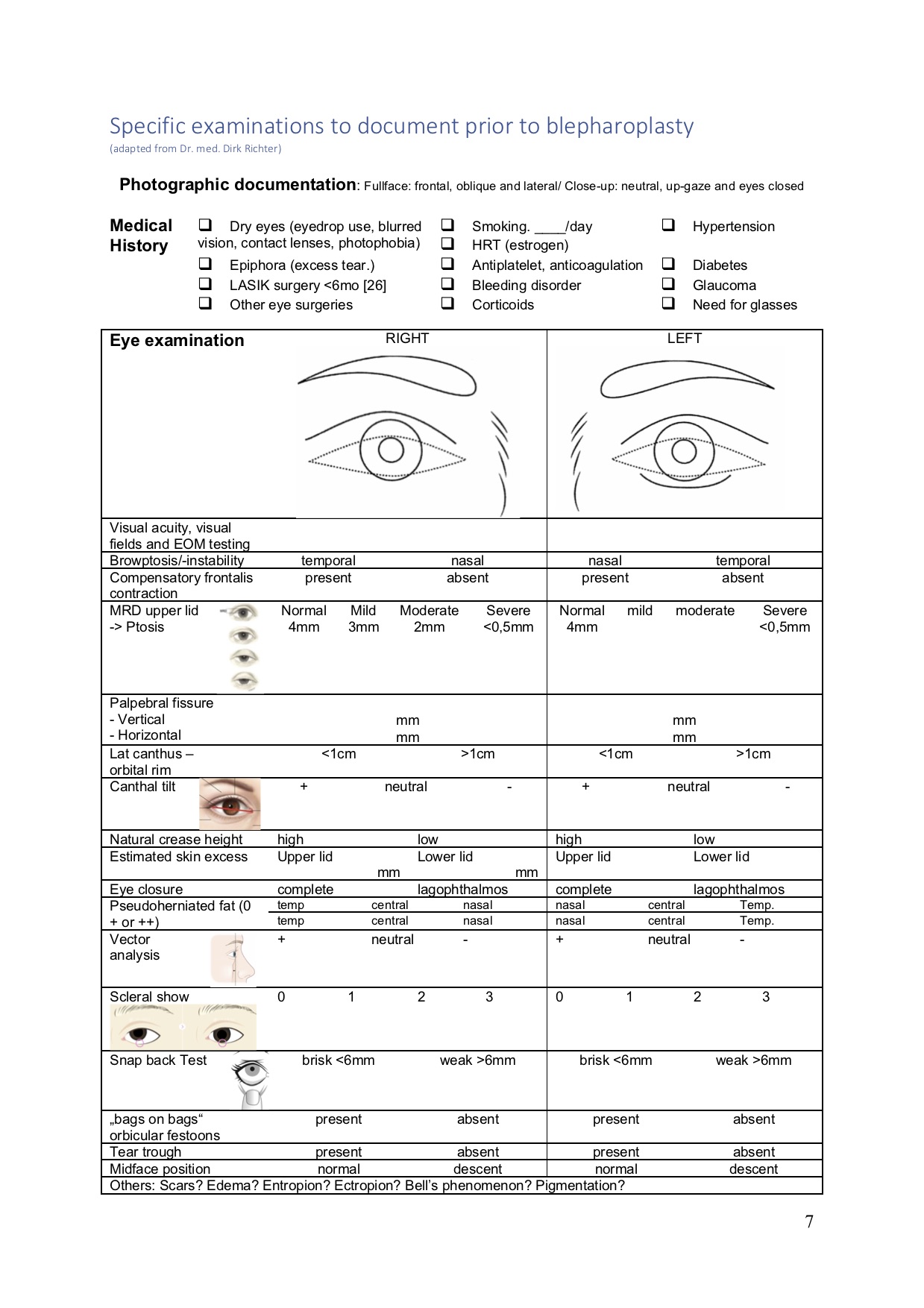
Specific examinations to document prior to blepharoplasty
05
Upper lid blepharoplasty in 5 steps
Upper lid blepharoplasty in 5 steps
1. Skin Markings
Lower incision/ eyelid crease mark
The patient is marked in an upright position. While fixing the eyebrow in the right position, first the eyelid crease mark is drawn in the midpupil line, in women, between 7 and 10 mm, in men 5–8 mm above the lash line. The line is completed laterally and medially following the arc of the lid crease. Laterally, this incision takes a lazy-S–shaped course, falling into a lateral orbital skin crease, to allow greater skin excision of the lateral upper lid, where most of the redundancy is found.
Upper incision/ estimating skin excess
Measuring the skin to be retained:
The superior mark is made by following the natural contour of the (natural, not plucked) brow paralleling the lower incision while keeping the mark at least 10 mm below the inferior edge of the brow hairs. This line is generally located at the juncture of the thick and thin skin of the upper lid. Flowers suggests that at least 20 mm of skin are needed between the eyebrow and lid margin to allow comfortable eyelid closure. reference27
This can be confirmed by measuring the skin to be removed, performing a “skin-pinch-technique” by placing the nontooth forceps based at the lower incision and gently pinch together the eyelid skin till slight eversion of the eyelashes is noted.
The superior mark is made by following the natural contour of the (natural, not plucked) brow paralleling the lower incision while keeping the mark at least 10 mm below the inferior edge of the brow hairs. This line is generally located at the juncture of the thick and thin skin of the upper lid. Flowers suggests that at least 20 mm of skin are needed between the eyebrow and lid margin to allow comfortable eyelid closure. reference27
This can be confirmed by measuring the skin to be removed, performing a “skin-pinch-technique” by placing the nontooth forceps based at the lower incision and gently pinch together the eyelid skin till slight eversion of the eyelashes is noted.
2. Anesthesia
Upper Blepharoplasty is typically performed under local anesthesia or monitored care anesthesia with local injection using a mixture of 1% lidocaine with epinephrine of 1:100,000 concentration, taking care of injecting equal volumes on both sides (usually 3cc) performing a thorough subcutaneous hydrodissection reference28. The local anesthetic should be injected superficially from laterally to medially in order to avoid any subcutaneous or intraorbicularis hematoma formation.
+/- Hyaluronidase (Wydase) (0.1 to 10 ml of local anesthetic) may also be added to help diffuse the local anesthetic through the subcutaneous layer.
+ /- Sodium bicarbonate can be added to the injection to buffer the pH and to avoid burning pain• Additionally, later when addressing the fat compartments the fat pads can be directly injected under direct vision after the septum is opened.
+/- Hyaluronidase (Wydase) (0.1 to 10 ml of local anesthetic) may also be added to help diffuse the local anesthetic through the subcutaneous layer.
+ /- Sodium bicarbonate can be added to the injection to buffer the pH and to avoid burning pain• Additionally, later when addressing the fat compartments the fat pads can be directly injected under direct vision after the septum is opened.
3. Excision of excess skin and orbicularis muscle
Many instruments are available to perform the skin/muscle incision, including the traditional scalpel, scissors, electrocautery (Colorado needle), radiofrequency devices, and carbon dioxide (CO2) or YAG lasers.
The marked skin is removed and the orbicularis muscle is exposed. The excision of the orbicularis muscle occurs only laterally, nasally the orbicularis is just incised exposing the orbital septum, which is left intact.
The preseptal orbicularis is adherent to the septum, and careful dissection in the proper submuscular plane is required.
4. Management of fat
Exposure of the central and nasal fat pads is accomplished by making small incisions in the orbital septum and applying gentle pressure on the globe. By this means the fat pads will prolapse through the windows and can be excised or sculpted.
There is a separate area of fat between the yellow central fat and the whiter nasal fat. This junctional fat invests the septum and extension of Whitnall’s ligament that forms the interpad septum. The interpad septum and junctional fat should be left intact to avoid an A-frame deformity.
ROOF fat is dense fat behind the orbicularis muscle, not as easy coming out as the preaponeurotic fat and if prolapsing can be excised especially laterally.
The lacrimal gland can be identified by its paler color, generally light pinkish-brown; lateral location; and its firmer texture. If it is prolapsed, the gland can be repositioned into the lacrimal fossa or sutured to the periosteum inside the orbital rim with non-absorbable suture. Alternatively Whitnall’s ligament can be sutured to the periosteum strengthening the septal support to the lacrimal gland.
Care should be taken to avoid pulling on the fat as it can be uncomfortable for the patient and often has intertwined vessels within the pad that may bleed on excessive manipulation.
5. Reconstruction of eyelid crease and skin closure
Fixation of the orbicularis muscle to the levator aponeurosis using 2-3 absorbable sutures (usually 6-0 Monocryl) in its central, temporal and nasal position is performed in order to form the eyelid crease and to prevent postoperative ptosis.The skin is closed with running subcuticular suture (Prolene 6-0) reference29.
Postoperative treatment
- Patients are carefully observed for 2 to 3 hours, with cold compresses on the eye area, to ensure that no bleeding symptoms arise. reference30
- After that cold compresses may be applied to the closed lids for 48h to reduce edema.
- Adequate analgesia reduces the risk of postoperative bleeding by avoiding peaks in blood pressure.
- Head elevation to reduce edema.
- Patients are asked to avoid significant physical activity for 1 week to limit postoperative edema and ecchymosis.
- Nonabsorbable sutures are removed at 5-7 days.
- Lubricant eye drops are prescribed to reduce any dryness of the eyes during the first 2 or 3 weeks (3 times per day)
- After that cold compresses may be applied to the closed lids for 48h to reduce edema.
- Adequate analgesia reduces the risk of postoperative bleeding by avoiding peaks in blood pressure.
- Head elevation to reduce edema.
- Patients are asked to avoid significant physical activity for 1 week to limit postoperative edema and ecchymosis.
- Nonabsorbable sutures are removed at 5-7 days.
- Lubricant eye drops are prescribed to reduce any dryness of the eyes during the first 2 or 3 weeks (3 times per day)
Ancillary procedures
- Direct browpexy: To avoid resulting eyebrow ptosis or to achieve a discreet brow lift, the sub-brow dermis is fixed to the periosteum or frontalis muscle about 1-2 cm above the upper edge of the orbit with a PDS 5-0 suture.
- Transpalpebral corrugator supercili resection
- Ptosis repair -> levator advancement
- Lipofilling e.g. the eyebrow region. (CAVE A./N. supratrochlearis)
- Canthopexy: see below
- Transpalpebral corrugator supercili resection
- Ptosis repair -> levator advancement
- Lipofilling e.g. the eyebrow region. (CAVE A./N. supratrochlearis)
- Canthopexy: see below
Although very uncommon, vision loss due to retrobulbar hematoma is the most feared complication resulting from upper lid blepharoplasty. This complication can be prevented by avoiding traction on the orbital fat during fat excision and by careful hemostasis. A serious hematoma occurring during the hours following surgery should be evacuated by reopening the lid.
06
Lower lid blepharoplasty
Lower lid blepharoplasty
There are two main approaches to lower lid blepharoplasty:
The transconjunctival approach is preferred for young patients who have minimal aging changes and little cheek descent and for patients who have a negative vector with a higher risk of postoperative ectropion.
The transcutaneous approach allows for greater re-draping of the orbicularis muscle and more significant improvement in the laxity of the lower eyelid. Both the transconjunctival and transcutaneous surgical approaches are equally effective in addressing fat (resection and/or redistribution), but the transconjunctival route alone does not in general provide adequate exposure to the mid face and does not allow appropriate cephalic and lateral elevation of the cheek unit.
The transconjunctival approach is preferred for young patients who have minimal aging changes and little cheek descent and for patients who have a negative vector with a higher risk of postoperative ectropion.
The transcutaneous approach allows for greater re-draping of the orbicularis muscle and more significant improvement in the laxity of the lower eyelid. Both the transconjunctival and transcutaneous surgical approaches are equally effective in addressing fat (resection and/or redistribution), but the transconjunctival route alone does not in general provide adequate exposure to the mid face and does not allow appropriate cephalic and lateral elevation of the cheek unit.
Transcutaneous lower lid blepharoplasty
1. Skin marking
The lower lid incision is placed in the infraciliary groove approximately 2-3 mm inferior to the eye lashes/lid margin. It begins 3-5 mm lateral to the inferior punctum and extends 8 to 10 mm lateral to the lateral canthus tailored into one of the existing wrinkles. In case of much skin excess, the lateral extension can be prolonged further and although marked obliquely the resulting wound will end up horizontally after the redundant skin is excised. If upper blepharoplasty is also planned, 8 to 10 mm of intact skin should exist between the two markings to prevent lymphatic flow obstruction. The orbital rim is marked with a dotted line, the course of the infraorbital nerve and Whitnall’s tubercle are marked as we.
2. Anesthesia
Protective contact lenses are placed bilaterally (metal if working with laser, and plastic if electrocautery is used). Local anesthesia with vasoconstrictor is injected in a subcutaneous, premuscular plane along the infraciliary incision line. If canthopexy/canthoplasty is planned, additional local anesthesia should be injected along the lateral and inferior orbital rim.
3. Suspension suture and incision
The eyelid is temporary suspended with a 5-0 prolene suture. The incision is made starting laterally with a no. 15 surgical blade in the previous surgical marking. Then a tenotomy scissor is used to first carefully undermine the thin skin from laterally to medially in a subcutaneous plane before incising it.
After the skin incision is completed, the pretarsal and preseptal aspects of the orbicularis muscle are exposed and incised. In its lateral aspect a small submuscular approach through the orbicularis is created. Tenotomy scissors are inserted and by spreading submuscularly towards the middle a submuscular pocket is created preserving the integrity of orbicularis. By beveling the pair of scissors orienting it in an oblique fashion the muscle fibres are now cut. This ensures a generous 5 mm-6mm strip of pretarsal muscle is preserved on the lower eyelid which adds to stablization of the lid.
After the skin incision is completed, the pretarsal and preseptal aspects of the orbicularis muscle are exposed and incised. In its lateral aspect a small submuscular approach through the orbicularis is created. Tenotomy scissors are inserted and by spreading submuscularly towards the middle a submuscular pocket is created preserving the integrity of orbicularis. By beveling the pair of scissors orienting it in an oblique fashion the muscle fibres are now cut. This ensures a generous 5 mm-6mm strip of pretarsal muscle is preserved on the lower eyelid which adds to stablization of the lid.
4. Development of a myocutaneous flap
After insertion retractors the dissection continues inferiorly developing the skin-muscle flap further with the bipolar coagulation dividing the flap away from the orbital fat down to the level of the orbital rim.
5. Division of the orbitomalar ligament (OML) and preperiosteal dissection
Once the orbital rim is reached, the orbitomalar ligament is identified and incised along the entire orbital rim superficially to the periosteum. The dissection proceeds inferiorly below the orbital rim in a preperiosteal plane until the SOOF is visible.
6. Levator labii superioris alaeque nasi muscle
The levator labii and nasi muscle is released using bipolar coagulation in order to correct the tear trough deformity.
This muscle has the longest name of all the muscles in the body. As the name indicates it elevates the upper lip and the nostrils.
7. Septal incision
The orbital septum is incised horizontally along the entire extent of the eyelid starting from medially, which allows the redundant orbital fat to bulge into the field.
Care is taken to avoid the inferior oblique muscle, especially in revision surgery, as it passes between the medial and central fat compartments and serves as an important surgical landmark.
8. Management of fat
Excision of fat
Marked excess fat can be excised. The central fat pad often herniates through the incision and is addressed first, then the medial pad, taking care to avoid injury to the inferior oblique muscle. Partial resection of the central fat may improve identification of the medial fat, which appears whiter and more fibrous than the central and lateral fat, which appears yellow and softer. Finally, the lateral fat compartment is addressed.
Release at the arcus marginalis and septal reset (= fat redraping)
Moderate or mild fat prolapse (or the residual fat after reduction) may be redraped to fill the hollows along the inferior orbital rim or the nasojugal fold (“tear trough”). Medial and central fat is advanced, the medial fat is secured under the the levator labii superioris muscle and to the periosteum with multiple interrupted Monocryl 5-0 sutures. The result is a smooth contour that obscures the infraorbital rim and resembles the contour of youth. Compared with fat grafting, transposed orbital fat is much more predictable and also has a 100% survival rate, as it remains attached to the blood supply in the form of a pedicled vascularized flap.
9. Canthopexy or canthoplasty
Canthopexy or canthoplasty should be considered on most patients who undergo lower blepharoplasty using a 5-0 PDS suture. It reduces the need to resect skin that in truth is not excessive, but appears so owing to dropped lid posture from lid laxity and loss of tone.reference31 A graded approach is adopted, but regardless of the procedure the canthus should always be anchored inside the orbital rim, not at the edge, allowing the lid to conform to the globe.
- Mild horizontal laxity -> Canthopexy = plication suture (5-0 PDS suture introduced through an incision at the lateral canthus and secured to the lateral orbital rim)
- Marked laxity -> Tarsal strip
- Marked laxity with significant canthal migration -> relocation of the whole lateral canthal tendon on the lateral orbital rim = Canthoplasty = resection of a redundant block of tarsal plate or formation of a strip of tarsus from the redundant lid or anchorig the tarsus via drill hole the lateral orbital rim.
- Mild horizontal laxity -> Canthopexy = plication suture (5-0 PDS suture introduced through an incision at the lateral canthus and secured to the lateral orbital rim)
- Marked laxity -> Tarsal strip
- Marked laxity with significant canthal migration -> relocation of the whole lateral canthal tendon on the lateral orbital rim = Canthoplasty = resection of a redundant block of tarsal plate or formation of a strip of tarsus from the redundant lid or anchorig the tarsus via drill hole the lateral orbital rim.
10. Skin-muscle flap suspension
If the palpebral tone was found to be normal or slightly diminished during the preoperative evaluation, the orbicularis oculi muscle is suspended to the lateral orbital rim. Suspension of the muscle yields better tone to the skin-muscle flap, which decreases eyelid rhytids and decreases the likelihood of retraction, scleral exposure, and ectropion. This suspension also lifts the dropped SOOF.
11. Skin resection
The amount of skin resection depends of the redraped fat. In case of a stabile canthopexy and skin muscle flap suspension the excess laterally can be excised more generously.
11. Closure
The septum does not need to be closed. Closure is then performed with interrupted Prolene 6-0 sutures laterally and the remaining skin with intradermal sutures (Prolene 5-0).
The main complications following lower lid blepharoplasty are ectropion, lid retraction or scleral show. These occur if too much skin is removed or if there is uncorrected horizontal lid laxity. They are prevented by adding a canthopexy/-plasty to the procedure. A correction is not recommended in the first 6 months after the surgery as the ectropion often recovers when the muscle is adequately innervated again.
Patients should also be informed that dry eye, chemosis, and tearful eyes will disappear within 3 months after transcutaneous lower blepharoplasty, which may boost patient satisfaction and confidence reference32
Transconjunctival blepharoplasty
Alternatively, a lower blepharoplasty can be performed using a transconjunctival incision.
1. Anesthesia
See also upper/transcutaneous blepharoplasty part. Retract the lower lid and inject 1% lidocaine with 1:100,000 adrenaline deep to the conjunctiva along the proximal border of the tarsal plate. reference28
2. Incision
The lower lid is everted using small retractors. The incision is made approximately 8 mm posterior to the eyelid margin, 1-2 mm below the inferior border of the tarsal plate. The incision is made directly into the fat compartment in a perpendicular manner to avoid the inferior oblique muscle. Pressure is applied to the globe causing the fat of the lower lid to balloon in the fornix.
3. Fat management
The closer each fat compartment is opened to the orbital rim, the easier the exposure and the less chance of encountering bleeding or damage to the inferior oblique muscle
4. Closure
It is not necessary to close the conjunctiva or the fascia if a small incision is made or two separate incisions are made; if a single incision is made all along the eyelid, suture closure prevents malaligned healing of conjunctival edges.
The most common complication following transconjunctival blepharoplasty is inadequate or asymmetrical fat prolapse. Lower eyelid retraction is less common than with the skin approach because no skin is excised and the septum is not damaged during the procedure. Damage to the inferior oblique muscle is uncommon although transient weakness may occur.
Ancillary procedures
Lateral canthal anchoring is integral to both transconjunctival and standard transutaneous lower lid blepharoplasty.
Extended midface blepharoplasty: Reposition of the malar fat and the SOOF in the lower and lateral orbital rim through midface subperiosteal dissection.
Skin-only blepharoplasty (pinch blepharoplasty): this techniques preserves the orbital septum as the fat is harvested from the transconjunctival approach
Tissue augmentation techniques include fat transposition, autologous fat transfer, and injection of hyaluronic acid or other fillers.
Autologous PRP treatment (platelet-rich plasma): enhances some parameters associated with healing properties, suggesting a potential therapeutic value after blepharoplasty surgeryreference33
Skin resurfacing: Laser, chemical peel (caution because of the high risk of full-thickness burns and ectropion)
Images
Transverse section of the eye
Ligaments and tendons of the eye
Specific examinations to document prior to blepharoplasty
Videos
Preoperative Examination
Lower lid blepharoplasty skin markings
Upper lid blepharoplasty skin markings
Upper lid blepharoplasty, internal browpexy and lipofilling
Upper lid blepharoplasty
Lower lid blepharoplasty
Lower Lid Blepharoplasty, Midface Lift and Canthopexy
References
[1]
Preference for attractive faces in human infants extends beyond conspecifics, Quinn, P.C., et al.,, Dev Sci, 2008
[2]
Infant preferences for attractive faces : Rudiments of a stereotype, Langlois , J.H., et al., Developmental Psychology, 1987
[3]
Ideal Facial Relationships and Goals, Bueller, H., Facial Plast Surg, 2018
[4]
Filtered beauty in Oslo and Tokyo: A spatial frequency analysis of facial attractiveness, Overvoll, M., et al., PLoS One, 2020
[5]
Brow/Upper lid anatomy, aging and aesthetic analysis, Branham, G. and J.B. Holds, Facial Plast Surg Clin North Am, 2015
[6]
Upper blepharoplasty: the aesthetic ideal, Pepper, J.P. and J.S. Moyer, Clin Plast Surg, 2013
[7]
Preoperative evaluation of the blepharoplasty patient. Bypassing the pitfalls, Jelks, G.W. and E.B. Jelks, Clin Plast Surg, 1993
[8]
Advanced rejuvenative upper blepharoplasty: enhancing aesthetics of the upper periorbita, Fagien, S., Plast Reconstr Surg, 2002
[9]
Current concepts in aesthetic upper blepharoplasty., Rohrich, R.J., et al., Plast Reconstr Surg, 2004
[10]
Female eye attractiveness - Where beauty meets science, Prantl, L., J Craniomaxillofac Surg, 2019
[11]
Darwinian aesthetics: sexual selection and the biology of beauty, Grammer, K., et al., Biol Rev Camb Philos Soc, 2003
[12]
Female eye attractiveness - Where beauty meets science, Prantl, L., J Craniomaxillofac Surg, 2019
[13]
Upper blepharoplasty: the aesthetic ideal, Pepper, J.P. and J.S. Moyer, Clin Plast Surg, 2013
[14]
Advanced rejuvenative upper blepharoplasty: enhancing aesthetics of the upper periorbita, Fagien, S., Plast Reconstr Surg, 2002
[15]
Observations on periorbital and midface aging, Lambros, V., Plast Reconstr Surg, 2007
[16]
Facial Aging: A 54-Year, Three-Dimensional Population Study, Lambros, V.,, Plast Reconstr Surg, 2020
[17]
A Dual Approach to Understanding Facial Perception Before and After Blepharoplasty, Bater, K.L., et al., JAMA Facial Plast Surg, 2018
[18]
Eyebrow and eyelid dimensions: an anthropometric analysis of African Americans and Caucasians, Price, K.M., et al., Plast Reconstr Surg, 2009
[19]
Lower Eyelid Length, Fezza, J.P. and G. Massry, Plast Reconstr Surg, 2015
[20]
Composite rhytidectomy, Hamra, S.T., Plast Reconstr Surg, 1992
[21]
Ideal Facial Relationships and Goals, Bueller, H., Facial Plast Surg, 2018
[22]
Relative maxillary retrusion as a natural consequence of aging: combining skeletal and soft-tissue changes into an integrated model of midfacial aging, Pessa, J.E., et al.,, Plast Reconstr Surg, 1998
[23]
Analysis of eyelid fat pad changes with aging, Oh, S.R., et al., Ophthalmic Plast Reconstr Surg, 201
[24]
Precision planning in blepharoplasty. The importance of preoperative mapping, Flowers, R.S. and S.S. Flowers, Clin Plast Surg, 1993
[25]
A randomised double-blinded crossover study comparing pain during anaesthetising the eyelids in upper blepharoplasty: First versus second eyelid and lidocaine versus prilocaine, Pool, S.M., M.M. Struys, and B. van der Lei, J Plast Reconstr Aesthet Surg, 2015
[26]
Improved upper blepharoplasty outcome using an internal intradermal suture technique: a prospective randomized study, Pool, S.M., et al., Dermatol Surg, 2015
[27]
Canthopexy as a routine blepharoplasty component, Flowers, R.S., Clin Plast Surg, 1993
[28]
Dynamic changes of tear fluid after cosmetic transcutaneous lower blepharoplasty measured by optical coherence tomography, Shao, C., et al., Am J Ophthalmol, 2014
[29]
A randomised double-blinded crossover study comparing pain during anaesthetising the eyelids in upper blepharoplasty: First versus second eyelid and lidocaine versus prilocaine, Pool, S.M., M.M. Struys, and B. van der Lei, J Plast Reconstr Aesthet Surg, 2015
[30]
Effect of platelet-rich plasma on patients after blepharoplasty surgery, Parra, F., et al., Orbit, 2018