["18952ef1cbdccf0cbb8e5a4952a65eee68d20ce3","7e2a2f2b3b32a29179d959013e1a74ab0cb7f604","42b4be201f4766cc48df2bfcdd9dcd3e1c4d6a61"]
Bodylift
body lift
body contouring
massive weight loss
upper body lift
lower body lift
3412
3412
Chapter reads
1
1
Chapter likes
7/10
Evidence score
09
9
Images included
02
2
Videos included
01
Introduction
Introduction and Definition
Body-lifting procedures create a firmer, tighter, more rejuvenated appearance for patients who have lax, ptotic tissues after massive weight loss (by dietary restrictions or postbariatric) or in case of aging in normal weight patients.
Massive weight loss is defined as a loss of 50 % of excess weight.26
Massive weight loss is defined as a loss of 50 % of excess weight.26
Obesity and it’s comorbidities is increasing in industrial countries since 1950, which means increasing need for skin redundancy after massive weight loss and/ or body- contouring, as an opportunity even for normal weight but disproportionate fat distribution as an aspect of aesthetic surgery. A variety of bariatric surgery techniques developed1; 2.The body mass index (BMI) is a minor indicator of percent of body fat and does not capture information on the mass of fat in different body sites and its contribution 3
Deformities of tissue ptosis after massive weight loss are typically circumferential, surgical treatment is most effective when patients achieved a BMI < 30 kg/ m2 stable for at least 6 months. Patients after massive weight loss with BMI 25- 30 kg/ m2 are best candidates for extensive body contouring4
With BMI 34 kg/ m2 , patients should be encouraged loosing more weight. In appropriate candidates body contouring with BMI 30- 34,9 kg/ m2 is possible for functional reasons. With BMI ≥ 40 and fail to respond to dietary, behavioral and medical therapies an consultation for Bariatric surgery should be taken into account10.
Deformities of tissue ptosis after massive weight loss are typically circumferential, surgical treatment is most effective when patients achieved a BMI < 30 kg/ m2 stable for at least 6 months. Patients after massive weight loss with BMI 25- 30 kg/ m2 are best candidates for extensive body contouring4
With BMI 34 kg/ m2 , patients should be encouraged loosing more weight. In appropriate candidates body contouring with BMI 30- 34,9 kg/ m2 is possible for functional reasons. With BMI ≥ 40 and fail to respond to dietary, behavioral and medical therapies an consultation for Bariatric surgery should be taken into account10.
Procedures include brachioplasty, upper back lift, abdominoplasty, lower back lift, and thigh lift. In 1990 Lockwood developed a circumferential body lift for normal weight patients with tissue resection on the superficial fascia to achieve tensionless sutures and decreasing complications like seromas or wound healing disorders 6. Carwell was the first to include post-bariatric patients 9.
The comorbidities of post bariatric patients (often with comorbidities including hyperlipidemia, diabetes mellitus, cardiovascular disease, obstructive sleep apnea, joint disease, vitamin D deficiency, low muscle function and depression) as well as the high numbers of complications led to a variety of surgery’s. In 2001 a combination of tissue removing and liposuction, called Saldanha technique (lipoabdominoplasty) was introduced: This method avoids undermining by performing an extensive liposuction and skin removal just under the derm 10. Further methods for different body parts were introduced. Besides, for achieving best aesthetic result the existing form of the body parts and body shape needs to be analysed, different types of fat distribution must be considered. Furthermore nutritional deficiency, comorbidities (diabetes) and cigarette abuse must be taken into account and need to be improved for best outcome 12.
The occurrence of complications tend to be higher in postbariatric patients. Reducing of complications is determined by reducing resection weight, operation time and blood loss.8a
The occurrence of complications tend to be higher in postbariatric patients. Reducing of complications is determined by reducing resection weight, operation time and blood loss.8a
Best possible esthetic and functional outcome means custom fit surgical staging of procedures with additional Liposuction or useful combination of firming procedures.
Patient's selection:
Comorbidities, BMI and cause of massive weight loss (postbariatric) influence choice of procedures and timing
Comorbidities, BMI and cause of massive weight loss (postbariatric) influence choice of procedures and timing
02
Indications for body lift
Tissue characteristica and general considerations
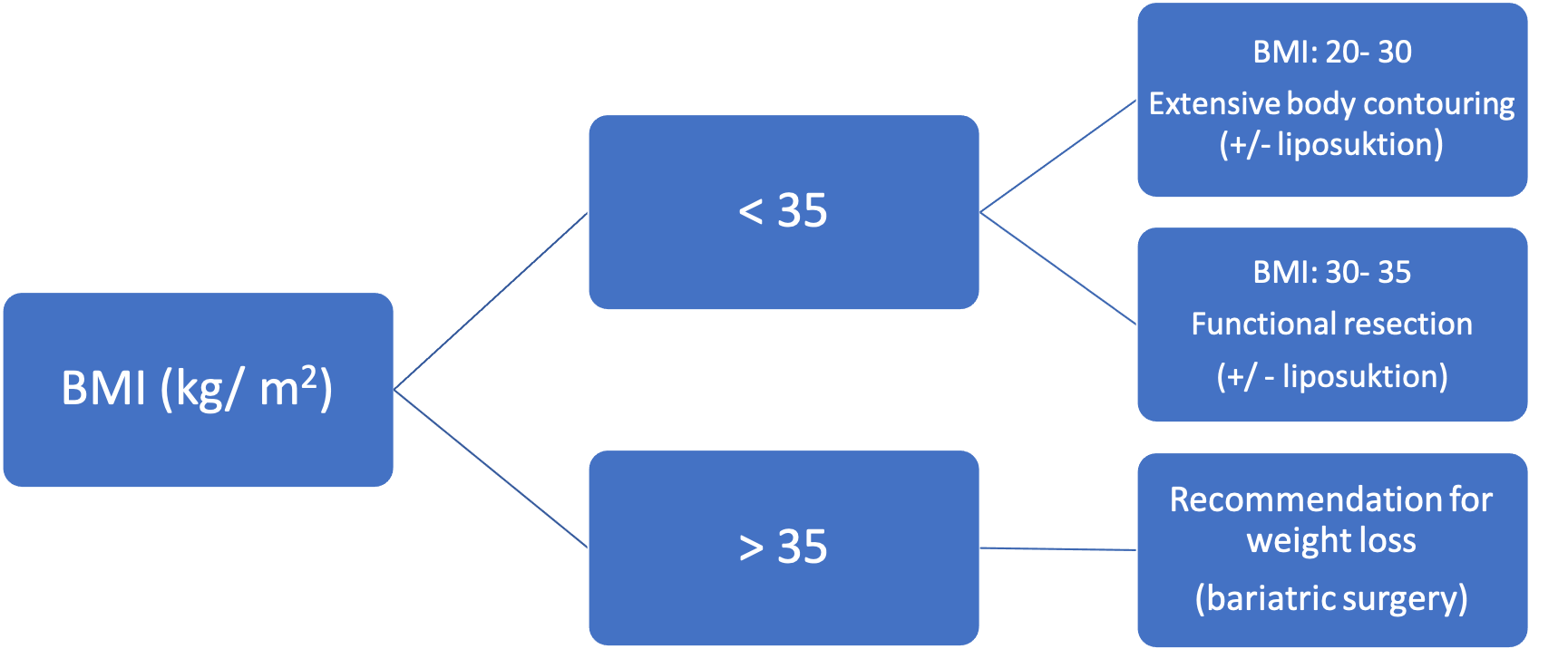
Table 1: BMI dependent choice of surgical techniques
Upper back- Lift23
Mild forms / single stage operation
Constitutional skin excess (Image 1) caused by
Weight loss
Aging (skin laxity)
Upper back lift is best performed at a different time than lower back lift because opposing lines of tension reduce optimal tissue removal and may cause banding across the back, and vascular compromise
Preparation
The “grasp or pinch test” is used to simulate lateral closure and confirms the margins of resection preoperatively

Figure 1: Pinch test for establishing markings
The incision line is marked like an eight (narrow in the middle line because of adhesions zone over spine)
Markings are done with female patients wearing their bra (for concealing scars)

Figure 2: Preoperative markings upper body lift
Severe forms
Extent of skin and soft tissue excess lateral and dorsal thorax
Treatment of upper breast fold and lower scapular or deeper lower chest fold possible
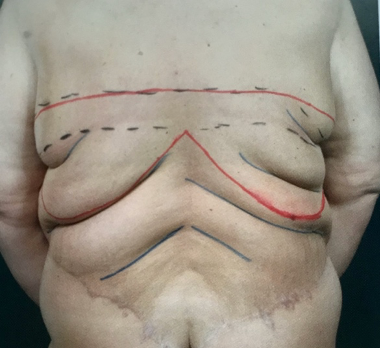
Figure 3: Preoperative markings in upper body lift (severe forms)
surgical goals: Resection of as many rolls as possible for creating a firm, flat back
Upper lateral body lift
Men:
combination of correcting gynecomastia or extensive skin (after massive weight loss)
• Small, invisible scars in axillary region 13
• in frontal view: Excision line = new inframammary fold
• Small, invisible scars in axillary region 13
• in frontal view: Excision line = new inframammary fold
Women:
ideal combination of lateral thoracic lift and mastopexy in ptotic breast (with wise- pattern technique/ Rubin Technique)
Medial and lateral flaps of dermis/ breast tissue are mobilized from chest wall for creating volume to upper parts of the breast21

Figure 4: markings of mastopexy in combination with lateral thoracic lift (red = incision line)
Lower body lift
Excess posterior skin requires belt lipectomy or lower body lift, depending on the deformation and the ptosis of skin after massive weight loss or in case of aging.
Surgical goal is creating a flat back by resecting lower back rolls (belt lipectomy), additionally with abdominoplasty (circumferential body lift) and/ or buttock augmentation.
Surgical goal is creating a flat back by resecting lower back rolls (belt lipectomy), additionally with abdominoplasty (circumferential body lift) and/ or buttock augmentation.
1. (Circumferential) belt lipectomy25
improves the lower truncal unit with resection of lower back rolls
resection line is higher than in lower body lift/ circumferential body lift
superior resection line is drawn first at the superior margin of the flank rolls
inferior line is drawn that crossed the interspinal line approximately 5 cm above the intergluteal cleft
2. (Circumferential) lower body lift9
improves buttock and thigh projection and allows resection of the nature of tissue ptosis in the trunk
skin markings and resection lines are lower than in belt lipectomy
inferior incision line is drawn either inside or at the superior margin of the gluteal projection
superior incision line should be drawn 5 cm above gluteal cleft

Markings of belt lipectomy (red) and lower body lift (blue)
3. Lower Body Lift with autologous buttock augmentation
Massive weight loss with lower back rolls and need for buttock projection
probably Liposuction for flanks/ hips or thighs necessary for contouring depending on shape analysis
A gluteal augmentation flap14, supplied by perforators from the superior gluteal artery, lateral sacral arteries, and lumbal artery 15, can be added to correct insufficient buttock projection (figure 5)
A pinch test less than 5 cm indicates that the autologous gluteal flaps are not sufficient to provide adequate buttock projection and additional volume should bussi Eva added
((Link: gluteal augmentation/ V Mandlik))
A pinch test less than 5 cm indicates that the autologous gluteal flaps are not sufficient to provide adequate buttock projection and additional volume should bussi Eva added
((Link: gluteal augmentation/ V Mandlik))
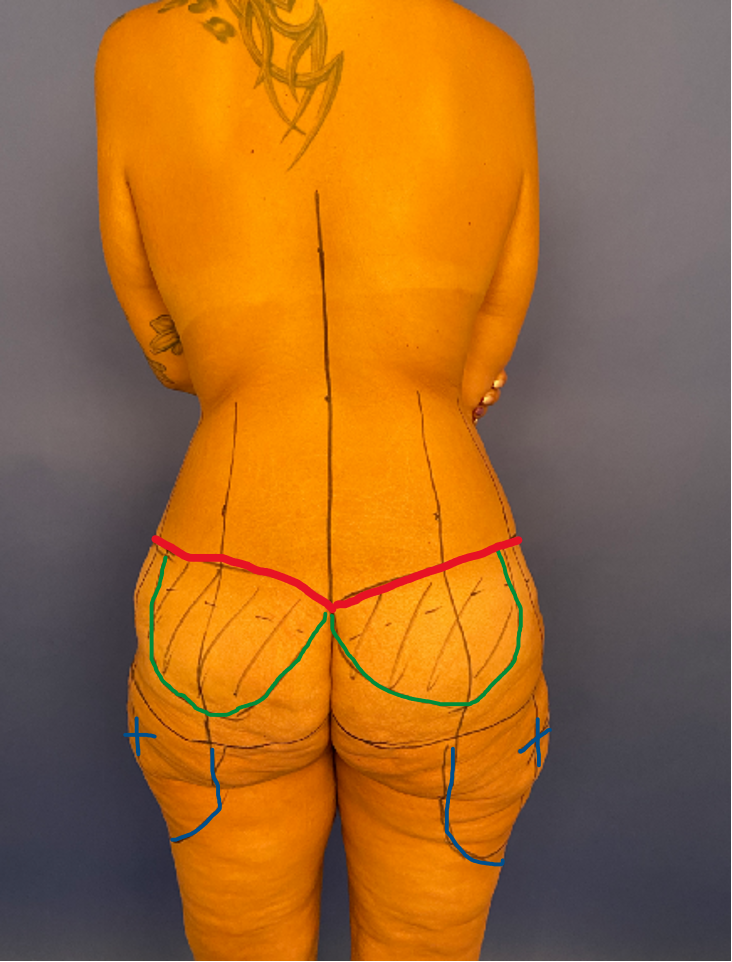
Figure 5: markings for lower body lift and buttock augmentation (red: incision line; green autologous fat flaps; blue: area of corrective liposuction
03
Surgical techniques
Surgical techniques:
Antibiotics perioperative i.v. (Cefazolin 2 g single shot); in case of allergies: Clindamycin 600 mg single shot)
Key components of upper body lift:
Preoperative markings:
Superior and inferior markings are drawn across the upper back, with the distance between them determined by pinch test and scar location
Perioperative:
Prone position with arm position: abduced max. 90. °, elbows flexed (reducing tension)
Checking for resection width, if necessary correcting of spindle, setting of hatch marks for closure (as the superior skin flap is often less wide than the lower tissue)(figure. 1 + 2)
Incision of spindle markings: electrocautery, straight to the muscle fascia leaving superficial fatty tissue on the fascia (prevention lymphatic drainage)
Cutting of the marked spindle without undermining flaps (* preparation of mammareduction or brachioplasty)
3-layer closing with regard to hatch marks:
Subcutaneous sutures to the deep fascia: 2-0 polydioxane (PDS)
Subcutaneous layer: 3-0 polyglecaprone (Monocryl)
Skin layer: intracuticular 4-0 Monocryl
Key components of upper lateral thoracic lift (in men):
Key components of mastopexy and lateral thoracic lift (in women):
Preoperative markings:
Markings: 1. marking: midline sternal notch to xiphoid; 2. marking: breast meridian line from mid clavicle to IMF (ignoring original nipple position); 3. marking: wise pattern with lateral portion including the
Perioperative:
Marking of NAC (3,8- 4,2mm diameter)
De-epitheliazation of wise pattern
Degloving of breast parenchyma by raising a flap of 1,5 cm thickness (central pedicled)
creating a subcutaneous pocket cranial
breast tissue and lateral flaps are transposed into the pocket and fixed onto the pectoralis fascia
Key components of lower body lift
Preoperative markings:
The “grasp test” is used to simulate lateral closure and confirms the margins of resection preoperatively
Superior and inferior markings are drawn across the lower back, and the distance between them is determined by pinch test and ultimate scar location
Cross-hatches are made across the horizontal marks to ease closure
Perioperative:
The patient is initially positioned prone for ultrasound-assisted lipoplasty/suction-assisted lipoplasty of the back, posterior hips/flanks, buttocks, thighs
When combination with abdominoplasty: the patient is primarily transferred to the supine position for anterior liposuction and abdominoplasty
Turning in prone position again: posterior excisions are performed with no undermining
Proceeding from the midline to lateral until reaching the mid-axillary line; in this way, the posterior skin closure is made easier
Scarpa’s layer with 2/0 vicryl
Dermis with 3/0 monocryl
3/0 monocryl for the subcuticular stitch
No need for drainage: quilting sutures to muscle fascia to reduce wound cavity
Key components of lower body lift with gluteal augmentation20
Preoperative markings:
The “grasp test” is used to simulate lateral closure and confirms the margins of resection preoperatively
An oval- shaped dermal fat flap originating in the medial half of the regularly excised supragluteal tissue is marked (figure 5)
The size of the flap is individualized according to the patient’s buttocks contour
Perioperative:
Liposuction for additional areas in prone position
incision of cranial marking and dissection of the flap down to the fascia at an oblique angle
A pocket is created for insertion of the flap by undermining the buttock in the plane above the fascia and extending it a sufficient length to reach the inferior gluteal crease
closure: 4 - layer's
Quilting sutures to the deep fascia (Scarpa layer) (2-0 polydioxane (PDS))
Dermis with 3/0 monocryl
3/0 monocryl for the subcuticular stitches
gluteal cleft: back stitches with non- resorbable sutures (Prolene 2-0)
04
Postoperative Care
Follow up:
Visitations: weekly up to the 6th week
Using compression belt or bra immediately postoperative for 6 weeks consequently for reducing seroma
Reduced Elevation of arms for 2 weeks, than improvement of motion to normal range of motion
Ultrasound examination every 7 days. If seroma occurs: puncture and injection of triamcinolone 40 % (beginning after two weeks, repetition every two weeks)
Wound care
keeping wounds dry until two weeks, disinfection after showering
in lower body lift: daily showering of sutures in gluteal cleft from beginning and disinfection after visits to the toilet
Scar therapy
Beginning after 2 weeks postoperatively
Scar massage (twice a day)
Fluid/gel: maintaining moisturization and decreasing tension
Patient education on proper wound care is a simple method of improving the cosmetic appearance of surgical scars
05
Common complications and their management
Complications
Minor complications
Wound dehiscence (most common)
superficial and minor:
often suture knot infection
Conservative therapy: healing in secondary intention; removal of exposured sutures
Increasing wound care: showering, disinfection, absorbent dressing
Deep and major:
no signs of infection: debridement and secondary closure
with signs of infection: antibiotics (testing of microorganism, beginning with clindamycin 600 mg 1-1-1); revision surgery
Hematoma
Small: leave or aspire
Large: puncture not possible; revision surgery, closing dead space
Infection
Superficial: in case of wound healing disorder: debridement, microbiology testing (due to testing choice of antibiotics)
Deeper tissue infection: abscess drainage or revision surgery and i.v. antibiotics (due to testing of microorganism)
Seroma
risk increases by 5% for each unit increase in BMI at the time of plastic surgery19
Punktion of seroma consequently until it ends up
weekly controls: ultrasound examination
Major complications
DVT (deep vein thrombolism)
Prophylaxis17:
elastic compression stockings/ intermittent pneumatic compression stockings
chemoprophylaxis: low-dose unfractionated heparin, low-molecular-weight heparin 1 day before surgery and 7 days after surgery18
(early) mobilization
06
Algorithm for Decision making
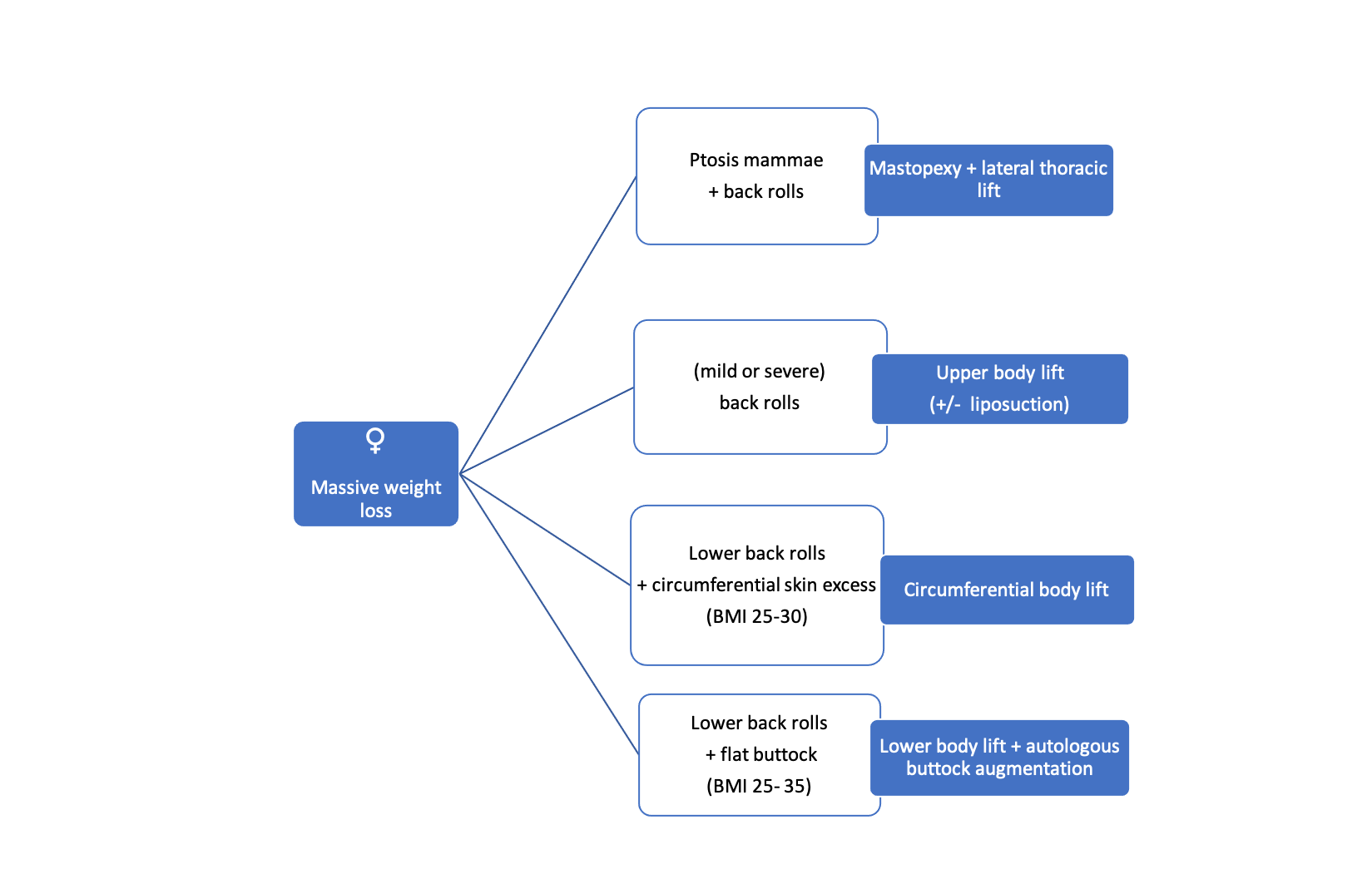
Table 2: Procedure Selection
Images
Figure 2: Preoperative markings upper body lift
Figure 3: Preoperative markings in upper body lift (severe forms)
Figure 4: markings of mastopexy in combination with lateral thoracic lift (red = incision line)
Preoperative markings for lower body lift
Figure 1: Pinch test for establishing markings
Figure 5: markings for lower body lift and buttock augmentation (red: incision line; green autologous fat flaps; blue: area of corrective liposuction
Table 1: BMI dependent choice of surgical techniques
Table 2: Procedure Selection in women
Markings of belt lipectomy (red) and lower body lift (blue)
References
[1]
An outcomes analysis of patients undergoing body contouring surgery after massive weight loss, Shermak MA, Chang D, Magnuson TH, Schweitzer MA, Plast Reconstr Surg, 2006
[2]
The history of metabolic and bariatric surgery: Development of standards for patient safety and efficacy, Blaine T Phillips 1 , Scott A Shikora , Metabolism, 2018
[3]
Increasing prevalence of overweight among US adults. The National Health and Nutrition Examination Surveys, 1960 to 1991, Kuczmarski RJ, Flegal KM, Campbell SM, Johnson CL, JAMA, 1994
[4]
Body Mass Index: Obesity, BMI, and Health: A Critical Review, Nuttall FQ, Nutr Today, 2015
[5]
Body contouring following massive weight loss, Taylor J, Shermak M, Obes Surg, 2004
[6]
Reducing complications in post-bariatric plastic surgery: our experience and literature review, Romano L, Zoccali G, Orsini G, Giuliani M, Acta Biomed, 2019
[7]
Lower body lift with superficial fascial system suspension, Lockwood T, Plast Reconstr Surg, 1993
[8]
Circumferential torsoplasty, Carwell GR, Horton CE Sr, Ann Plast Surg, 1997
[9]
Lipoabdominoplasty, Saldanha OR, Federico R, Daher PF, Malheiros AA, Carneiro PR, Azevedo SF, Saldanha Filho OR, Saldanha CB, Plast Reconstr Surg, 2009
[10]
An outcomes analysis of patients undergoing body contouring surgery after massive weight loss, Shermak MA, Chang D, Magnuson TH, Schweitzer MA, Plast Reconstr Surg, 2006
[11]
Risk factors and complications after body-contouring surgery and the amount of stromal vascular fraction cells found in subcutaneous tissue, Morandi EM, Ploner C, Wolfram D, Tasch C, Dostal L, Ortner F, Pierer G, Verstappen R, Int Wound J, 2019
[12]
Body contouring, Shermak MA, Plast Reconstr Surg, 2012
[13]
Boomerang pattern correction of gynecomastia, Hurwitz DJ, Plast Reconstr Surg, 2015
[14]
Mastopexy after massive weight loss: dermal suspension and selective auto-augmentation, Rubin JP, Khachi G, Clin Plast Surg, 2008
[15]
Circumferential Contouring of the Lower Trunk: Indications, Operative Techniques, and Outcomes-A Systematic Review, Carloni R, De Runz A, Chaput B, Herlin C, Girard P, Watier E, Bertheuil N, Aesthetic Plast Surg, 2016
[16]
Circumferential torsoplasty, Carwell GR, Horton CE Sr, Ann Plast Surg, 1997
[17]
Gluteal Augmentation and Contouring with Autologous Fat Transfer: Part I, Ghavami A, Villanueva NL, Clin Plast Surg, 2018
[18]
Remodeling bodylift with high lateral tension, Pascal JF, Le Louarn C, Aesthetic Plast Surg, 2002
[19]
Autoprosthesis buttock augmentation during lower body lift, Sozer SO, Agullo FJ, Wolf C, Aesthetic Plast Surg, 2005
[20]
Factors impacting thromboembolism after bariatric body contouring surgery, Shermak MA, Chang DC, Heller J, Plast Reconstr Surg, 2007
[21]
Prevention of venous thromboembolism in the plastic surgery patient, Davison SP, Venturi ML, Attinger CE, Baker SB, Spear SL, Plast Reconstr Surg, 2004
[22]
, , ,
[23]
Prevention of venous thromboembolism in body contouring surgery: a national survey of 596 ASPS surgeons, Clavijo-Alvarez JA, Pannucci CJ, Oppenheimer AJ, Wilkins EG, Rubin JP, Ann Plast Surg, 2011