["41532ae3d4f101474aa22e7a73b8f5a0c2aedae9","42b4be201f4766cc48df2bfcdd9dcd3e1c4d6a61"]
Mastopexy
mastopexy
ptosis mammae
surgical approach
short scar
4819
4819
Chapter reads
0
0
Chapter likes
7/10
Evidence score
34
34
Images included
01
1
Videos included
01
Definition
Definition
Mastopexy is understood as the fixation, tightening and reshaping of the female breast after lowering/sagging of the breast tissue (ptosis mammae) with the aim of repositioning the gland and restoring a natural form that corresponds to the patient's esthetic desire.
Various authors developed flowcharts and calculation models for the ideal dimensions of the female breast; some with digital programs for download 03. The most common findings are the relationship between upper pole-to-lower pole perc22entage proportion: 45:55 04; also the correct position of the female breast on the chest wall: between 2./3. and 6./7. rib; from the sternal margin to the anterior axillary fold (5). Different ideals and standards of beauty exist depending on the region, age or culture. 22
Definition of bra cup sizes
The European standard EN 13402 defines bra sizes based on the "bust girth" and the "underbust girth". Bras are labeled with the under bust girth (rounded to the nearest multiple of 5 cm), followed by a letter code that indicates the "cup size".
The decisive factor is the difference between the intramammary circumference (underbust girth) and the size measured over the breast (with a firm breast or with bra; "bust girth"). Cup A (USA: AA): 13 cm difference between inferior and upper breast width, Cup B (USA: A): 15 cm, Cup C (USA: B): 17 cm, Cup D (USA: C): 19 cm
This means that the size of the breast in relation to the figure, even with the same cup size, can vary depending on the body measurements. (Table: Bra Size Calculator 2020) 06
The decisive factor is the difference between the intramammary circumference (underbust girth) and the size measured over the breast (with a firm breast or with bra; "bust girth"). Cup A (USA: AA): 13 cm difference between inferior and upper breast width, Cup B (USA: A): 15 cm, Cup C (USA: B): 17 cm, Cup D (USA: C): 19 cm
This means that the size of the breast in relation to the figure, even with the same cup size, can vary depending on the body measurements. (Table: Bra Size Calculator 2020) 06
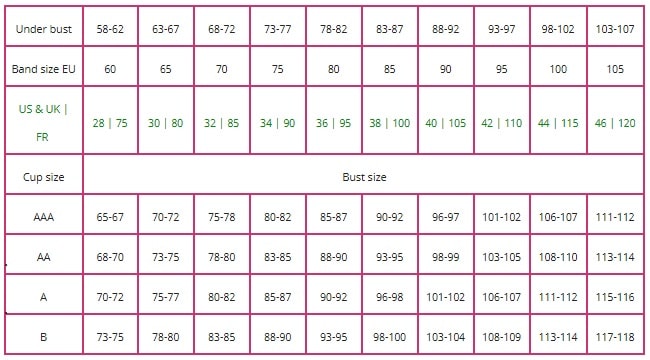
Cup size
02
Classification
Classification
One of the most frequently cited classifications is that of Regnault (06), which particularly targets the position of the nipple-areola complex (NAC) in relation to the inframammary fold (IMF/ 5). However, this classification does not adequately represent the complex anatomy of the shape disorders in the female breast.
Shiffman (07) compared various classifications of breast ptosis in terms of their significance (including Lalardrie-Jouglard (1973), Regnault (1976), Lewis (1983), Brink (1990), LaTrenta and Hoffman (1994), de la Torre and Vasconez (2007) ) and pointed out that the benefit of individual classifications depends on the planned therapy and therefore each of them should be used individually.Lalardrie and Jouglard found that ptosis occurs as the thoracomammary angle decreases and falls below 90 °, and the convexity of the upper breast changes to a concave shape.Lewis classified the breast ptosis depending on the hypertrophy or atrophy of the mammary gland.Brink’s classification attempted to distinguish between true ptosis, glandular ptosis, parenchymal maldistribution, and pseudoptosis.Vebros (08) bases his classification on the quality of the suspension and the skin.
A reliable classification of the ptosis mammae should ideally take into account not only the glandular sagging and excess of skin but also the position of the inframammary fold (IMF), the development of the glandular quadrants and the relation between the skin excess above (Nipple-Jugulum-Distance, NJD) and below (Nipple-IMF-Distance, NIF) the nipple. In any classification, the ptosis of the mammary gland and the position of the NAC should be seen separately!
The Regensburg classification of ptosis mammae
Type 1: orthotopic IMF, all quadrants developed, F-Fp-Distance <15 cm, NJD<25 cm
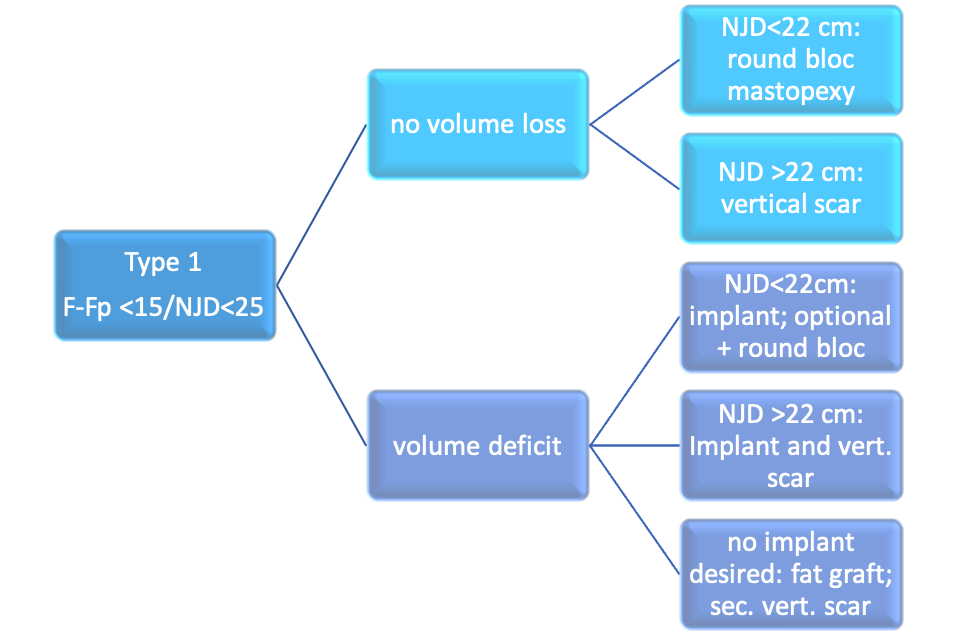
Table1new
Type 2: orthotopic IMF, all quadrants developed, F-Fp-Distance>15 cm, NJD > 25 cm
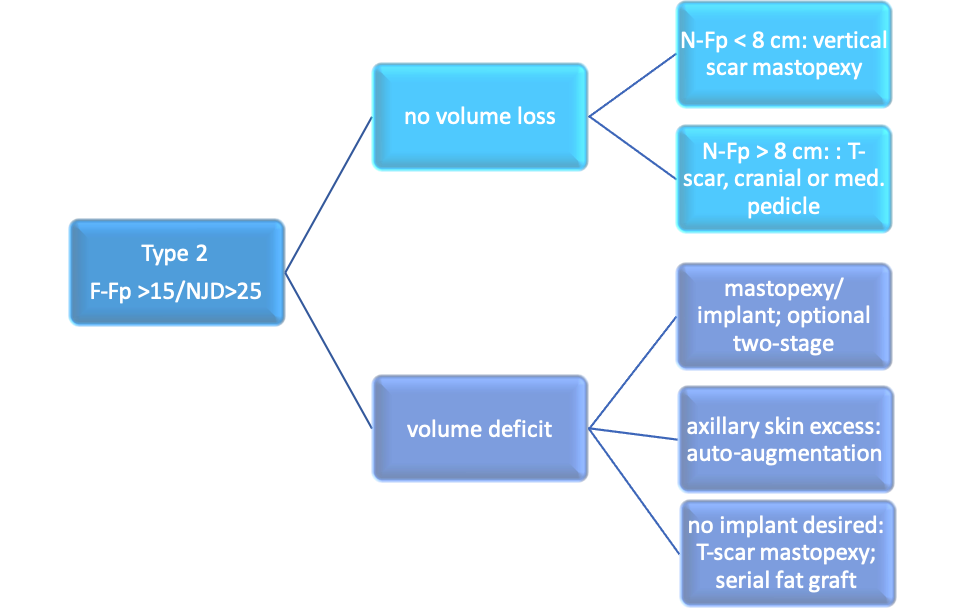
Table2new
Type 3: caudalized or orthotopic IMF, severe loss of skin elasticity and/or glandular ptosis
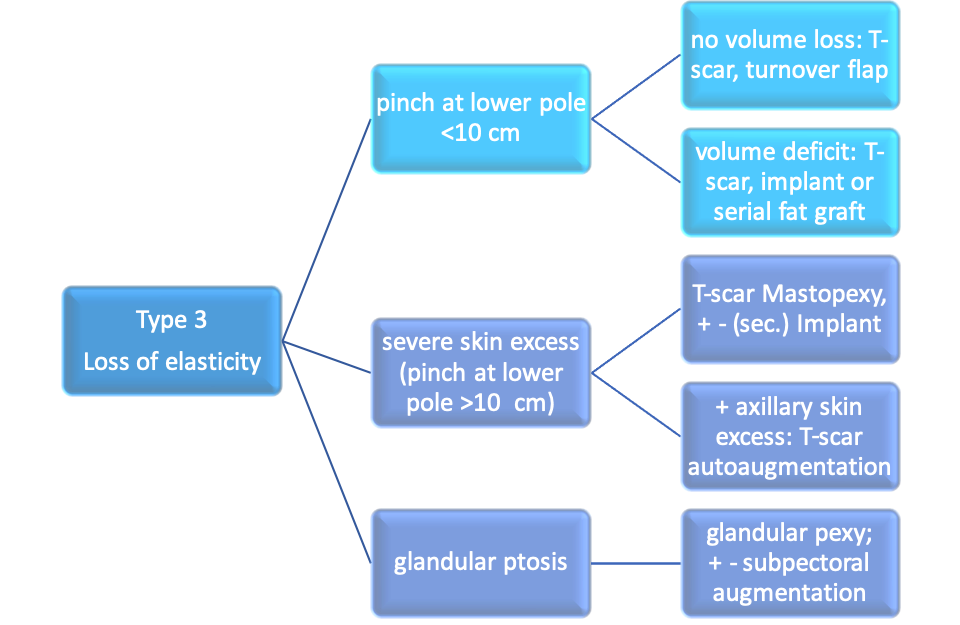
Table3new
Type 4: elevated IMF, hypoplastic lower quadrants (tuberous breast; see chapter malformation!)
Definition of the tables above:
Orthotopic IMF (Inframammary fold):
Humeral midpoint (half length of humerus =1/10 of body size in cm)
All quadrants developed:
No pathological or genetic hypoplasia of the lower quadrants; in supine position no volume deficit of the different quadrants
All quadrants hypoplastic:
A-cup or less; mismatch between chest and breast volume
skin excess and/or glandular ptosis:
Sagging of the lower pole in upright position; skin has to be reduced in the majority of cases
F-Fp-Distance:
F= Inframammary fold; Fp= Projection of F to the anterior skin of the breast. . The normal IMF-position dependent on the body height varies only for 1-2 cm.
Important: the NJD/IMF-ratio cannot be representative for all shapes of breast and has to be correlated to breast form, body size and pseudoptosis!
N-Fp-Distance:
Nipple to IMF-projection; describes the ptosis of the NAC related to the virtual position after mastopexy as an indicator for the amount of skin resection.
Pinch at lower pole:
Inferior skin excess that can be pinched to receive tight breast shape.
03
Causes of ptosis mammae
Causes of ptosis mammae
The sagging and lowering of the female breast can have various, sometimes multifactorial causes, which can be an indication for mastopexy:
Genetic
Congenital, hypoplastic development of the ligamentous suspension of the breast (Fascia, Cooper's ligaments) leads to early relaxation and sagging of the (often normal-sized) breast.
Malformation
Tuberous breast deformity, especially grade II and III, is characterized by moderate to severe hypoplasia of the lower quadrants of the breast (v. Heimburg,09. This aspect is reinforced by hypoplastic dermis under the irregularly enlarged areola with a transareolar glandular prolapse (Ribeiro L; 10). Asymmetries (up to the Amazon syndrome) are typically characterized by a hypoplastic breast on one side and a relatively enlarged to ptotic breast at the other side; often with the indication for augmentation on the smaller side and mastopexy on the larger side.
Postpartum
After pregnancy and breastfeeding, the involution leads to relaxation of the overstretched skin and fixation structures after previous, functional hyperplasia of the mammary gland.
Postbariatric
After massive weight loss through diet or restrictive / malabsorptive surgery, the hypoplasia of the intramammary adipose tissue (12) with a mostly pre-existing, fatty macromastia leads to a pronounced ptosis of the remaining mammary gland with simultaneous, more or less pronounced excess tissue in the thorax, especially laterally towards the axilla.
Macromastia
The enlarged breast is usually associated with a weight-related lowering and sagging of the gland, especially in older patients.
Hormonal changes
The mammary gland develops especially under the influence of growth hormone (GH), progesterone and prolactin (PRL) and, like few organs, is subject to a pronounced hormonal influence. (02). Hormonal changes, including iatrogenic (e.g. hormon-suppressive or ablative therapy in breast cancer), can lead to an involution of the breast with consecutive ptosis mammae.
Age-related Involution
During menopause there is a natural involution of the female breast with regressive changes of the lobular epithelium and a loss of volume.
Iatrogenic
Severe scar formations, e.g. at the lower pole of the breast, as well as insufficient techniques of skin tightening (like round bloc in case of severe skin excess at the lower pole) can lead to ptosis of skin and/or breast tissue.
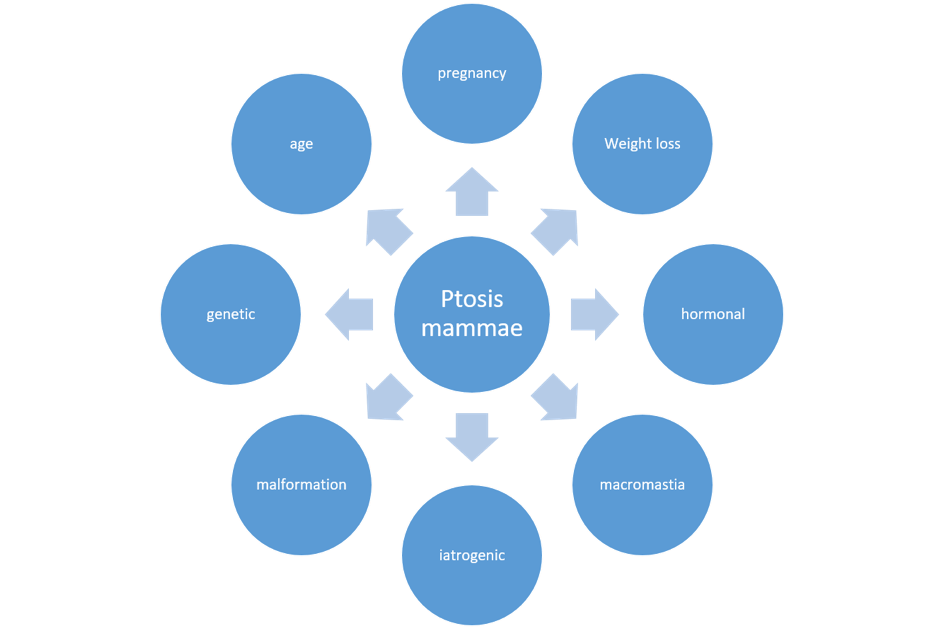
Causes of ptosis
04
Anatomy
Anatomical structures
The female mammary gland is a paired organ with prefascial position on the ventral side of the thorax. It covers 2/3 of the pectoralis major muscle and is connected to the thorax via Cooper's ligaments. It consists of 20-22 glandular lobes in average that converge in the area of the nipple. A glandular portion usually extends towards the axilla (tail of spence). The greatest density of glandular tissue is behind the nipple, while the proportion of adipose tissue is higher in the peripheric parts.
The inferior border of the gland is formed by the inframammary fold, which is characterized by firm tissue connections between the dermis and the fascial structures of the thoracic wall. It usually corresponds to the middle of the humerus on the hanging arm.
The NAC, which consists of the nipple and the areola, is ideally positioned at the level of the strongest projection of the (firm) breast above the 4th-5th rib.
Various authors developed flowcharts and calculation models for the ideal dimensions of the female breast; some with digital programs for download (3).The most common findings are the relationship between upper pole-to-lower pole percentage proportion: 45:55 (4); also the correct position of the female breast on the chest wall: between 2./3. and 6./7. rib; from the sternal margin to the anterior axillary fold (5).Different ideals and standards of beauty exist depending on the region, age or culture.
The inferior border of the gland is formed by the inframammary fold, which is characterized by firm tissue connections between the dermis and the fascial structures of the thoracic wall. It usually corresponds to the middle of the humerus on the hanging arm.
The NAC, which consists of the nipple and the areola, is ideally positioned at the level of the strongest projection of the (firm) breast above the 4th-5th rib.
Various authors developed flowcharts and calculation models for the ideal dimensions of the female breast; some with digital programs for download (3).The most common findings are the relationship between upper pole-to-lower pole percentage proportion: 45:55 (4); also the correct position of the female breast on the chest wall: between 2./3. and 6./7. rib; from the sternal margin to the anterior axillary fold (5).Different ideals and standards of beauty exist depending on the region, age or culture.
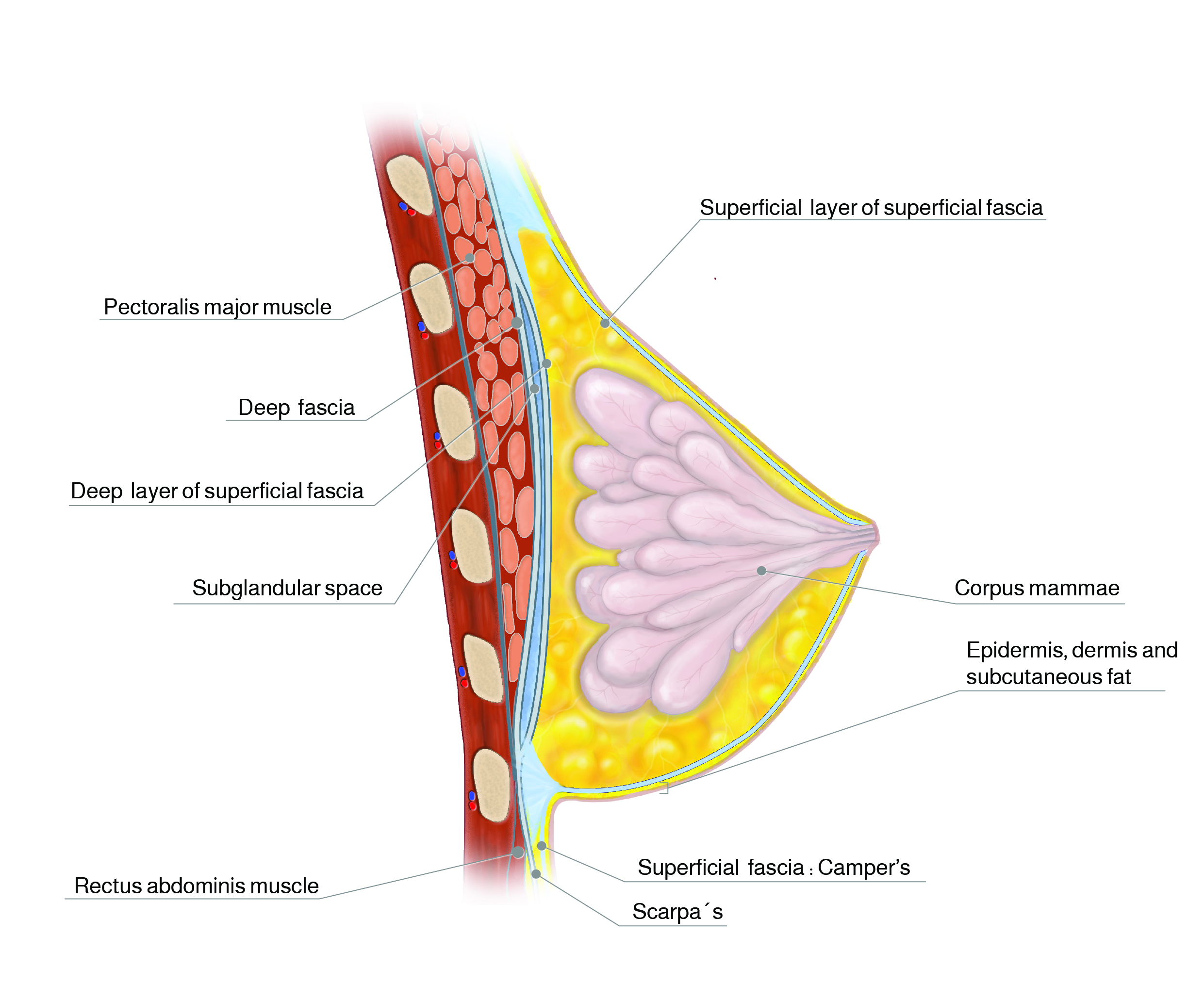
Anatomy breast
05
Indication for mastopexy
Indication for mastopexy
A difference must be made between a) aesthetic and b) medical indication.
The transition between the two groups of indications is often undefined.In contrast to the hypertrophic breast / macromastia with a clear indication for reduction in breast size, no significant improvement for pain and myogelosis is generally to be expected in mastopexy.
A medical indication can be seen especially in the following cases:
-Extensive overlap of the skin with the formation of moisty regions and, as a result, of eczema and intertrigo (often after weight loss)
- Ptosis as a result of a severe malformation of the female breast (tubular or tuberous breast)
-severe malformation of the breast that cannot be concealed by clothing.
In the majority of cases,
however, the decision for mastopexy should be seen as an aesthetic indication with the patient`s desire to improve the body shape; the claim for the ideal shape and unvisible scar formation is particularly high.
The transition between the two groups of indications is often undefined.In contrast to the hypertrophic breast / macromastia with a clear indication for reduction in breast size, no significant improvement for pain and myogelosis is generally to be expected in mastopexy.
A medical indication can be seen especially in the following cases:
-Extensive overlap of the skin with the formation of moisty regions and, as a result, of eczema and intertrigo (often after weight loss)
- Ptosis as a result of a severe malformation of the female breast (tubular or tuberous breast)
-severe malformation of the breast that cannot be concealed by clothing.
In the majority of cases,
however, the decision for mastopexy should be seen as an aesthetic indication with the patient`s desire to improve the body shape; the claim for the ideal shape and unvisible scar formation is particularly high.
Consultation, informed consent and typical risks
Since patients generally have high expectations regarding the aesthetic result in addition to medical reasons, preliminary talks, planning and preoperative preparation are one of the most important elements of therapy.
The first consultation
What kind of expectations has the patient; and are the expectations of the postoperative result realistic and achievable?
Are there any risk factors (e.g. obesity, smoking, radiation or previous breast operations) in the medical history?
Anatomical malformations must be taken into account (tubular breast, Poland syndrome, scoliosis, funnel chest)
Is the volume of the mammary gland sufficient to achieve a satisfactory result for the patient after mastopexy alone?
Has family planning been completed?
Scarring: skin type? Pre-existing hypertrophic scars?
If there are risk factors for breast cancer or if the patient is over 50 years old, mammography should be planned preoperatively after consultation with the gynecologist; for younger patients, an ultrasound examination with written documentation is sufficient.
Are there any risk factors (e.g. obesity, smoking, radiation or previous breast operations) in the medical history?
Anatomical malformations must be taken into account (tubular breast, Poland syndrome, scoliosis, funnel chest)
Is the volume of the mammary gland sufficient to achieve a satisfactory result for the patient after mastopexy alone?
Has family planning been completed?
Scarring: skin type? Pre-existing hypertrophic scars?
If there are risk factors for breast cancer or if the patient is over 50 years old, mammography should be planned preoperatively after consultation with the gynecologist; for younger patients, an ultrasound examination with written documentation is sufficient.
The informed consent:
Basically, be careful in case of unrealistic expectations!
Any photos presented by the patient (often of breast-augmented models with ideal dimensions) should be discussed critically and the anatomical differences to the patient must be pointed out.
The information should take place with a sufficient time frame before the operation; We regularly discuss the typical risks during the initial consultation, prepare an information sheet for the patient and repeat the common risks during the preoperative consultation. At this point, the information sheet is signed a second time by the doctor and patient.
The focus should also be placed on the aesthetic risks (asymmetry, shape disorder, scarring and warping, etc.).The courts often consider that 24 hours prior to an esthetic operation is aesthetic is insufficient.
Any photos presented by the patient (often of breast-augmented models with ideal dimensions) should be discussed critically and the anatomical differences to the patient must be pointed out.
The information should take place with a sufficient time frame before the operation; We regularly discuss the typical risks during the initial consultation, prepare an information sheet for the patient and repeat the common risks during the preoperative consultation. At this point, the information sheet is signed a second time by the doctor and patient.
The focus should also be placed on the aesthetic risks (asymmetry, shape disorder, scarring and warping, etc.).The courts often consider that 24 hours prior to an esthetic operation is aesthetic is insufficient.
Possible adverse events (to be explained to the patient) : Bleeding (very rarely preserved blood: the risk of HIV and Hep.C is indicated but seldom!), Infection, wound healing disorder, visible or painful scars, form disorder, re-ptosis or asymmetry, reduced sensation of skin/MAC or blood circulation disorder ; necrosis of the skin, tissue or nipple in very rare cases, breastfeeding problems, cyst formation, pain, thrombosis / embolism (therefore heparin support with the risk of thrombopenia), further operations.
Photo documentation:
For each patient, standardized conventional photographs must be taken standing upright preoperatively.
The following procedures have proven to be the minimum standard:
The following procedures have proven to be the minimum standard:
Frontal, with arms down and upraised vertically and straight
Frontal with the upper body bent at 45 degrees, both sides
Arms down from both sides
Inclined pictures with 45 degrees and hanging arms
In case of relevant erythema or eczema in the lower breast, additional picture with the breast raised by the patient
If available, 3-D photography with a scanning system can be helpful (e.g. for volumetry)
06
Preoperative planning
Preoperative planning
Markings:
Marking takes place the day before or the morning before the operation (before taking premedication drugs); the patient must be advised in advance of not using skin cream, etc.
The patient is standing upright, with her arms hanging relaxed ; the shoulders should be symmetrical on the same level (Cave spine deformities; e.g. scoliosis!). The women are advised not to move during marking.
A first line is painted vertical from sternal notch crossing the xiphoid to the navel.
Then bilaterally a line is marked from the mid of the clavicula to the median of the breast mound, which defines the way of the NAC up to their correct position.
Important is the exact height of the nipple. It is defined by imaging a 90°-angle from the skin above the breast down to the IMF (F-Fp; which means that the angle between the nipple-IMF-line to the chest will be less than 90°!); the horizontal position is defined by the mid-clavicula line.
Next, the lower edge of the vertical scar is defined by the crossing between IMF and a vertical line from the new nipple-position.
The new Areola is designed 1-2 cm higher than the nipple position; depending from the planned diameter (3,5-4,5 cm).A dome-shaped figure is painted with the length of the branches 5-8 cm in average (depending of the diameter and the expected skin excess). From the edge of the branches, a vertical line is designed to the inferior point at IMF after forming a breast mould to both sides.
In case of asymmetrical medialisation of the areola, it is helpful to hide the NAC during painting of the new position; in this manner malpositioning of the new NAC can be avoided.
If the expected NAC-to-IMF-distance will be more than 7-8 cm, a short horizontal scar is planned.
The patient is standing upright, with her arms hanging relaxed ; the shoulders should be symmetrical on the same level (Cave spine deformities; e.g. scoliosis!). The women are advised not to move during marking.
A first line is painted vertical from sternal notch crossing the xiphoid to the navel.
Then bilaterally a line is marked from the mid of the clavicula to the median of the breast mound, which defines the way of the NAC up to their correct position.
Important is the exact height of the nipple. It is defined by imaging a 90°-angle from the skin above the breast down to the IMF (F-Fp; which means that the angle between the nipple-IMF-line to the chest will be less than 90°!); the horizontal position is defined by the mid-clavicula line.
Next, the lower edge of the vertical scar is defined by the crossing between IMF and a vertical line from the new nipple-position.
The new Areola is designed 1-2 cm higher than the nipple position; depending from the planned diameter (3,5-4,5 cm).A dome-shaped figure is painted with the length of the branches 5-8 cm in average (depending of the diameter and the expected skin excess). From the edge of the branches, a vertical line is designed to the inferior point at IMF after forming a breast mould to both sides.
In case of asymmetrical medialisation of the areola, it is helpful to hide the NAC during painting of the new position; in this manner malpositioning of the new NAC can be avoided.
If the expected NAC-to-IMF-distance will be more than 7-8 cm, a short horizontal scar is planned.
07
Surgical techniques of mastopexy
Round bloc technique (11)
Indication
Type 1; Mild Ptosis, F-Fp < 15 cm/NJD < 22 cm. Small to normal gland size; Cup A-B.
Marking
Areola diameter 3.5-4 cm; 2nd. oval circle, maximum 3 cm higher than original.
Technique
De-epithelization of the area between the two circles; Incision of the caudal outer circumference up to the median line. Preparation between gland and subcutis caudally, laterally and medially up to the pectoral fascia. Mobilization of the gland ventrally of the fascia in a 3-finger-wide tunnel upwards and fixation of the gland on the fascia with delayed- or non-resorbable suture. Periareolar purse string sutures (PDS or non-absorbable; 3.0 -4. 0) to diminuish the outer circle. Wound closure by running sutures.
Advantages: Limited scar area; minor surgical trauma
Disadvantages: only suitable for small tightening; widened scars; Recurrent ptosis
Advantages: Limited scar area; minor surgical trauma
Disadvantages: only suitable for small tightening; widened scars; Recurrent ptosis
Vertical mastopexy with cranial pedicle ("monobloc"; mod. Lassus / Lejour) (13)
Indication
Type1: F-Fp <15 cm/ NJD 22- 25 cm; or Type 2: F-Fp >15 cm/ NJD >25 cm/ N-Fp < 8 cm. Moderate ptosis, Average size of the gland, Cup A to C. Moderate skin excess in the lower breast pole.

Mastopexy Lejour
Marking
Areola 3.5-4 cm; “Dome design” as described by M. Lejour. Cranially pedicled skin flap.
Technique
De-epithelialization of the MAC- pedicle including an approx. 2 cm zone caudal to the areola.
Mobilization between subcutis and gland caudally, laterally and medially (similar to a virtual, subcutaneous wise pattern figure).
Mobilization of a 3-5 cm -tunnel superior to the pectoralis fascia.
A fixation suture is made between this point and the cranial mid of the gland (non-absorbable or delayed). Shortening of the vertical scar by 2 continuous, deep and superficial intradermal sutures.
Continuous suture for the areola; in case of higher tension, possibly an additional purse string suture is needed.
Mobilization between subcutis and gland caudally, laterally and medially (similar to a virtual, subcutaneous wise pattern figure).
Mobilization of a 3-5 cm -tunnel superior to the pectoralis fascia.
A fixation suture is made between this point and the cranial mid of the gland (non-absorbable or delayed). Shortening of the vertical scar by 2 continuous, deep and superficial intradermal sutures.
Continuous suture for the areola; in case of higher tension, possibly an additional purse string suture is needed.

Mastopexy Lejour postop
Vertical mastopexy with medial pedicle and rotation (Hall-Findlay) (14)
Indication
as 2.; often in combination with a breast reduction.
Slightly better projection; occasionally bottoming out.
Slightly better projection; occasionally bottoming out.
Marking
As 2.; the pedicle is designed from medially.
Technique
De-epithelialization of the MAC- pedicle
C-shaped incision around the pedicle transglandular down to the fascia.
Rotation of the gland for 90 degrees cranially; Fixation by pillar sutures between the gland flaps.
Running suture for the vertical scar with a slight shortening; Periareolar suture (absorbable).
C-shaped incision around the pedicle transglandular down to the fascia.
Rotation of the gland for 90 degrees cranially; Fixation by pillar sutures between the gland flaps.
Running suture for the vertical scar with a slight shortening; Periareolar suture (absorbable).
In case of malformation (tubular breast): Spreading, Dividing and Unfurling of the mammary gland (15)
Indication
Type 4; Breast malformation with hypoplasia of (inferior) parts of the gland and skin deficiency (tubular breast; see chapter Malformation)

Tuberous breast2
Marking
If the skin envelope at the lower pole is deficient, only periareolar, as described under 1)
Otherwise with an additional small vertical scar
Otherwise with an additional small vertical scar
Technique
De-epithelization of the marked periareolar zone and incision semicircular at the inferior circumference. Mobilization between the subcutis and gland to the fascia
Preparation of the entire gland on the surface of the fascia up to the midline behind the nipple.
In case of hyperdense glandular tissue, radial incisions from dorsal (spreading); otherwise cross- incision at the level of the nipple at the backside of the gland and forming of a pocket caudally, which can be spread out down to the planned new inframammary fold by longitudinal incisions.
It is important to fix the lower pole of the gland at the new inframammary fold with resorbable sutures
Wound closure by purse string and separate periareolar suture.
Preparation of the entire gland on the surface of the fascia up to the midline behind the nipple.
In case of hyperdense glandular tissue, radial incisions from dorsal (spreading); otherwise cross- incision at the level of the nipple at the backside of the gland and forming of a pocket caudally, which can be spread out down to the planned new inframammary fold by longitudinal incisions.
It is important to fix the lower pole of the gland at the new inframammary fold with resorbable sutures
Wound closure by purse string and separate periareolar suture.

Tuberous breast postop2
16
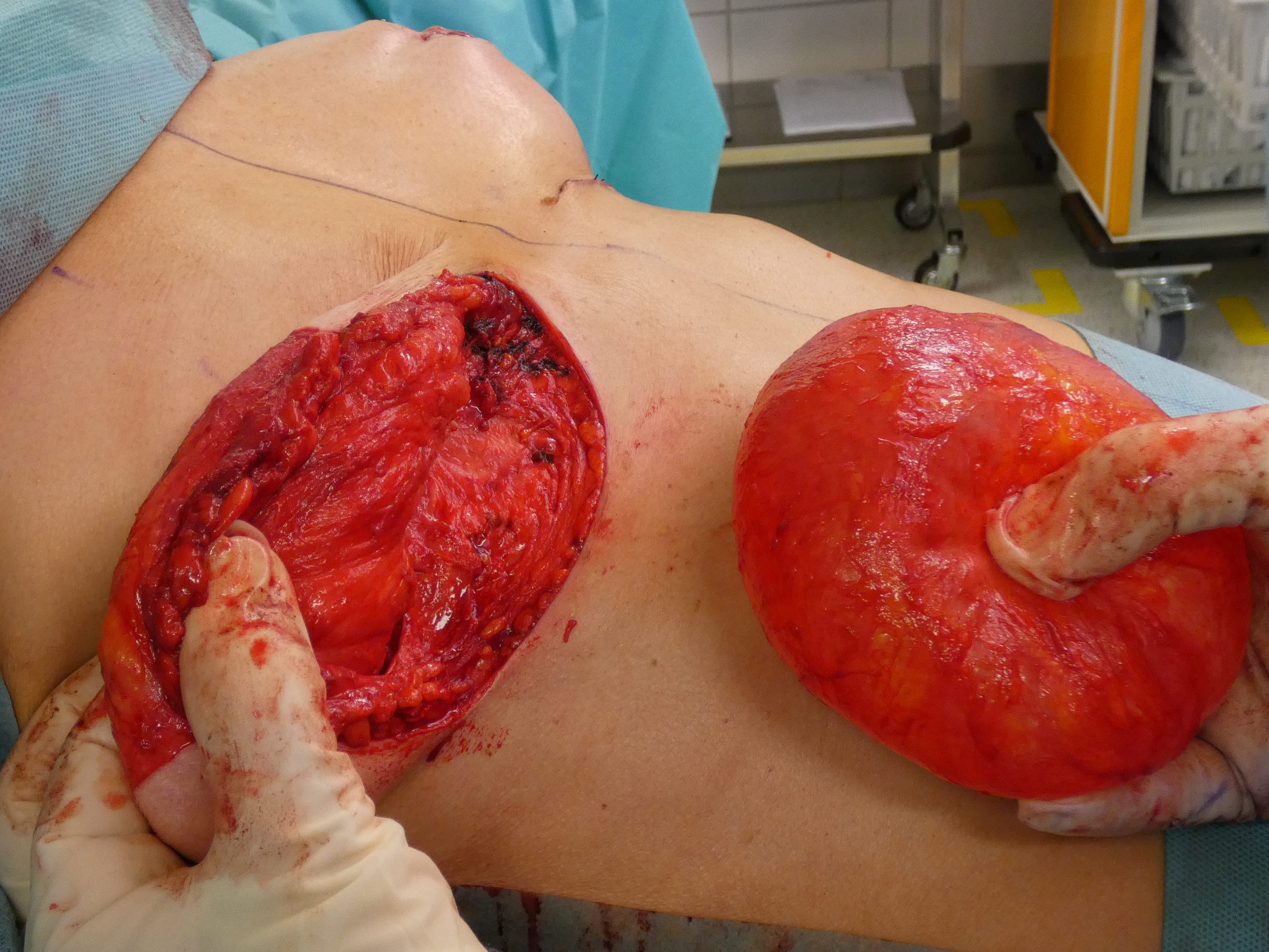
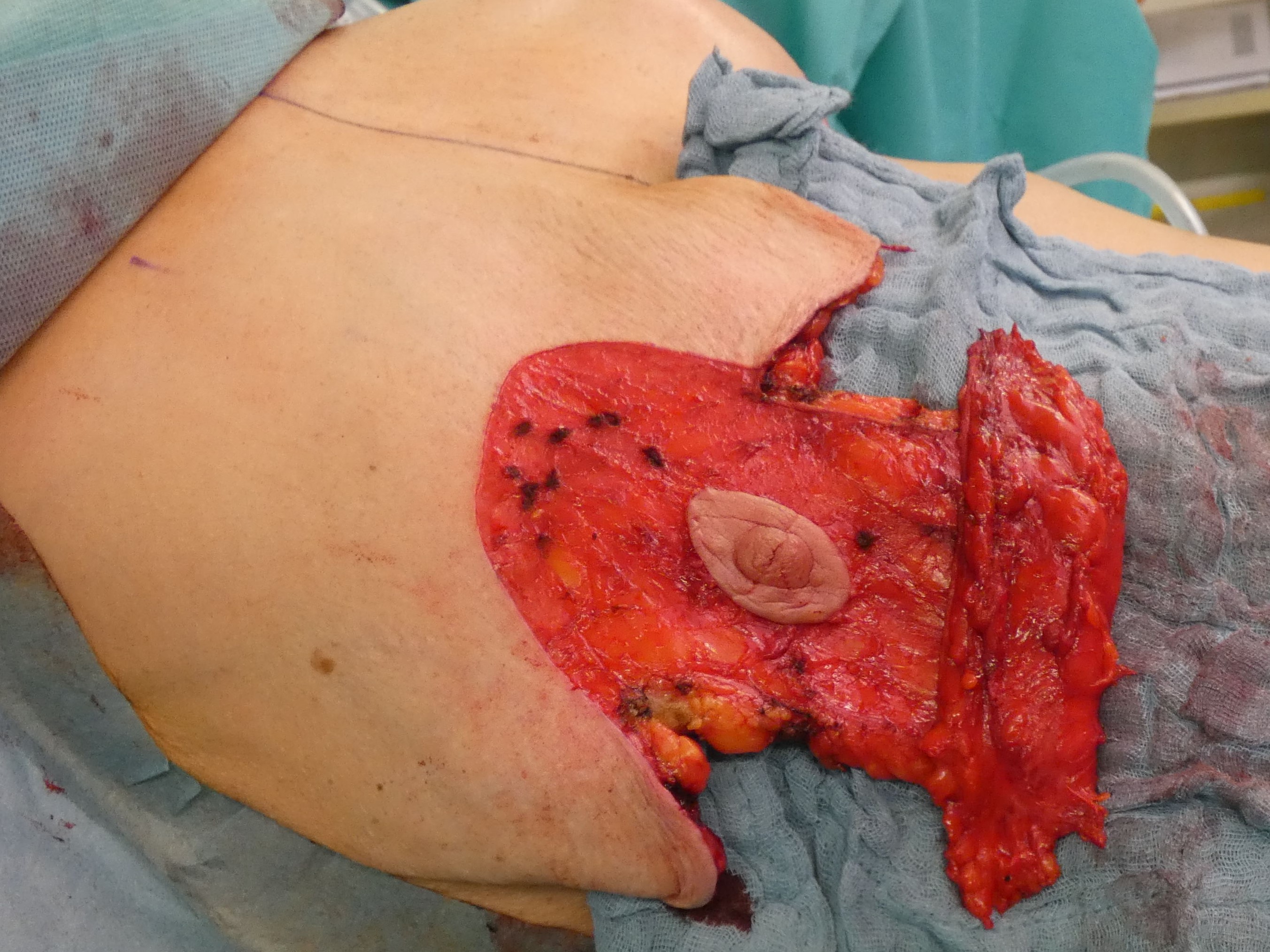
T-scar Mastopexy with inferocentral, septum-based pedicle
Indication
Type 2: F-Fp >15 cm/ NJD > 25 cm/ N-Fp > 8 cm; Type 3: Loss of elasticity. Advanced skin excess or loss of elasticity; possibly combined with reduction mammaplasty
Marking
Wise pattern: 4-4,5 cm NAC; 5-7 cm vertical scar; horizontal part depending to skin excess
Technique
De-epithelization of an inferior pedicle which includes the NAC and circular incision of the new position. Vertical skin incision laterally and medially of the pedicle according to the expected skin excess. Mobilization subcutaneously from all sides down to the fascia; the gland gets its blood supply through the fascia and the Wühringer septum. Fixation of the cranial part of the gland to the fascia at the height of the 3rd rib, with medial and lateral plication if necessary.
Caudal stabilisation with turnover-flap
Indication
Type 3; loss of elasticity, caudal skin excess >10 cm vertically. Often after implant removal.
Marking
T-scar, cranial pedicle (depending to the amount of skin surplus)
Technique
Complete deepithelialisation of the whole pedicle supporting the NAC including the caudal area down to the IMF; including the Wise-Pattern area caudally. Removal of the implant, if necessary. Mobilisation of the gland on the pectoral fascia cranially and mastopexy of the gland between the 2nd rib and the retroareolar tissue. The deepithelialized caudal flap is folded 180° and sutured to the pectoralis fascia to support projection and stabilize the lower pole. In case of a longer caudal pedicle, the lateral branches of the wise-pattern-figure can be sutured to the cental part to gain more volume in this area. The skin pedicles are closed over the new breast mound.

Autoaugmentation prae
Autoaugmentation: implant ex
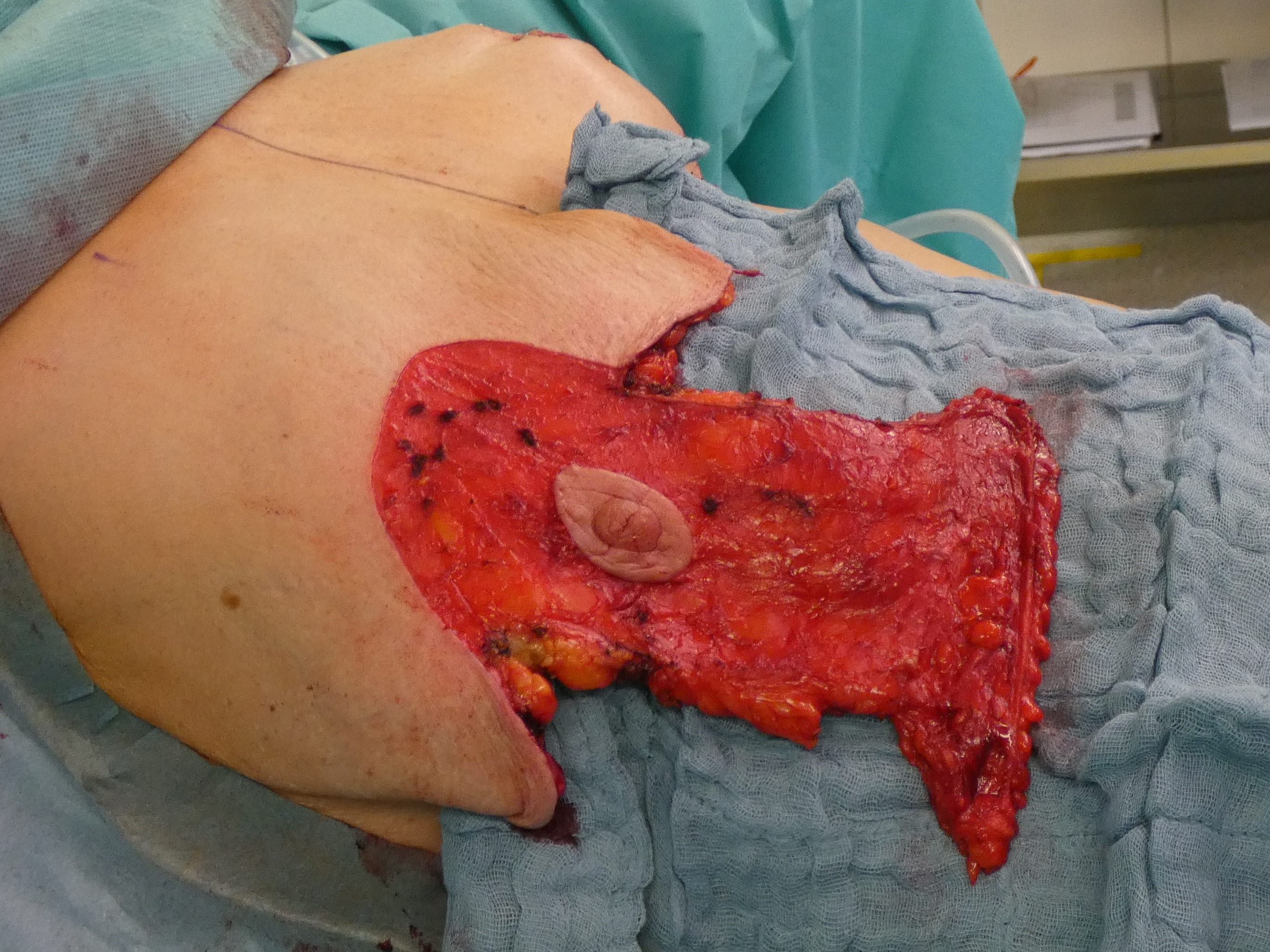
Autoaugmentation. flap
Autoaugmentation: flap folded

Autoaugmentation painting

Autoaugmentation : folding the pedicle

Autoaugmentation: closing skin envelope
Auto-augmentation and internal suspension (Rubin) (17)
Indication
Type 2/3; massive excess of skin, also towards the axilla, after excessive weight loss; small gland left with the patient`s desire for autologous enlargement
Marking
Like Wise Pattern; with medial wing up to the median line and lateral wing up to the middle axillary line, rising upwards at the axilla and including the skin excess.
Technique
Incision of 3.5-4 cm areola diameter; caudocentral pedicle.
Complete de-epithelization of the entire remaining incision area.
Preparation subcutaneously down to the fascia; no mobilization of the gland from the pectoral fascia!
The medial and lateral pedicle is mobilized up to the sternal margin or to the anterior axillary line and folded around the gland, so that the dermis flaps finally cover the gland completely like an implant envelope. These flaps are sutured together with delayed resorbable sutures.
Fixation of the border of this sheath with cranialization on the pectoral fascia; the skin flaps are placed over this “anatomical implant” and sutured together.
Complete de-epithelization of the entire remaining incision area.
Preparation subcutaneously down to the fascia; no mobilization of the gland from the pectoral fascia!
The medial and lateral pedicle is mobilized up to the sternal margin or to the anterior axillary line and folded around the gland, so that the dermis flaps finally cover the gland completely like an implant envelope. These flaps are sutured together with delayed resorbable sutures.
Fixation of the border of this sheath with cranialization on the pectoral fascia; the skin flaps are placed over this “anatomical implant” and sutured together.

Rubin side pre

Rubin side

Rubin front
Mastopexy and Augmentation (18)
Indication
All types; ptosis and hypomastia; patient`s desire for enlargement.
It should be noted that the combination of mastopexy and implant-supported augmentation is associated with an increased risk of form disorders; the possibility of two-stage surgery should be discussed with the patient.
It should be noted that the combination of mastopexy and implant-supported augmentation is associated with an increased risk of form disorders; the possibility of two-stage surgery should be discussed with the patient.

Mastopexy/Augmentation
Marking
With a slight ptosis of 1. ° following Regnault`s classification and the desire to enlarge by at least one cup size, the implant will fill up the skin envelope and inframammary incision may be sufficient.
If this does not fit for the skin excess, a periareolar tightening figure should be used (see pt. 1).
In case of Ptosis 2-3°, a vertical figure should always be planned (see point 2).
If this does not fit for the skin excess, a periareolar tightening figure should be used (see pt. 1).
In case of Ptosis 2-3°, a vertical figure should always be planned (see point 2).
Technique
The expected result can be simulated with test implants and a bustier to demonstrate the form facing a mirror. Depending on the desired breast size, the volume and shape of the implants and the tightening figure are planned:
a) Skin excess expected to be slight:
Inframammary incision; round or anatomical implants.
b) Excess of skin to be expected even after augmentation (tested with staples intraoperatively):
Periareolar deepitheliasation; semicircular incision at the caudal border and preparation between gland and subcutis, if the subcutaneous tissue amount is sufficient. The implant pocket is formed epi- or subpectorally.
c) Moderate to severe excess of skin to be expected:
Deepitheliazation of the vertical figure, fixation of the dermal flap caudally in the IMF after augmentation.
CAVE: When lowering of the inframammary fold is planned, it is important to spread the gland down to the new fold and fix it to avoid “double-bubble”!
a) Skin excess expected to be slight:
Inframammary incision; round or anatomical implants.
b) Excess of skin to be expected even after augmentation (tested with staples intraoperatively):
Periareolar deepitheliasation; semicircular incision at the caudal border and preparation between gland and subcutis, if the subcutaneous tissue amount is sufficient. The implant pocket is formed epi- or subpectorally.
c) Moderate to severe excess of skin to be expected:
Deepitheliazation of the vertical figure, fixation of the dermal flap caudally in the IMF after augmentation.
CAVE: When lowering of the inframammary fold is planned, it is important to spread the gland down to the new fold and fix it to avoid “double-bubble”!

Mastopexy/Augmentation postop
Mastopexy and Lipofilling
Indication
Type1-4; patient`s desire for moderate enlargement and rejection of foreign body
Sufficient donor areas available
Request for liposuction.
Sufficient donor areas available
Request for liposuction.
Marking
Like mastopexy alone; a slight skin excess is planned.
Marking of the liposuction areas.
Marking of the liposuction areas.
Technique
Due to the required exposure time of the tumescent solution, the procedure starts with the infiltration of the liposuction areas.
The next step performs de-epithelialization of the NAC- pedicle, mobilization of the subcutaneous tissue and mastopexy of the gland, as well as temporary closure with clips to simulate the shape, regarding the estimated volume excess by fat transfer.
The fatty tissue harvested by liposuction is filtrated or centrifuged and infiltrated with a 2mm cannula in a criss-cross technique without bolus injection in the subcutaneous layer and behind the gland; an intraglandular injection has to be avoided.
The next step performs de-epithelialization of the NAC- pedicle, mobilization of the subcutaneous tissue and mastopexy of the gland, as well as temporary closure with clips to simulate the shape, regarding the estimated volume excess by fat transfer.
The fatty tissue harvested by liposuction is filtrated or centrifuged and infiltrated with a 2mm cannula in a criss-cross technique without bolus injection in the subcutaneous layer and behind the gland; an intraglandular injection has to be avoided.

Lipofilling prä

Lipofilling post
08
Tips and tricks
“Shortening and diminuishing the scars”:
In addition to tightening the breast, a scar as invisible as possible is important to most of the patients.
The mere reduction to a periareolar scar (Benelli) often leads to a further decrease of the NAC and recurrence of the ptosis.
The scars also tend to widen if the ratio between the circumference of the new areola and the outer figure is more than 1: 2. Above this ratio, an additional vertical scar should always be planned to avoid ugly scarring periareolar.
The mere reduction to a periareolar scar (Benelli) often leads to a further decrease of the NAC and recurrence of the ptosis.
The scars also tend to widen if the ratio between the circumference of the new areola and the outer figure is more than 1: 2. Above this ratio, an additional vertical scar should always be planned to avoid ugly scarring periareolar.
The vertical scar can be significantly reduced using our special suture technique:
From the cranial edge, a running suture is performed in the deep dermis using pseudomonofile, absorbable suture material.
At the caudal margin, the subcutaneous tissue is thoroughly freed of fat to allow skin shrinkage in this area.
The same suture now runs back cranially in the superficial dermis and can now be shortened by gently pulling both ends of the suture.
To improve scarring periareolar, an additional purse string suture is planned if the ratio between circumference of the new areola and the incision figure is more than 1.5. This suture is tightened to the diameter of the areola and the knot is hidden deeply below the dermis; care must be taken to ensure that the suture is not exposed anywhere to avoid infection.
Our own studies have shown that non-absorbable sutures (e.g. Goretex) have a higher risk of exposition but are superior to absorbable sutures in a 10-year follow-up concerning scar surface and diameter.
At the caudal margin, the subcutaneous tissue is thoroughly freed of fat to allow skin shrinkage in this area.
The same suture now runs back cranially in the superficial dermis and can now be shortened by gently pulling both ends of the suture.
To improve scarring periareolar, an additional purse string suture is planned if the ratio between circumference of the new areola and the incision figure is more than 1.5. This suture is tightened to the diameter of the areola and the knot is hidden deeply below the dermis; care must be taken to ensure that the suture is not exposed anywhere to avoid infection.
Our own studies have shown that non-absorbable sutures (e.g. Goretex) have a higher risk of exposition but are superior to absorbable sutures in a 10-year follow-up concerning scar surface and diameter.
Images
Type 2
Type 3
Type 4
Choice of technique
Causes of ptosis
Cup size
Rubin front
Rubin side pre
Rubin side
Mastopexy/Augmentation
Mastopexy/Augmentation
Mastopexy/Augmentation postop
Mastopexy/Augmentation postop
Mastopexy Lejour
Mastopexy Lejour 2
Mastopexy Lejour postop
Mastopexy Lejour postop 2
Tuberous breast
Tuberous breast2
Tuberous breast postop2
Tuberous breast postop
Table1new
Table3new
Table2new
Anatomy breast
Lipofilling prä
Lipofilling post
Autoaugmentation prae
Autoaugmentation: implant ex
Autoaugmentation. flap
Autoaugmentation: flap folded
Autoaugmentation painting
Autoaugmentation : folding the pedicle
Autoaugmentation: closing skin envelope
Videos
Preoperative markings
References
[1]
A New Tool for Breast Anthropometric Measurements: Presentation and Validation for Women and Men, Maksym Mikołajczyk, Anna Kasielska-Trojan and Bogusław Antoszewski, Aesthetic Plast Surg, 2019
[2]
, , ,
[3]
Population analysis of the perfect breast: a morphometric analysis, Mallucci P, Branford OA, Plast Reconstr Surg, 2014
[4]
, , ,
[5]
Breast ptosis. Definition and treatment, Regnault P., Clin Plast Surg, 1976
[6]
Breast ptosis. Definition and treatment, Regnault P., Clin Plast Surg, 1976
[7]
Breast Augmentation. Classification of Breast Ptosis, Melvin A. Shiffman , Springer Berlin, Heidelberg, 2009
[8]
Classification and Operative Tactic in the Treatment of the Small Ptotic Breast , Vebros J, Chir Belg , 1976
[9]
The 29. tuberous breast deformity: classification and treatment, von Heimburg D, Exner K, Kruft S, Lemperle G , Br J Plast Surg , 1996
[10]
Tuberous breast: a new approach, Ribeiro L, Canzi W, Buss AJ, Accorsi AJ , Plast Reconstr Surg , 1998
[11]
Mastoplasty after Massive Weight Loss: Redefinition and Stabilization of the Breast Mound with Submuscular Autoprosthesis, Colicchia GM et al, J Cutan Aesthet Surg, 2019
[12]
Mammary Gland Development, Hector Macias and Lindsay Hinck, Wiley Interdiscip Rev Dev Biol., 2012
[13]
A new periareolar mammaplasty: the “round block” technique, Benelli L , Aesthetic Plast Surg , 1990
[14]
Vertical Mammaplasty and Liposuction of the Breast , M Lejour, Plast Reconstr Surg, 1994
[15]
A simplified vertical reduction mammaplasty: shortening the learning curve, Hall-Findlay EJ.Hall-Findlay EJ, Plast Reconstr Surg, 1999
[16]
The tuberous breast deformity: classification and treatment, von Heimburg D, Exner K, Kruft S, Lemperle G.von Heimburg D, et al, Br J Plast Surg, 1996
[17]
Refinement of the central pedicle breast reduction by application of the ligamentous suspension, Würinger E.Würinger E, Plast Reconstr Surg, 1999
[18]
Mastopexy after massive weight loss: dermal suspension and selective auto-augmentation, Rubin JP, Khachi G.Rubin JP, et al, Clin Plast Surg, 2008
[19]
Strategies and Challenges in Simultaneous Augmentation Mastopexy. , Spring MA, Hartmann EC, Stevens WG.Spring MA, et al, Clin Plast Surg, 2015