["45c55662cb1e71bd85d27061be7cb8299309ac58","b5253982ad925e2c131e35dfc76354bd43d1d52e"]
Wrist arthroscopy
arthroscopy
hand
wrist
ganglion
ulna impaction syndrom
TFCC
STT
2313
2313
Chapter reads
0
0
Chapter likes
2/10
Evidence score
57
57
Images included
01
1
Videos included
01
Introduction
Introduction
Wrist arthroscopy allows complete visualization under enlargement of bony and ligamentary tissue. Its purpose is to evaluate an anatomic diagnosis and, if indicated, to provide treatment. Current indications, though numerous and potentially expanding, are also controversial. Wrist arthroscopy has become to the gold standard for the diagnosis of intra-articular pathology and triangular fibrocartilage lesions.
This chapter cannot replace a detailed medical textbook on wrist arthroscopy and surgery of the hand. Rather, it should provide guidance for the basic setup, the surgical technique and the indication for wrist arthroscopy.
This chapter cannot replace a detailed medical textbook on wrist arthroscopy and surgery of the hand. Rather, it should provide guidance for the basic setup, the surgical technique and the indication for wrist arthroscopy.
02
Method
Method
Arthroscopy can be performed under regional or general anaesthesia.
Instruments
The instruments, including the arthroscope with its image reproduction, should be checked before surgery will begin.
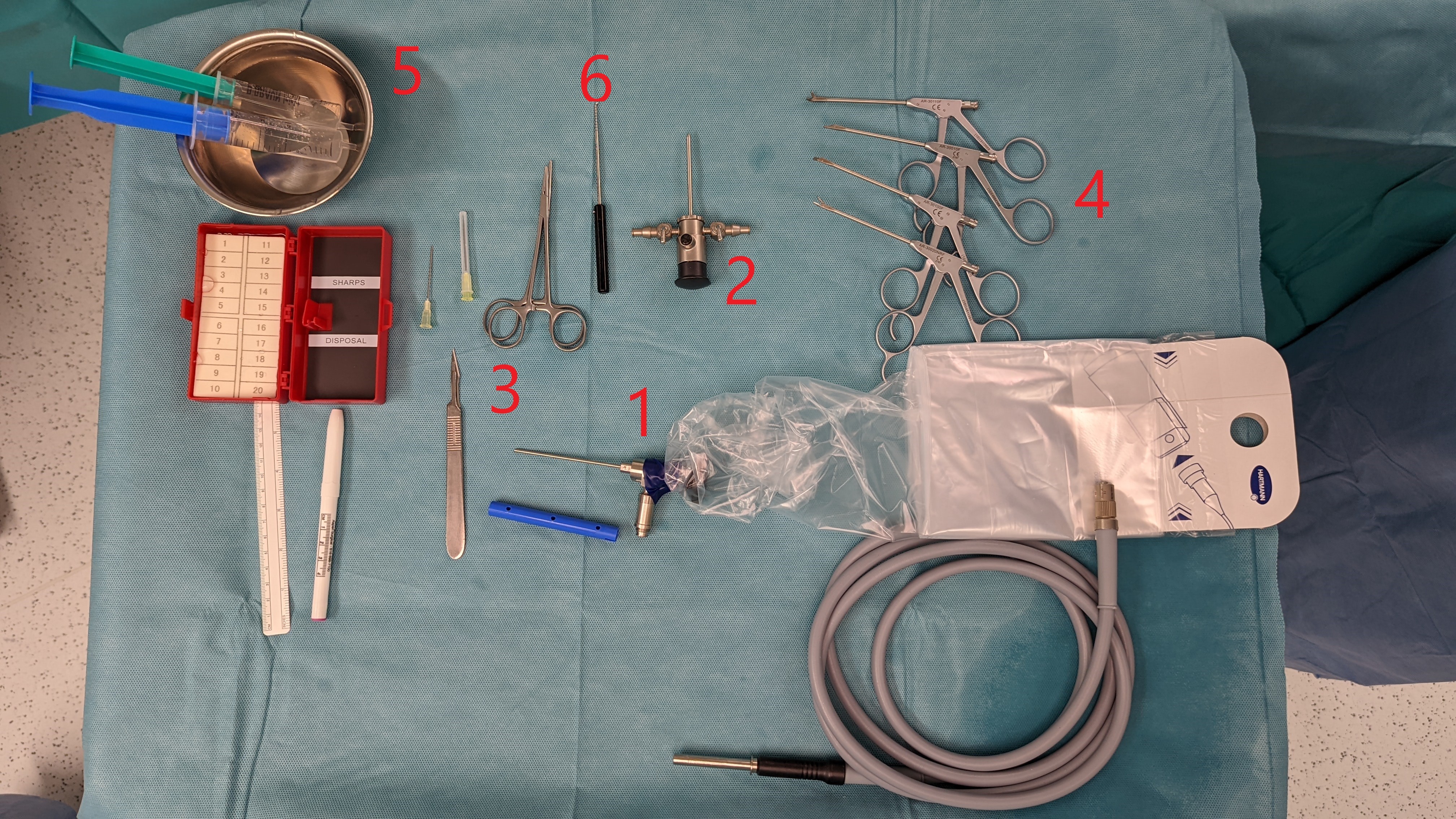
Instruments
1. Arthroscope with lightsource
2. Trocar
3. Instruments for acess: 20 gaudge needle; scalpel (no. 11); mosquito clamp
4. arthroscopic tissue forceps
5. saline solution
6. probe (hook)
A shaver, which is not shown in the picture, can also be used for debridement.
2. Trocar
3. Instruments for acess: 20 gaudge needle; scalpel (no. 11); mosquito clamp
4. arthroscopic tissue forceps
5. saline solution
6. probe (hook)
A shaver, which is not shown in the picture, can also be used for debridement.
Set-Up
The patient is placed with the shoulder abducted and elbow flexed at 90 degrees.
A tourniquet is placed above the elbow and the arm freely hanging. The distraction is achieved with weights on a strap on the tornique. Depending on the patient, weights of 2-6 kg are used.
The surgeon sits opposite the monitor, which is located in the area of the patient's legs.
A tourniquet is placed above the elbow and the arm freely hanging. The distraction is achieved with weights on a strap on the tornique. Depending on the patient, weights of 2-6 kg are used.
The surgeon sits opposite the monitor, which is located in the area of the patient's legs.

Set-up with 90° at elbow joint
Surgical technique
In our clinic we prefer the dry wrist arthroscopy (DWA)
Contrary to classically described wet arthroscopy, no fluid is injected into the radiocarpal joint for distention before developing portals. Overall, the processof diagnostic joint arthroscopy is similar to that in wet technique Instruments, like burrs and synoviotomes, are used in the same fashion. However, in DWA, one should always ensure the side valve of thearthroscope is open to prevent suction from collapsing the capsule, which would hinder the surgeon’s view. Saline maybe used to flush any debris that clogs the suction or to achieve better visualization.Dry wrist arthroscopy
Contrary to classically described wet arthroscopy, no fluid is injected into the radiocarpal joint for distention before developing portals. Overall, the processof diagnostic joint arthroscopy is similar to that in wet technique Instruments, like burrs and synoviotomes, are used in the same fashion. However, in DWA, one should always ensure the side valve of thearthroscope is open to prevent suction from collapsing the capsule, which would hinder the surgeon’s view. Saline maybe used to flush any debris that clogs the suction or to achieve better visualization.Dry wrist arthroscopy
03
Diagnostic intraoperative precedure
Diagnostic intraoperativ procedure
A systematic approach to evaluation of the wrist by arthroscopy starts with a thorough knowledge of the three-dimensional anatomy of the region. Traditionally, the workhorse arthroscopic portals are positioned over the dorsal wrist,avoiding the risk of injury to the neurovascular structures of the volar wrist. Anyway the volar portals are undispensable in evaluation and repairing especially dorsal bony and soft-tissue structures.Diagnostic Wrist Arthroscopy
Portals
The following table gives an overview of the different portals and the respective view of the different structures.Diagnostic Wrist Arthroscopy
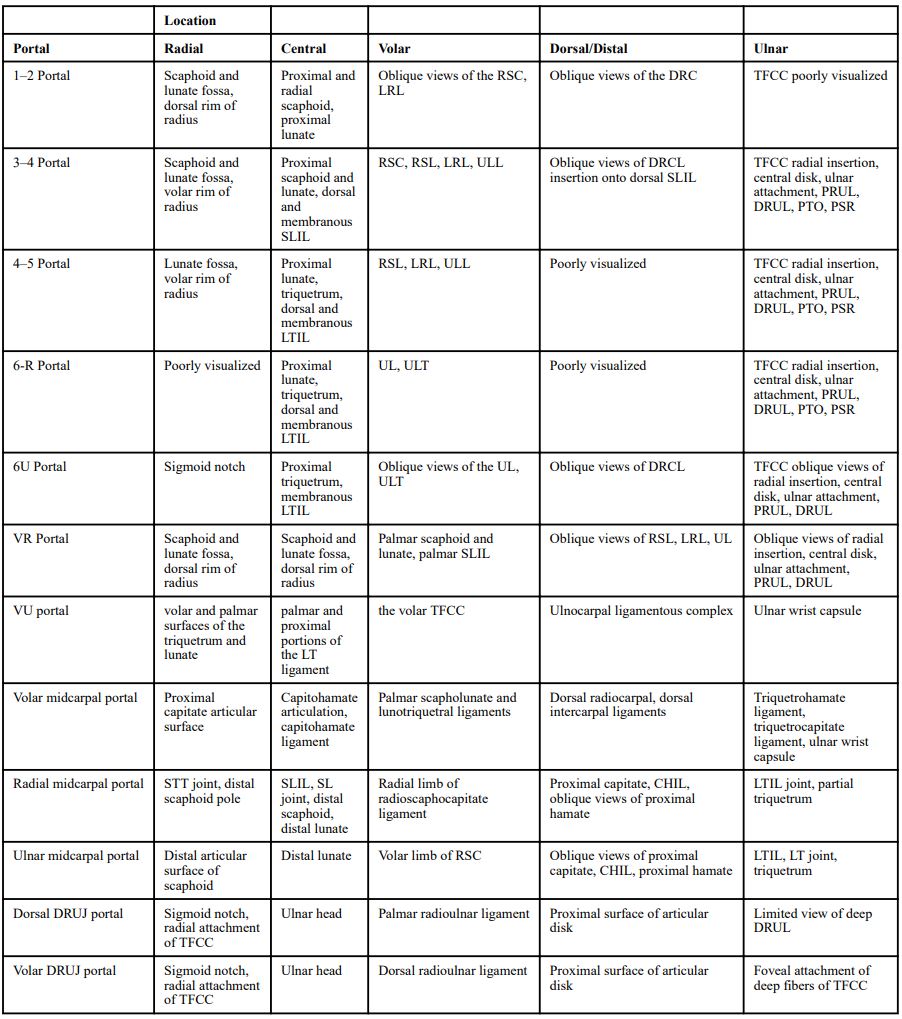
Anatomic structures by portal location
The dorsal portals are named for their relation to the extensor compartments: 3–4, 4–5, 6R, 6U, radial midcarpal, and ulnar midcarpal portals.Diagnostic Wrist ArthroscopyNew advances in wrist arthroscopy
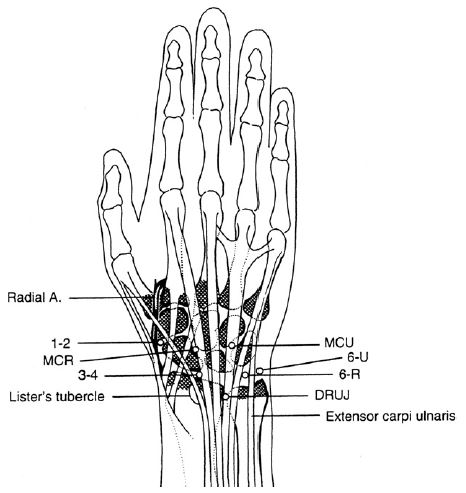
dorsal portals
Procedure
For classic diagnostic wrist arthroscopy, we use the 3/4 portal as the first access.
The portal is located approximately 1 cm distal to the tuberculum Lister in a softspot between the extensor pollicis longus (EPL) tendon and the extensor digitorum communis (EDC) tendons.Wrist arthroscopyDiagnostic Wrist Arthroscopy
We use a 20-gauge needle to probe the radiocarpal joint (approximately 10 degrees of inclination toward the hand). This is followed by a small skin incision in the area of the needle. An access to the joint can then be prepared along the needle with a mosquito clamp. Finally, the needle can be removed and the arthroscope can be carefully inserted with the trocar.
Once the arthroscope has been inserted, access can be made under visual control via the 4/5 or 6/R portal. The point of entry is the interval between the EDC and extensor digiti minimi (EDM) tendons. The inclination of the radius is normaly approximately 22 degrees, so the entry point for the 4–5 portal is slightly more proximal than the 3–4portal.Diagnostic Wrist Arthroscopy
CAVE: It is worth creating the ulnocarpal portal under arthroscopic view and using the inserted needle as a guide tool in order not to alter the TFCC, especially in ulna plus variance.
For the second / ulnocarpal portal we mostly use the 6R +/- 6 U
The portal is located approximately 1 cm distal to the tuberculum Lister in a softspot between the extensor pollicis longus (EPL) tendon and the extensor digitorum communis (EDC) tendons.Wrist arthroscopyDiagnostic Wrist Arthroscopy
We use a 20-gauge needle to probe the radiocarpal joint (approximately 10 degrees of inclination toward the hand). This is followed by a small skin incision in the area of the needle. An access to the joint can then be prepared along the needle with a mosquito clamp. Finally, the needle can be removed and the arthroscope can be carefully inserted with the trocar.
Once the arthroscope has been inserted, access can be made under visual control via the 4/5 or 6/R portal. The point of entry is the interval between the EDC and extensor digiti minimi (EDM) tendons. The inclination of the radius is normaly approximately 22 degrees, so the entry point for the 4–5 portal is slightly more proximal than the 3–4portal.Diagnostic Wrist Arthroscopy
CAVE: It is worth creating the ulnocarpal portal under arthroscopic view and using the inserted needle as a guide tool in order not to alter the TFCC, especially in ulna plus variance.
For the second / ulnocarpal portal we mostly use the 6R +/- 6 U

Acess 6R Portal with needle and smal clamp
Radiocarpal evaluation
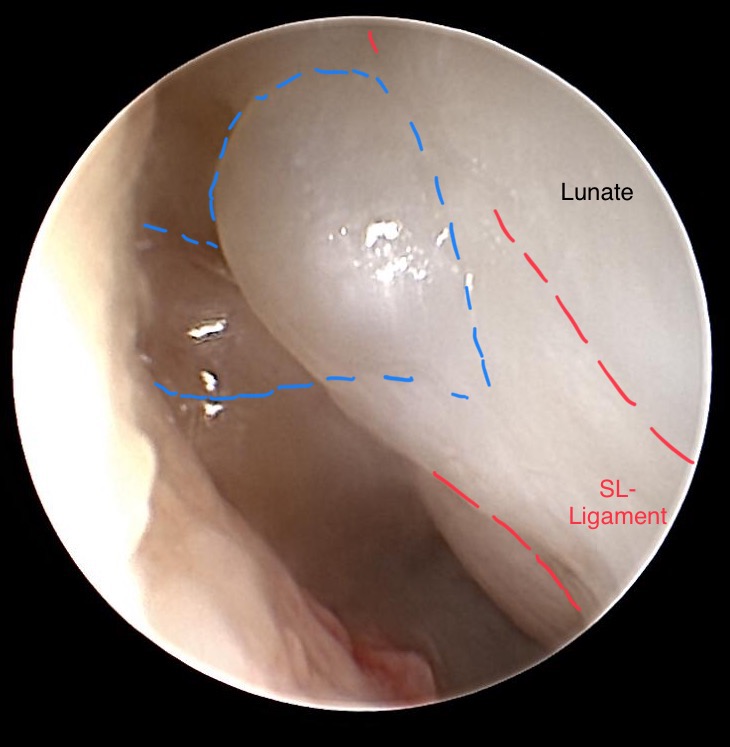
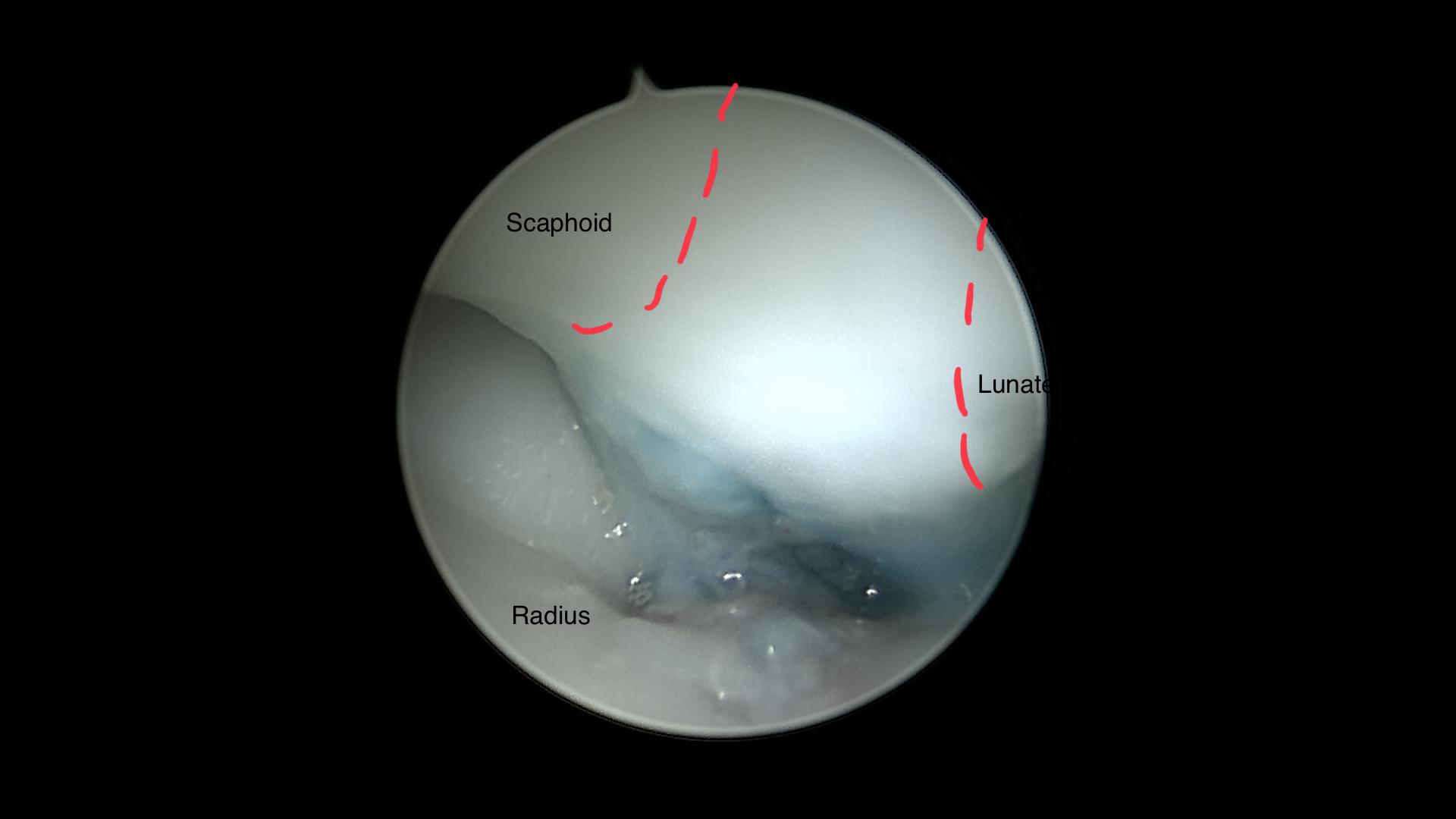
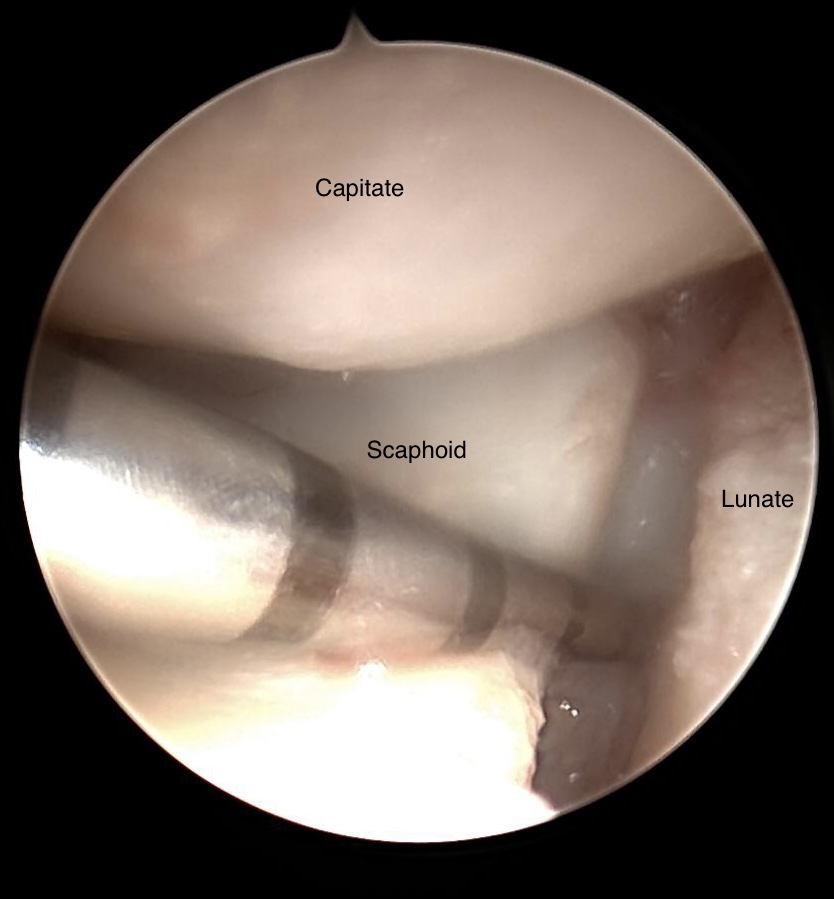
From the 3/4 portal, the surgeon is be able to view the proximal scaphoid, scapholunate ligament, lunate, and scaphoid fossa of the distal radius. The evaluation should begin from radial to ulnar.
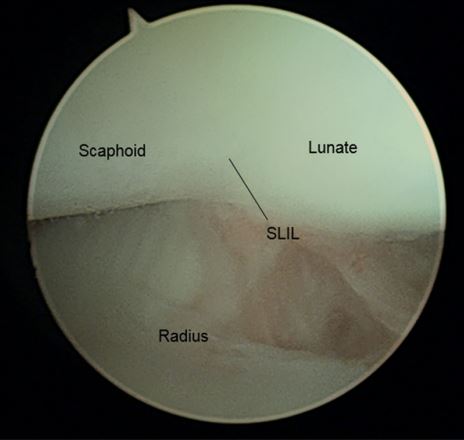
3-4 Portal, radiocarpal view
To view the radial styloid, proximal scaphoid articular cartilage, and scaphoid fossa the arthroscope is directed radially along the dorsal wrist capsule. From radial to ulnar the volar soft-tissue structures are, radioscaphocapitate ligament (RSC), long radiolunate ligament (LRL), short radiolunate ligament (SRL), and the radioscapholunate ligament (RSL) or ligament of Testut.Diagnostic Wrist Arthroscopy
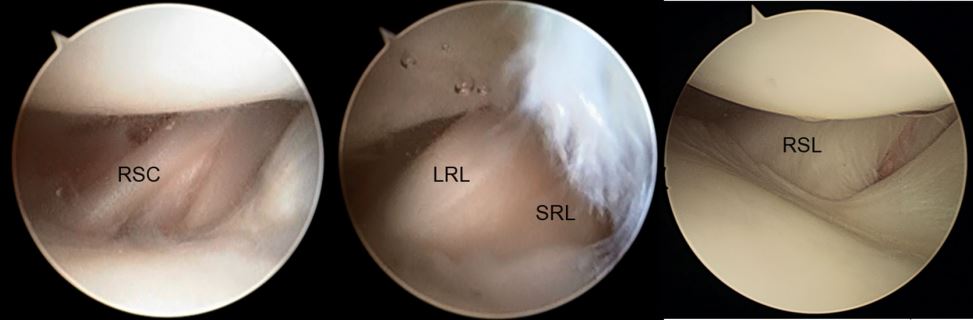
Volar/radial extrinsic ligaments. SRL, short radiolunate ligament
Centrally, at the top of the arthroscopic image,.the proximal membranous portion of the scapholunate (SL) ligament, and the dorsalscapholunate ligament can be visualized.Diagnostic Wrist Arthroscopy
An arthroscopic classification of carpal instability is shown in the following table.Arthroscopic management of scapholunate instability
An arthroscopic classification of carpal instability is shown in the following table.Arthroscopic management of scapholunate instability
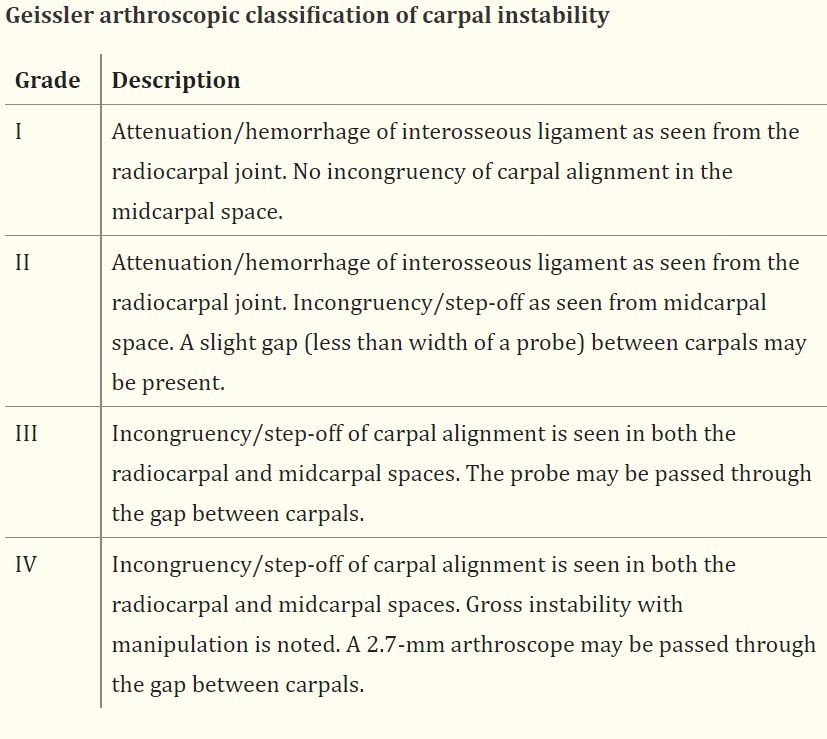
Geissler arthroscopic classification of carpal instability
The proximal articular cartilage of the lunate is evaluated for wear. On the distal radius the lunate fossa can be appreciated. Angling the scope toward the dorsal, ulnar wrist, the dorsal radio-carpal ligament can be inspected for injury. If necessary volar radial and ulnar portals can be used to evaluate the full extent of the palmar intercarpal ligaments and the dorsal capsular structures including the dorsal radiocarpal ligament.Diagnostic Wrist ArthroscopyClinical applications of volar portals in wrist arthroscopy
Advancing the scope ulnarly, the surgeon can eveluated the radial insertion of the triangularfibrocartilage complex (TFCC), the central disk, ulnar attachments, the palmar and dorsalradioulnar ligaments, the pisotriquteral orifice, and the prestyloid recess. A central perforation may be associated with an ulnocarpal impingement.Diagnostic Wrist Arthroscopy
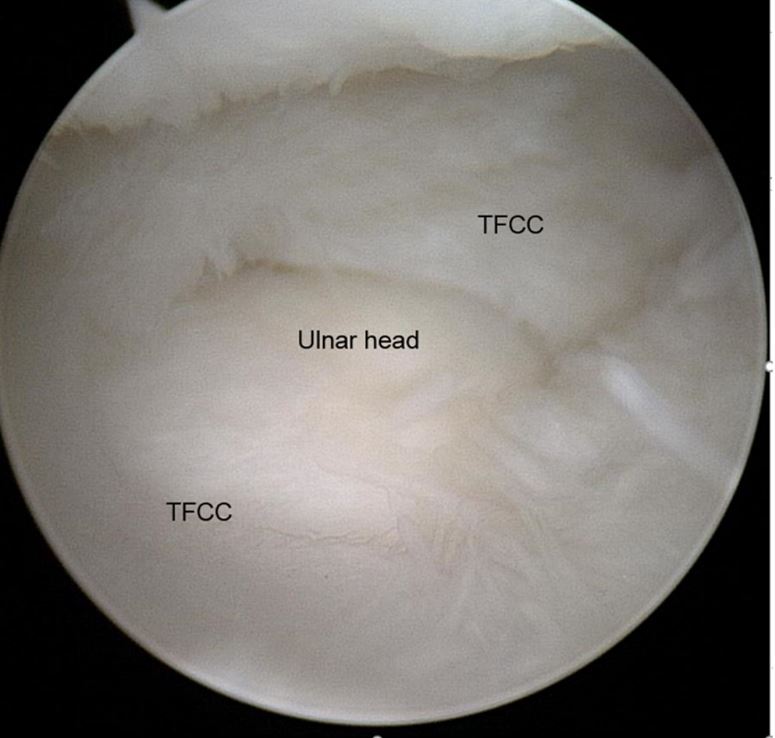
Central perforation of the TFCC
Via a 6R or 6U portal a hook probe canbe used to examine the integrity of the TFCC. A TFCC tear may be the cause of ulnar wrist pain. If instability is present with intact superficial PRUL and DRUL foveal attachments, DRUJ arthroscopy or arthrography may be warranted.Diagnostic Wrist Arthroscopy
TFCC disorders:Triangular fibrocartilage disorders: injury patterns and treatment
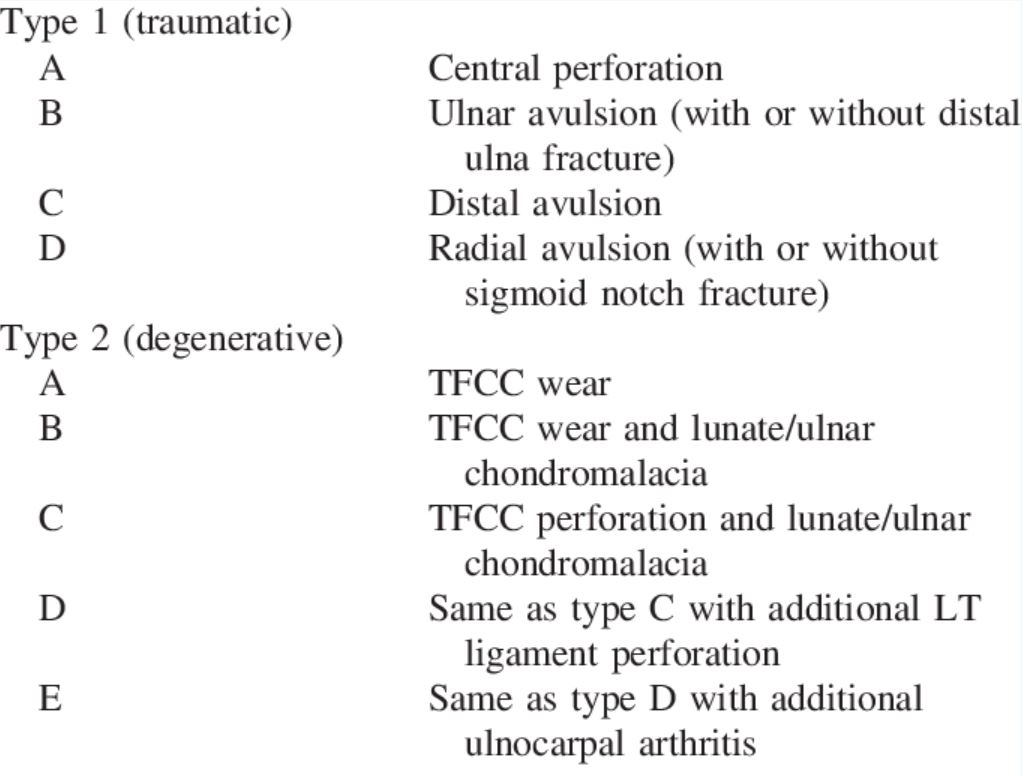
TFCC disorders (Palmer 1990)
The arhtroscope is then inserted into the 4/5 portal. It can be used to confirm the presence of lunate fossa articular wear, changes of the proximallunate, and injury/degeneration of the TFCC. This portal is also used to better visualize the proximal membranous and dorsal lunotriquetral interosseous ligament. Hemorrhage or attrition will cue the surgeon in to further evaluation from the midcarpaljoint.Diagnostic Wrist Arthroscopy
Midcarpal evaluation
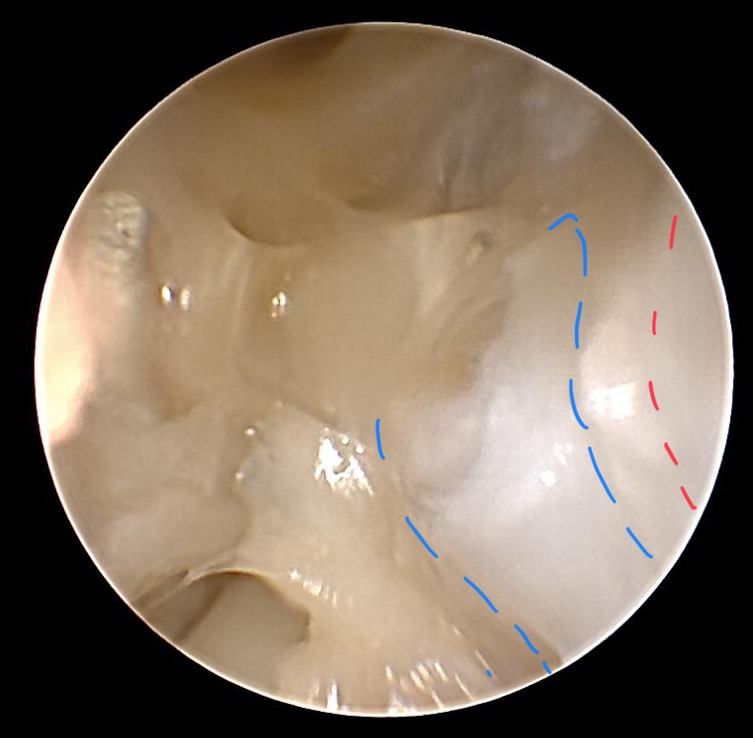
After the radiocarpal structures have been evaluated, the midcarpal approach is made. Through these portals (MCR, MCU), Injuries to the scapholunate or lunotriquetral ligamentscan be further classified.
Access is made as described above, also with a needle and a small clamp approximately 1 cm distal to the 3/4 portal.
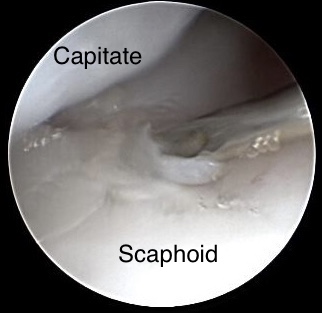
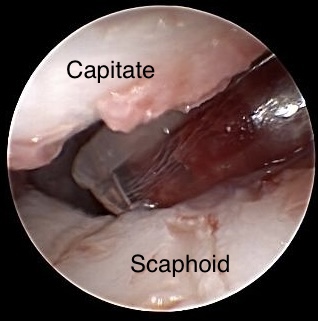
When the arthroscope is correctly, the surgeon should see the proximal capitate at the top of the image. The scaphocapitate joint and capitolunate joints can be seen. As the arhtroscope is directed radially, you can evaluate the scapho-trapeziotrapezoid joint and the distal scaphoid pole for articular changes.Diagnostic Wrist Arthroscopy
Access is made as described above, also with a needle and a small clamp approximately 1 cm distal to the 3/4 portal.
When the arthroscope is correctly, the surgeon should see the proximal capitate at the top of the image. The scaphocapitate joint and capitolunate joints can be seen. As the arhtroscope is directed radially, you can evaluate the scapho-trapeziotrapezoid joint and the distal scaphoid pole for articular changes.Diagnostic Wrist Arthroscopy
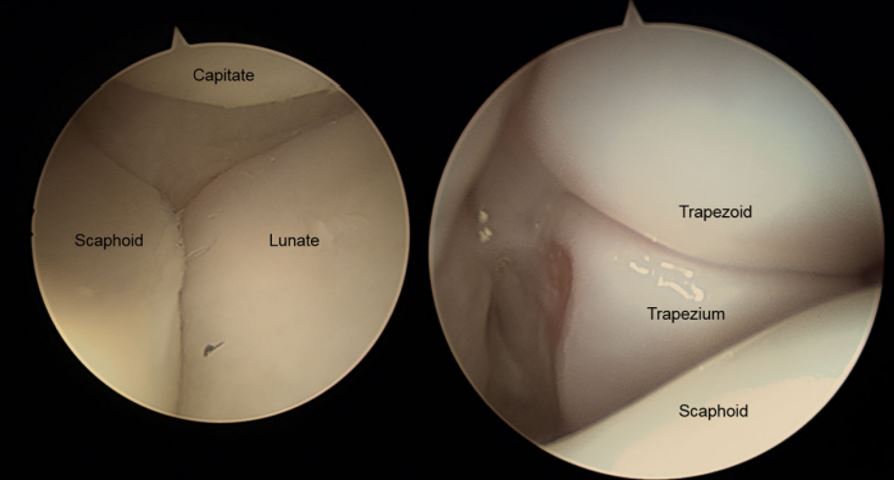
Midcarpal view (left: view on SL; right: view on STT)
From this point of view, a ligament injury can be classified according to Geissler. If the arhtroscope can pass between the bones,(>2.7mm gap.) it is a grade 4 instability according to Geissler. Otherwise, the probe should be used to check the grade of instability.
The radial limb of the RSC ligament can be inspected for injury vorarly.
Ulnarly, the proximal capitate, capitohamate articulation, and lunotriquetraljoint can be evaluated.Diagnostic Wrist Arthroscopy
The ulnar midcarpal portal is entered 1 cm distal to the 4–5 portal. The articular surfaces of the distal scaphoid, lunate, and triquetrum, and proximalcapitate, and hamate can again be inspected for articular wear ro gangings. Thris portal can be also used to visualizing a lunotriquetral (LT) instability.Diagnostic Wrist Arthroscopy
The radial limb of the RSC ligament can be inspected for injury vorarly.
Ulnarly, the proximal capitate, capitohamate articulation, and lunotriquetraljoint can be evaluated.Diagnostic Wrist Arthroscopy
The ulnar midcarpal portal is entered 1 cm distal to the 4–5 portal. The articular surfaces of the distal scaphoid, lunate, and triquetrum, and proximalcapitate, and hamate can again be inspected for articular wear ro gangings. Thris portal can be also used to visualizing a lunotriquetral (LT) instability.Diagnostic Wrist Arthroscopy
Cartilage alteration
Any cartilage alteration should be described using the Outerbridge classification.Wrist arthroscopy: indications, portal anatomy and therapeutic advances, Orthopaedics and Trauma
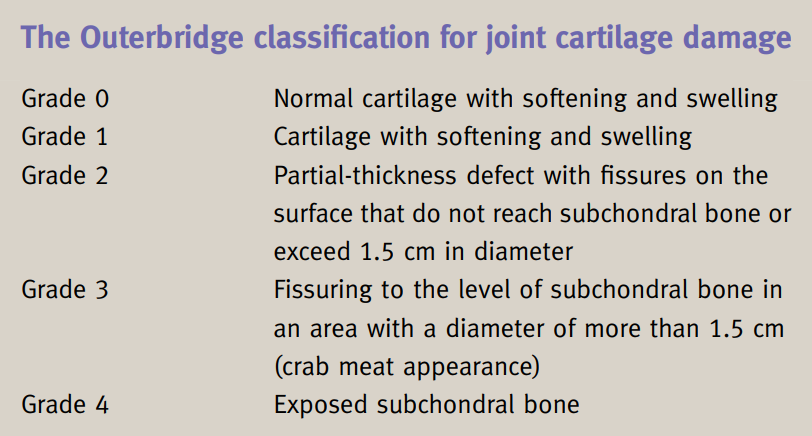
Outerbridge classification
04
Indication
Indication
When determining the indication, a fundamental distinction should be made between traumatic (acute) and degenerative (chronic).
Traumatic (acute) alterations
In the case of a traumatic injury, the indication for surgery is usually given early. Abnormalities in the examination, X-ray or CT are indicative for the treatment.
Indications for early elective surgery includeHandgelenksarthroskopie
Indications for early elective surgery includeHandgelenksarthroskopie
ligamentary injuries
dislocated intraarticular radius fracturesHandgelenksarthroskopie
Arthroscopy should be indicated for B and C radius fractures, especially sa gital fractures.
Degenerativ (chronic) alterations
Conservative therapy can be successful for chronic wrist pain. For example, ergotherapy, temporary immobilization or pain medication can be used. If conservative therapy fails, further diagnostics should be performed. An MRI examination is usually chosen for this purpose.
Indications for wirst arthroscopy in chronic complaints areHandgelenksarthroskopie
Indications for wirst arthroscopy in chronic complaints areHandgelenksarthroskopie
unclear wrist pain
carpal instability
joint blockages
Synovial hypertrophy
chondral lesion
Algorhythm
The following algorhythm shows the different paths for various disorders.
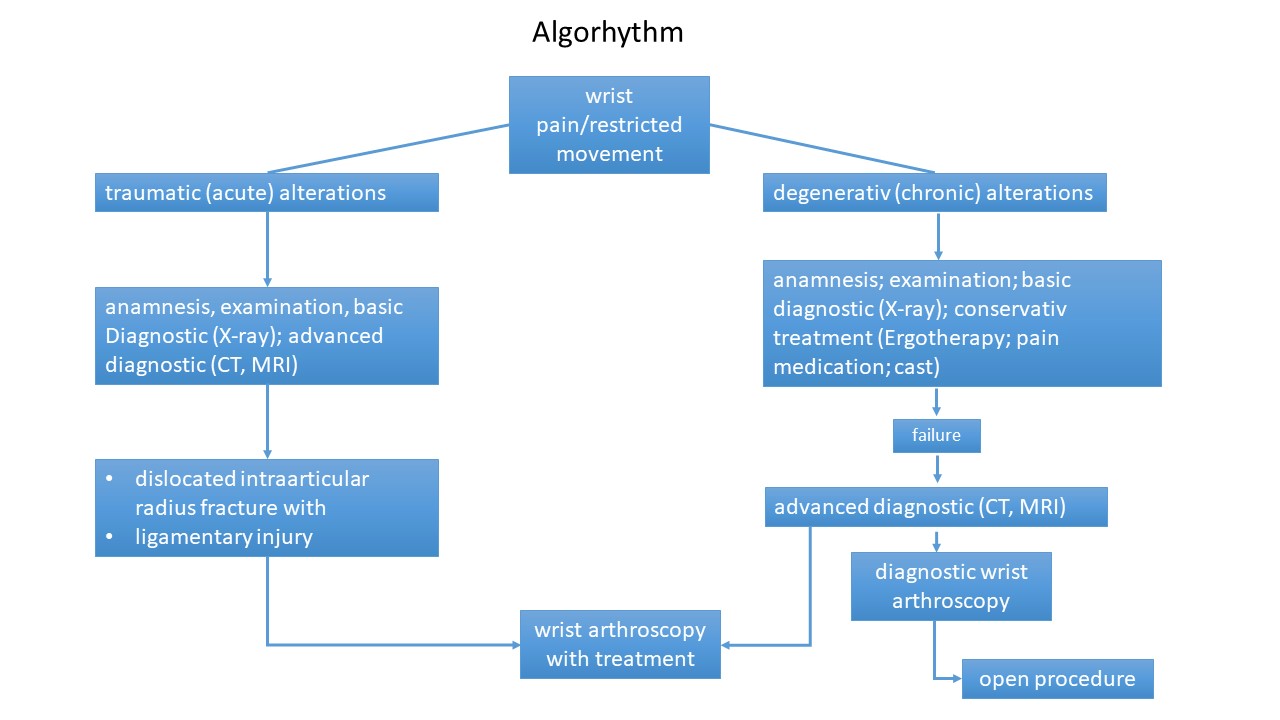
Algorhythm - from pain to treatment
05
Examples
In the following subchapters different cases from our clinic are presented. For this purpose, intraoperative images are presented descriptively.
06
Arthroscopic treatment of dorsal wrist cyst
25 y, female
no traumatic anamnesis
therapy resistant pain caused by a clinically evident dorsal wrist cyst
no traumatic anamnesis
therapy resistant pain caused by a clinically evident dorsal wrist cyst
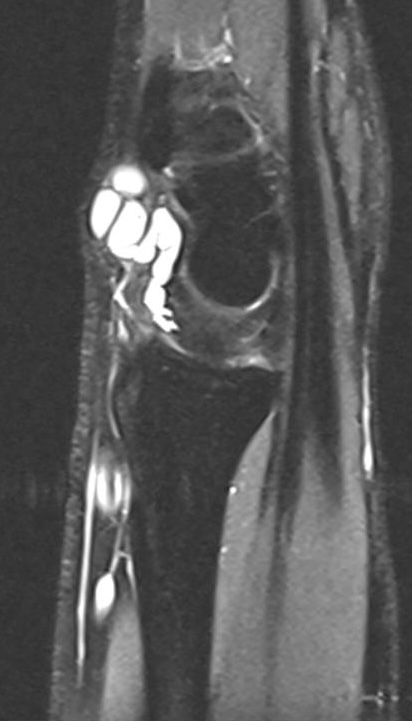
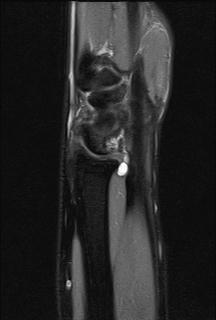
MRI of dorsal wrist cyst
In sagittal view the slide almost runs through the SL-joint space. The „fluid“origin of the wrist cyst is well detectable.

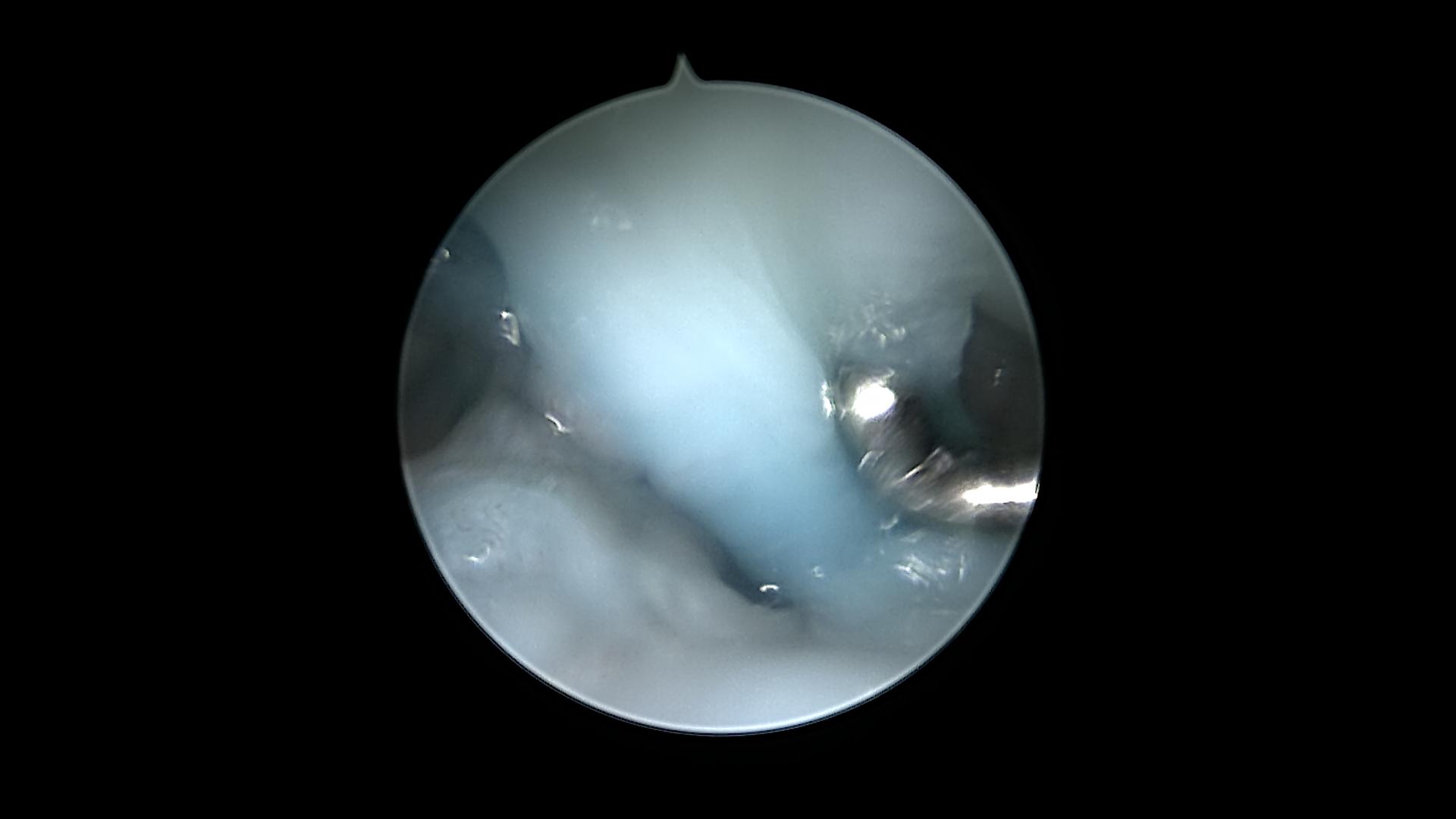
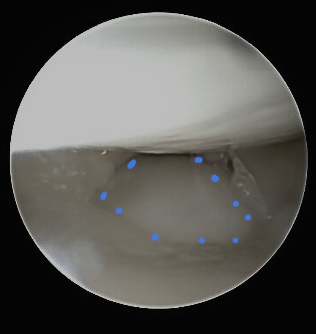
Ulnocarpal view on SL-Ligament
The integrity of SL ligament evaluated via probe, coming from 3/4 portal.
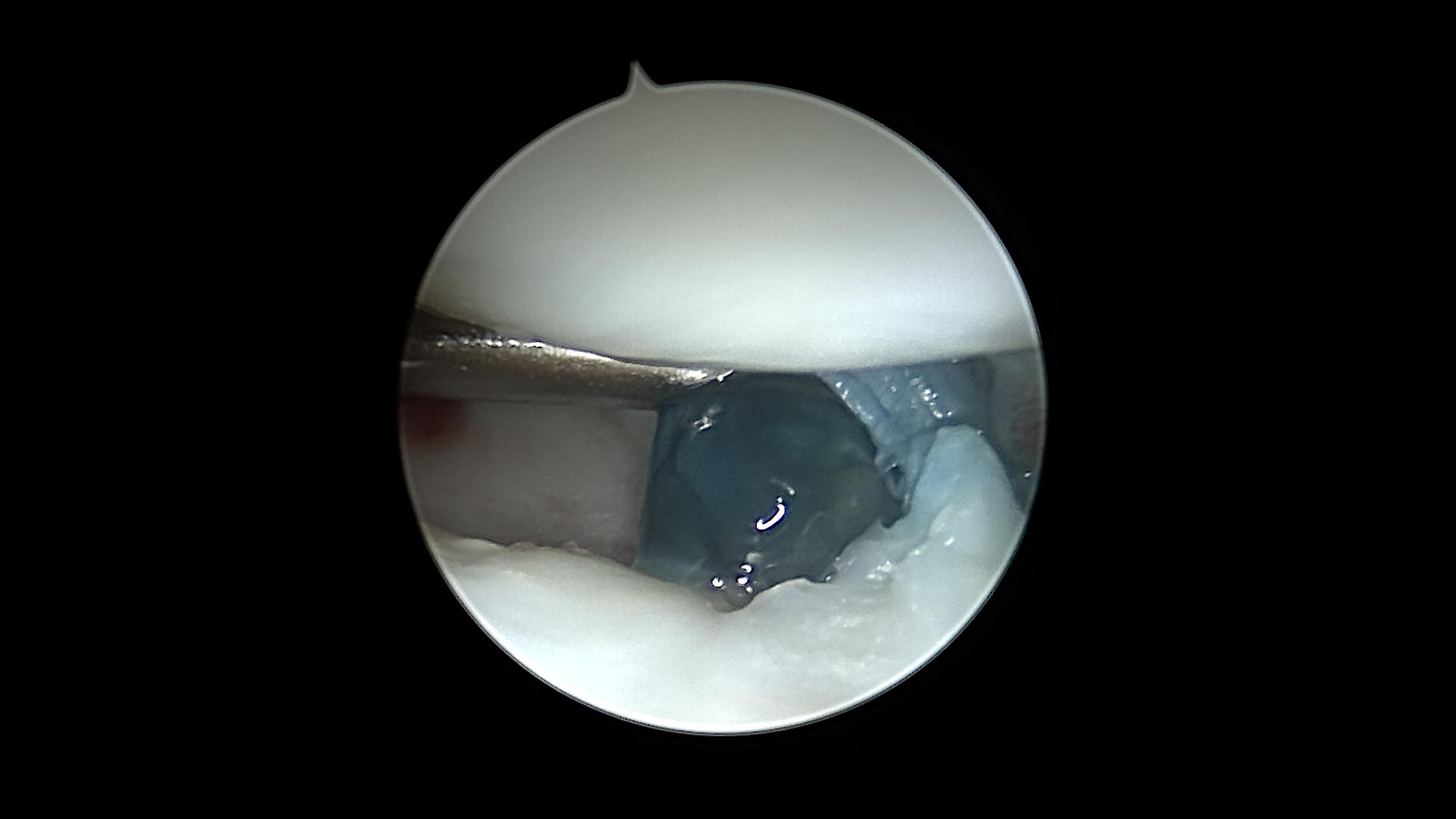
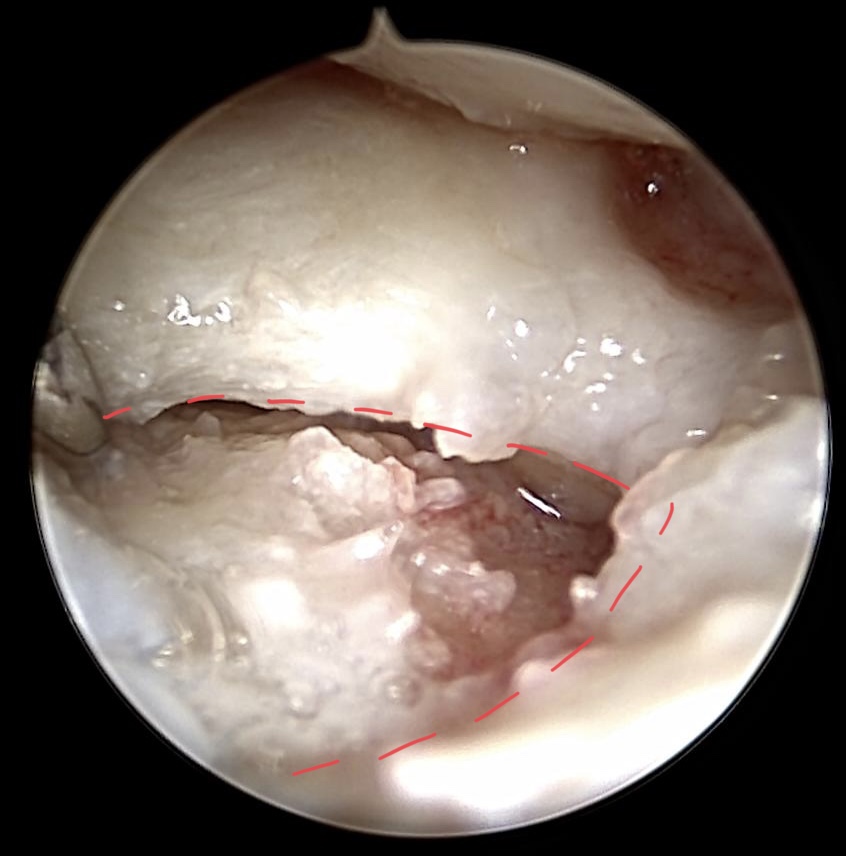
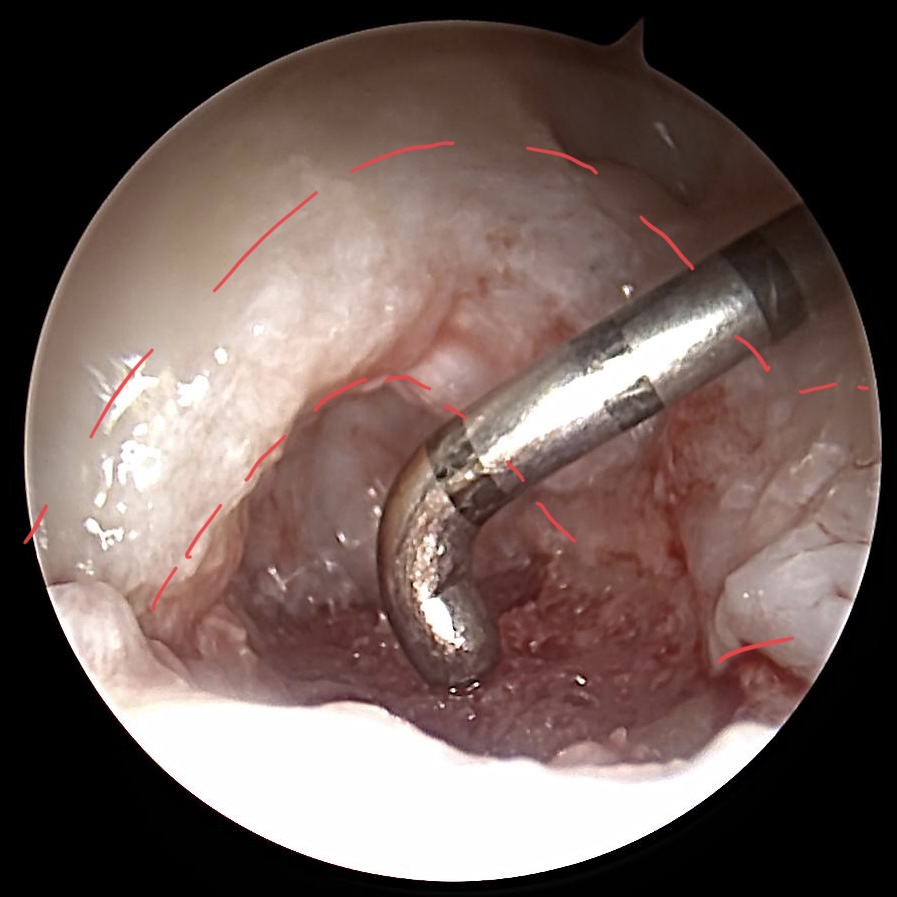
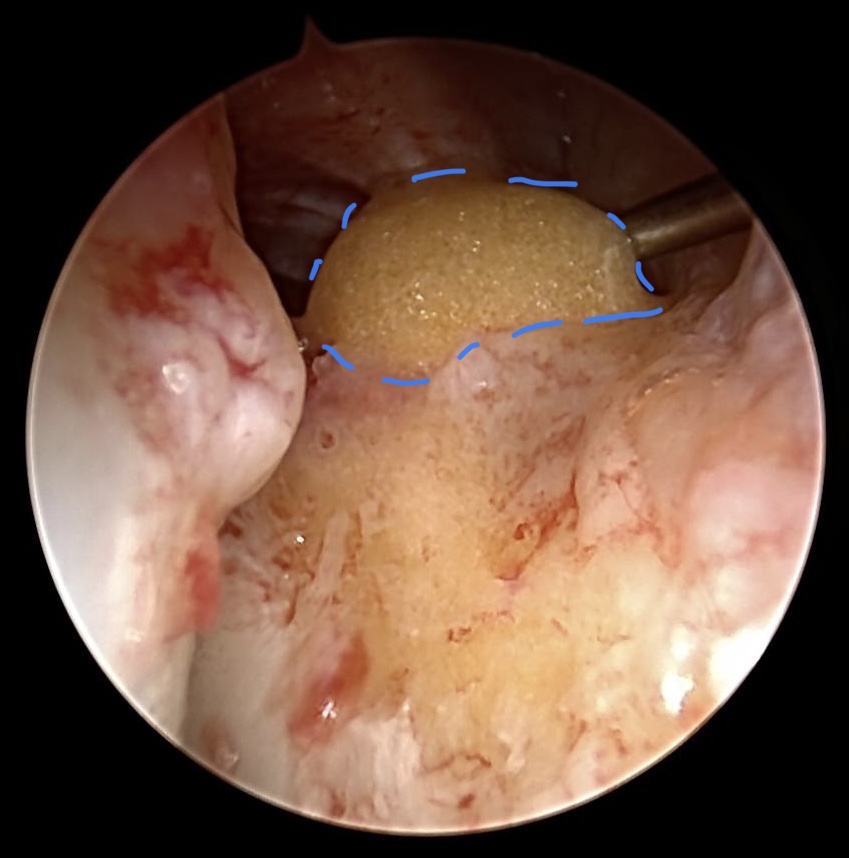
Dorsal wrist cyst with its origin from the SL-Ligament
(Scope coming from 6R) Following the most dorsal part of SL ligament detection of the cyst (blue) with its origin from the SL-ligament (red dotted lines) is performed
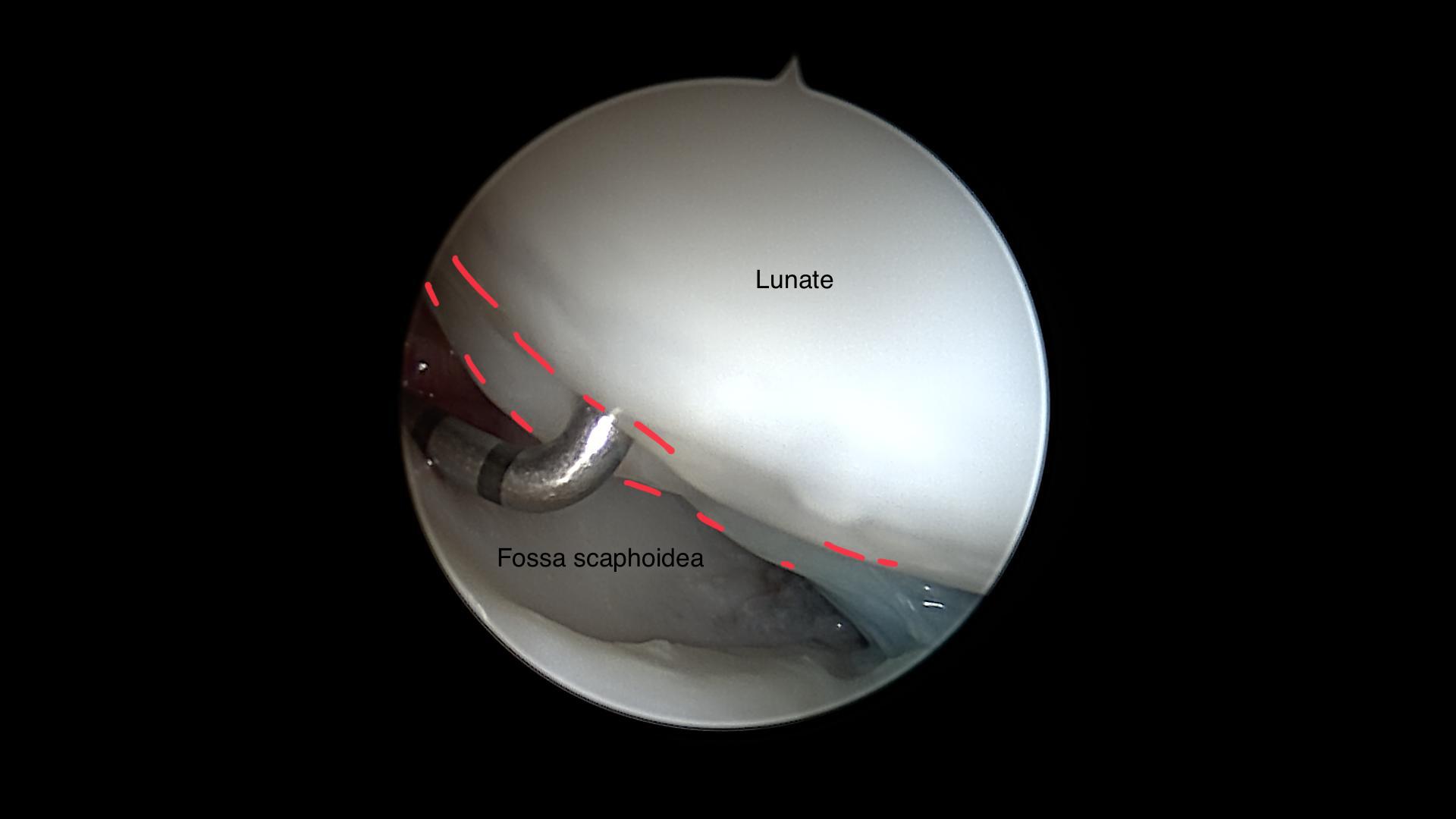
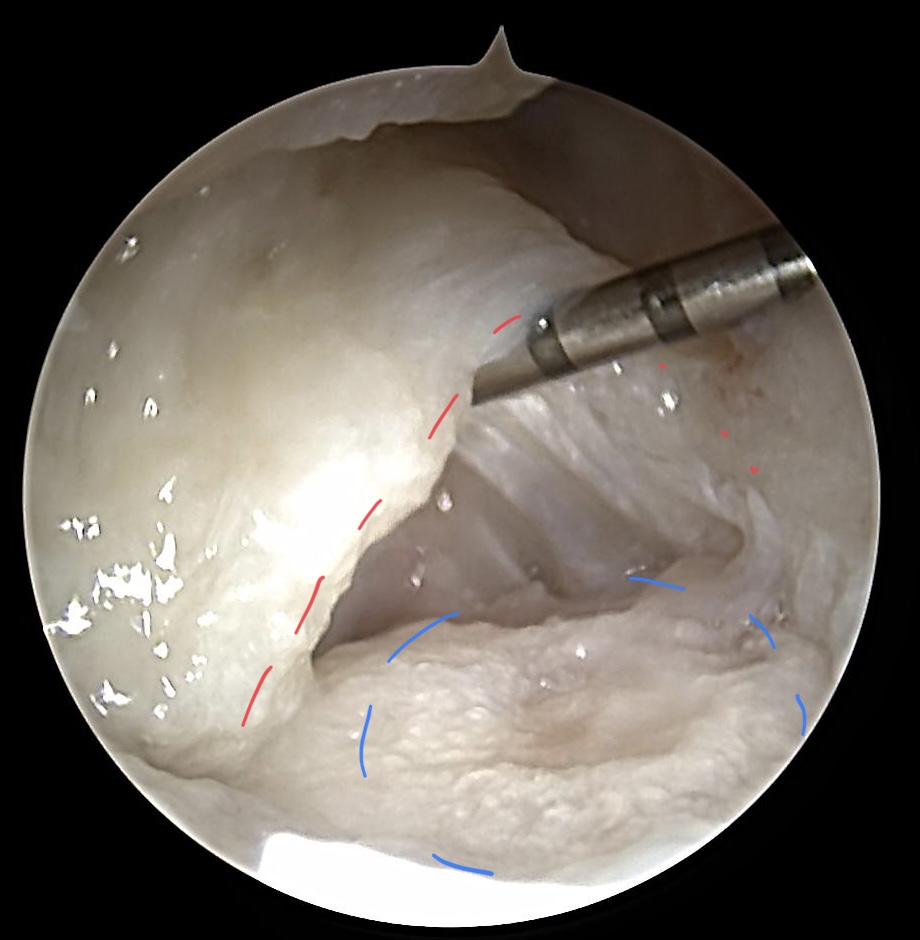
Resected wrist cyst
The pedicle of the wrist cyst (blue) was resected via shaver. The most dorsal aspect of the SL-ligament is marked with the red dotted line. In the middle of the image residual gel-like (mucin) liquid is visible. Creating a window in the dorsal wrist capsule to avoid recurrence of the cyst.
07
Arthroscopic treatment of volar wrist cyst
20 y, female
no traumtic anamnesis
failured conservative treatment
MRI detected volar wrist cyst
no traumtic anamnesis
failured conservative treatment
MRI detected volar wrist cyst
Sagittal view of a volar wrist cyst
Ulnocarpal view of the SL-ligament an the volar aspect of the blue dyed cyst
Before surgery the cyst was Ultrasound guided dyed with Patent Blue ®
Detection of the volar wrist cyst (dyed with Patent blue)
Arthroscopic dissection of the blue dyed cyst
Dyed gel-like liquid entering after dissection the cyst
It‘s important to create a window in the volar capsule to avoid a recurrence of the cyst.
08
Arthroscopic treatment of the TFCC
Arthroscopic evaluation of the TFCC includes especially the Hook test and the trampoline phenomenon. The Hook test indicates stability of the distal radio-ulnar joint (DRUJ). The Trampoline test is less reliable for foveal detachment of the TFCC. Central tears should be resected, especially in degenerative cases. Typically ulna plus variance can be reason for a painful degenerativ central tear +/- osteoarthroses or LT-ligament instability.
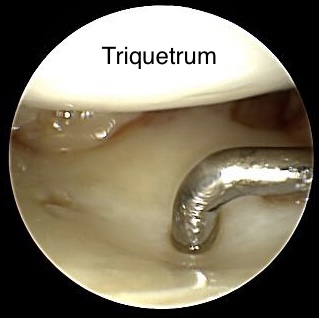
Hook test for testing normal or abnormal detachment of the TFCC
The image shows a tight Hook test for normal DRUJ stability. Anyway there a synovial hypertrophic alterations (red dotted lines) which will be resected with a shaver after evaluation of the wrist is performed.
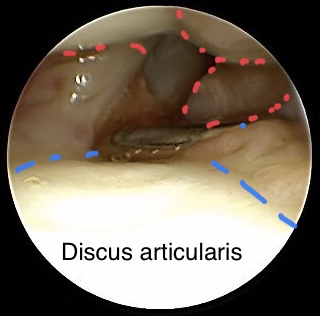
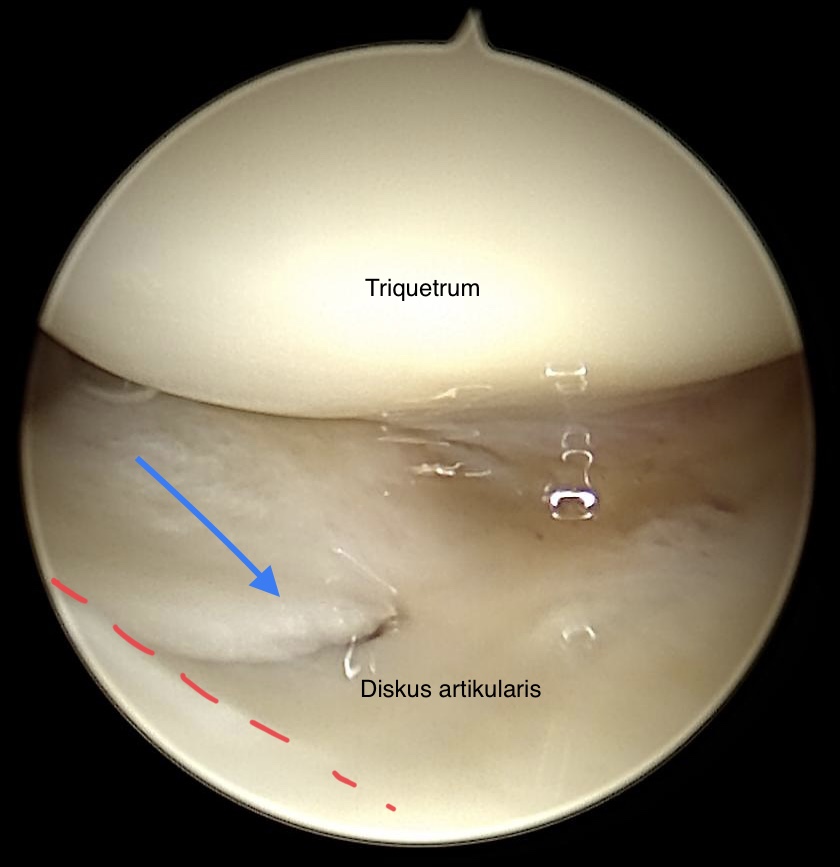
Normal „trampoline phenomenon“ on the discus articularis
As shown in the image a normal Trampoline test is performed although there is a very small tear in the volar part of the discus articularis. Cartilage of the Triquetrum doesn‘t show any alterations. (Scope is coming from the 3/4 portal)
Chronic traumatic tear (blue arrow) close to the radial border (red dotted line)
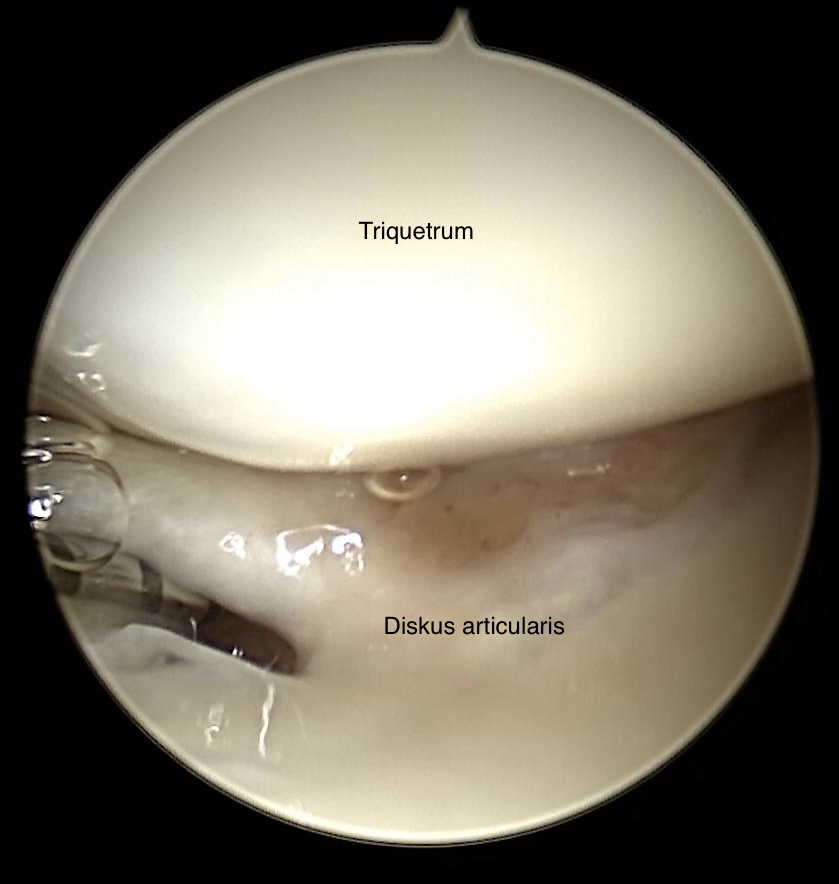
Old traumatic tear of the discus articularis
Again radiocarpal view on the TFCC with bigger tear (Typ 1 a according the Palmer classification) in the discus articularis. Cartilage shows no alteration.
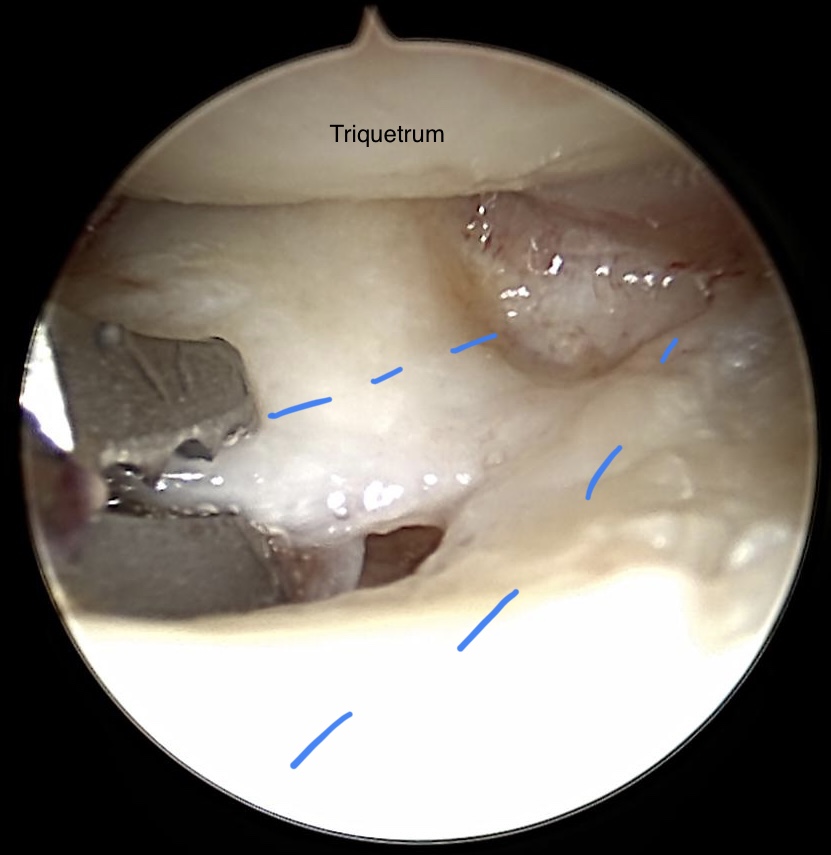
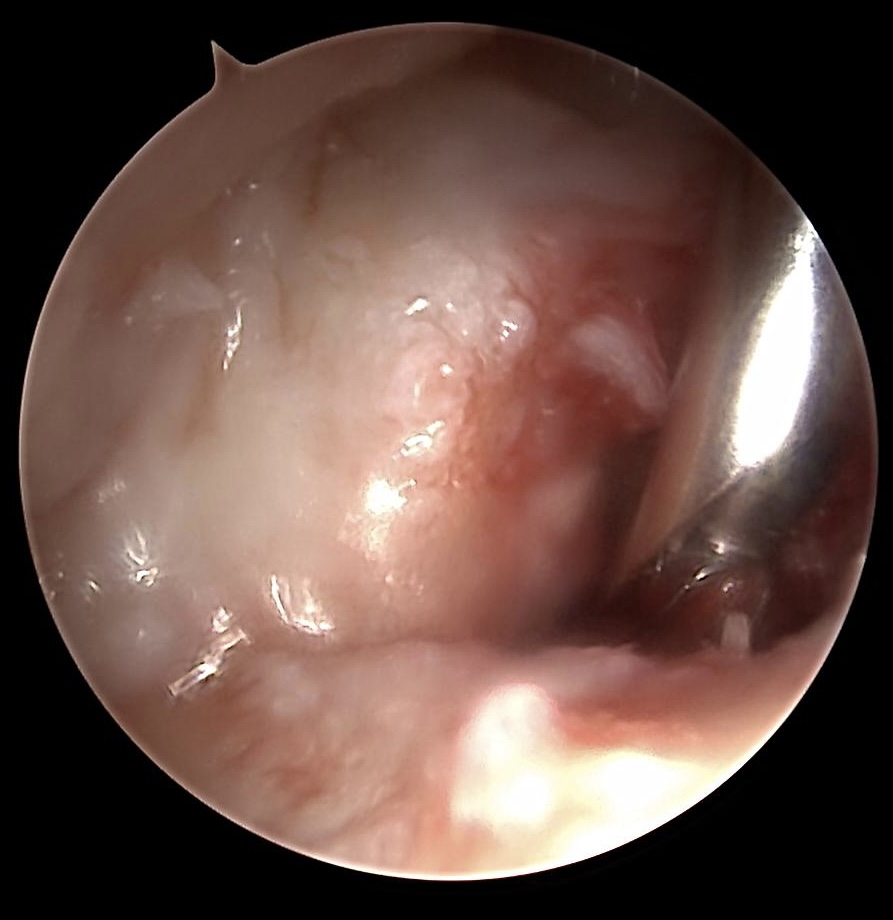
Debridement of the discus articularis (blue dotted lines)
Radiocarpal view on TFCC after debridement
Cartilage of the Triquetrum shows minor defects (2-3 degree according to the Outerbridge classification). Degenerativ tears, Typ 2d lesion (Palmer), are resected with a punch forceps. Osteoarthrosis of the ulna head becomes evident. The red dotted line indicates the volar and dorsal part of the radio-ulnar ligaments.
09
Arthroscopic management of ulna impaction syndrom
Ulna impaction syndrome is caused by an ulna plus variance. Most important is the clinical investigation and a good distinction to Morbus Kienböck. MRI and X-Ray is an elementary diagnostic tool.
Congenital ulna plus variance
Zentral TFCC lesion in ulna plus variance
This central lesion of the TFCC was evaluated by chance and did not provoque any pain for this 20 y old patient. She was arthroscopically treated due to a wrist cyst. From radiocarpal view the ulna head with intact cartilage (blue dotted line) „perforates“ the discus articularis., Most likely the discus has never been completely developed.
40 y female
ulnocarpal wrist pain
no trauma
ulnocarpal wrist pain
no trauma

Ulna impaction syndrom
The ulna head is clearly to long in relation to the radiocarpal joint surface. Due to the pressure degenerative cysts in the Lunatum became evident. Indication for arthroscopy is given.

Degenerative alterations of the TFCC in ulna impaction syndrome
Central degenerativ avulsion of the TFCC without any osteoarthrosis og the ulna head

Debridement of the degenerative discus articularis
It is worth trying to reduce ulnocarpal wrist pain by debridement of the TFCC. If pain proceeds longer than 3 months after arthroscopic treatment we recommend ulna-shortening osteotomy.

Ulnar shortening osteotomy due to ulna impaction syndrom
63 y, female
Exacerbated ulnocarpal wrist pain
arthroscopic debridement 5 years ago (evaluated Typ 2 D/E lesion according to Palmer)
Exacerbated ulnocarpal wrist pain
arthroscopic debridement 5 years ago (evaluated Typ 2 D/E lesion according to Palmer)

MRI with degenerative lesion of the lunate and ulna head
Text
Radiocarpal view on TFCC after resection of the discus articularis 5 years ago
The red dotted line indicates the volar radioulnar Ligament (RUL), well attached to the fovea ulnaris. Due to the ulna plus variance DRUJ is commonly more lax in clinical investigation. The blue dotted line indicates the proceded region of osteoarthrotic changes of the ulna head.
Wafer procedure of the ulna head
Wafer procedure of the ulna head
We‘re use a 3 mm burr to dissect the ulna head. During wafer procedure we switch from „dry“ to „wet“ arthroscopy. The RUL (red dotted line) must be preserved.

X-Ray after wafer procedure
The impaction zone is reduced. The patient has to wear a cast for 2 weeks. On the one hand for pain reduction and on the other hand to preserve the postoperative clot on the ulna head in order to promote a scar tissue replacing the ulna head cartilage.
10
STT osteoarthrosis
Osteoarthrosis of the Scapho-trapezo-trapezoidal joint (STT) is commonly associated with proceeded basilar thumb arthrosis. This often leads to open surgery procedures. Rarely STT arthrosis is isolated. We mostly treat these cases joint preserving with the combination of debridement and lipo-filling. Pain at rest and at stress is often well reduced.
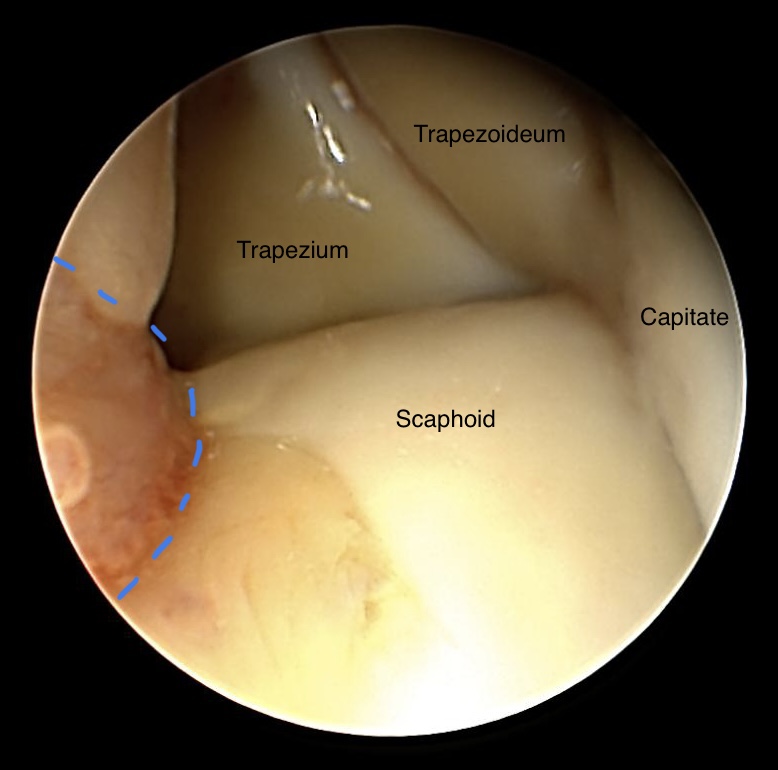
Radiomediocarpal view on STT joint
Normal aspects of a STT joint in young male patient after accident. Only small parts of synovial alterations have been detected (blue dotted line)

Isolated STT osteoarthrosis
X-ray made due to radiocarpal wrist pain in 82 y male patient. Moreover degenerative aspects in the Lunataum, the space between scaphoid und radial styloid. Clinically the radiocarpal pain over the basilar thumb was dominating the problems. Indication for arthroscopy was given.
STT osteoarthrosis combined with SL ligament instability
During diagnostic arthroscopy SL ligament instability was evaluated. 3-4° according to Geissler.
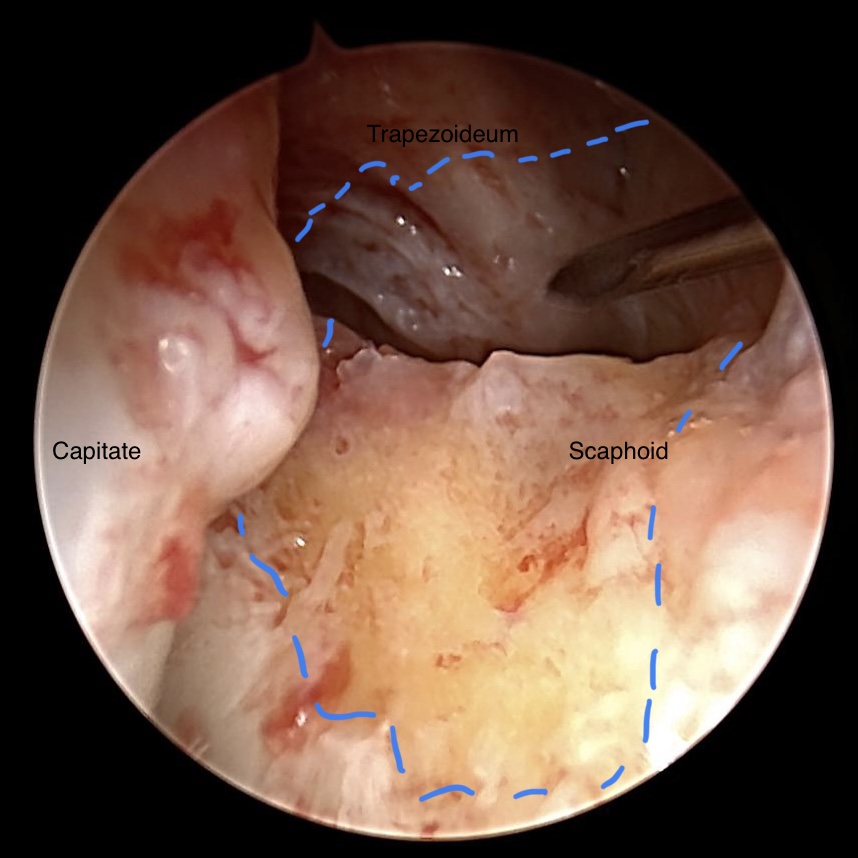
STT joint osteoarthrosis after debridment
Lipo filling in cases of STT joint arthrosis
The SL ligament instability was not treated because of higher SLAC-wrist . The patient wished a joint preservation. That‘s why we performed the lipofilling (blue dotted line),.
11
Arthroscopic treatment of Scaphoid non-union
26 y, male
Trauma took place more then 1,5 y ago
Exacerbation of pain in adominant left wrist
X-Ray and CT reveal a Scaphoid non-union
Trauma took place more then 1,5 y ago
Exacerbation of pain in adominant left wrist
X-Ray and CT reveal a Scaphoid non-union

Scaphoid non-union

CT: Scaphoid non-union
Ulnomediocarpal view of Scaphoid non-union
Diagnostic arthroscopy shows normal cartilage und no ligamentary alteration. Indication for simultaneous repair of the Scaphoid non-union is given. In the image above the non-union is incised with a sharp needle entered via RMC portal.

Arthroscopic resection of the Scaphoid non-union

Completed resection of the non-union region
Resecting the Scaphoid non-union we alternating use shaver, sharp spoon and a dentist hook. A burr can be useful as well.

Released Tourniquet reveals vital bony tissue
After arthroscopic resection of the non-union side it is worth to open shortly the Tourniquet in order to evaluate vitality of bony tissue.

Percutaneous reduction with guiding wire and anti-rotation wire
Linscheid manoeuvre (not shown) is sometimes necessary to obtain adequate reposition. In principle 2-3 K-wire is a sufficient reduction, especially for non-unions in the very proximal part of the Scaphoid. Anyway we prefer orthograde or anterograde inserted compression screw.
Placing cancellous bony tissue
Having placed 2 K-wires, cancellous bone craft, harvested from iliac crest, is cutted in small pieces. Bony tissue is collected for transfer in a needles cap, which can easily inserted via RMC portal. The end of this cap is cut off so that bony tissue can pushed out , e. g. with a K-wire, into resected region.

Transfered bone graft

Modulated and compressed bone graft after having inserted compression screw
Final arthroscopic survey in order to exclude intraarticular placed screw or displaced bony tissue should be performed. In very large defects after resecting non-union side, it can be useful entering via 3/4 portal a child urine catheter avoiding dislocation of bony tissue into the radiocarpal joint space when inserting via RMC portal the bone graft.

Consolidation of the Scaphoid non-union
After surgery patients have to wear consequently a circular cast including the first ray (without the IP-joint). CT is performed 8 weeks after surgery, if there is any doubt in bony healing cast can‘t be removed. CT is repeated 4-6 weeks later.
CAVE: Arthroscopic treatment of Scaphoid non-unions doesn‘t replace open surgery treatment. It is not a beginners tool, but the learning curve is steep.
Images
Set-up with 90° at elbow joint
Anatomic structures by portal location
3-4 Portal, radiocarpal view
Volar/radial extrinsic ligaments. SRL, short radiolunate ligament
dorsal portals
Portale 3D
Portals with technique and comments
Geissler arthroscopic classification of carpal instability
Central perforation of the TFCC
TFCC disorders (Palmer 1990)
Midcarpal view (left: view on SL; right: view on STT)
Instruments
Acess 6R Portal with needle and smal clamp
Ulnocarpal view on SL-Ligament
Dorsal wrist cyst with its origin from the SL-Ligament
Resected wrist cyst
Algorhythm - from pain to treatment
MRI of dorsal wrist cyst
Sagittal view of a volar wrist cyst
Ulnocarpal view of the SL-ligament an the volar aspect of the blue dyed cyst
Arthroscopic dissection of the blue dyed cyst
Arthroscopic view on the volar wrist cyst (dyed with Patent Blue®)
During dissection of the cyst blue dyed, gel-like liquid enters the joint
Debridement of the discus articularis (blue dotted lines)
Normal „trampoline phenomenon“ on the discus articularis
Chronic traumatic tear (blue arrow) close to the radial border (red dotted line)
Old traumatic tear of the discus articularis
Hook test for testing normal or abnormal detachment of the TFCC
Zentral TFCC lesion in ulna plus variance
Radiocarpal view on TFCC after debridement
Ulna impaction syndrom
Debridement of the degenerative discus articularis
Degenerative alterations of the TFCC in ulna impaction syndrome
Ulnar shortening osteotomy due to ulna impaction syndrom
MRI with degenerative lesion of the lunate and ulna head
Radiocarpal view on TFCC after resection of the discus articularis 5 years ago
Wafer procedure of the ulna head
Wafer procedure of the ulna head
X-Ray after wafer procedure
SL instability 3-4° according to Geissler
STT joint osteoarthrosis after debridment
Lipo filling in cases of STT joint arthrosis
Isolated STT osteoarthrosis
Radiomediocarpal view on STT joint
STT osteoarthrosis combined with SL ligament instability
Outerbridge classification
Scaphoid non-union
CT: Scaphoid non-union
Ulnomediocarpal view of Scaphoid non-union
Arthroscopic resection of the Scaphoid non-union
Completed resection of the non-union region
Released Tourniquet reveals vital bony tissue
Percutaneous reduction with guiding wire and anti-rotation wire
Consolidation of the Scaphoid non-union
Placing cancellous bony tissue
Transfered bone graft
Modulated and compressed bone graft after having inserted compression screw
Videos
Access 6R potal
References
[1]
Dry wrist arthroscopy, Jones CM, Grasu BL, Murphy MS, J Hand Surg Am, 2015
[2]
Diagnostic Wrist Arthroscopy, Michelotti BF, Chung KC, Hand Clin, 2017
[3]
Diagnostic Wrist Arthroscopy, Michelotti BF, Chung KC, Hand Clin, 2017
[4]
Diagnostic Wrist Arthroscopy, Michelotti BF, Chung KC, Hand Clin, 2017
[5]
New advances in wrist arthroscopy, Bain GI, Munt J, Turner PC, Arthroscopy, 2008
[6]
Wrist arthroscopy, Chloros GD, Shen J, Mahirogullari M, Wiesler ER, J Surg Orthop Adv, 2007
[7]
Diagnostic Wrist Arthroscopy, Michelotti BF, Chung KC, Hand Clin, 2017
[8]
Diagnostic Wrist Arthroscopy, Michelotti BF, Chung KC, Hand Clin, 2017
[9]
Diagnostic Wrist Arthroscopy, Michelotti BF, Chung KC, Hand Clin, 2017
[10]
Diagnostic Wrist Arthroscopy, Michelotti BF, Chung KC, Hand Clin, 2017
[11]
Arthroscopic management of scapholunate instability, Geissler WB, J Wrist Surg, 2013
[12]
Diagnostic Wrist Arthroscopy, Michelotti BF, Chung KC, Hand Clin, 2017
[13]
Clinical applications of volar portals in wrist arthroscopy, Slutsky DJ, Tech Hand Up Extrem Surg, 2004
[14]
Diagnostic Wrist Arthroscopy, Michelotti BF, Chung KC, Hand Clin, 2017
[15]
Diagnostic Wrist Arthroscopy, Michelotti BF, Chung KC, Hand Clin, 2017
[16]
Triangular fibrocartilage disorders: injury patterns and treatment, Palmer AK, Arthroscopy, 1990
[17]
Diagnostic Wrist Arthroscopy, Michelotti BF, Chung KC, Hand Clin, 2017
[18]
Diagnostic Wrist Arthroscopy, Michelotti BF, Chung KC, Hand Clin, 2017
[19]
Diagnostic Wrist Arthroscopy, Michelotti BF, Chung KC, Hand Clin, 2017
[20]
Diagnostic Wrist Arthroscopy, Michelotti BF, Chung KC, Hand Clin, 2017
[21]
Wrist arthroscopy: indications, portal anatomy and therapeutic advances, Orthopaedics and Trauma, Selvin O et al., Wrist arthroscopy: indications, portal anatomy and therapeutic advances, Orthopaedics and Trauma, ,
[22]
Handgelenksarthroskopie, Schaefer Manuel, Siebert Hartmut, Georg Thieme Verlag KG, 2001
[23]
Handgelenksarthroskopie, Schaefer Manuel, Siebert Hartmut, Georg Thieme Verlag KG, 2001
[24]
Handgelenksarthroskopie, Schaefer Manuel, Siebert Hartmut, Georg Thieme Verlag KG, 2001
[25]
Minimally invasive management of scaphoid nonunions, Slade JF 3rd, Dodds SD, Clin Orthop Relat Res, 2006
[26]
Minimally invasive management of scaphoid nonunions, Slade JF 3rd, Dodds SD, Clin Orthop Relat Res, 2006
[27]
Treatment of the scaphoid humpback deformity - is correction of the dorsal intercalated segment instability deformity critical?, Mathoulin CL, Arianni M, J Hand Surg Eur Vol, 2018