["7133c666e0c66761eba8ba6aa924d6b5731459ff","42b4be201f4766cc48df2bfcdd9dcd3e1c4d6a61"]
Rhinoplasty
primary rhinoplasty
aesthetic rhinoplasty
4294
4294
Chapter reads
0
0
Chapter likes
7/10
Evidence score
06
6
Images included
01
1
Videos included
01
Introduction
Introduction
Rhinoplasty is one of the most popular aesthetic procedures in plastic surgery3. At the same time its level of complexity is high due to an extensive ethical and inter-individual variability of nasal shape, aesthetic desires and concomitant functional impairment. Further, the flat learning curve is challenging for surgeons, as their final results cannot be evaluated in the immediate postoperative period due to persistent soft tissue edema commonly lasting for months.
This chapter represents a practical and concise guide for the aspiring rhinoplasty surgeon covering relevant knowledge on surgical anatomy, patient counselling and aesthetic nasal analysis, as well as a step-by-step instruction for primary open rhinoplasty. Supportive tips and pitfalls by experts in the demanding field of rhinoplasty were implemented to assist in the achievement of successful outcomes.
This chapter represents a practical and concise guide for the aspiring rhinoplasty surgeon covering relevant knowledge on surgical anatomy, patient counselling and aesthetic nasal analysis, as well as a step-by-step instruction for primary open rhinoplasty. Supportive tips and pitfalls by experts in the demanding field of rhinoplasty were implemented to assist in the achievement of successful outcomes.
02
Anatomical Foundation
Anatomical Foundation46
Skin envelope: Due to the presence of sebacious glands, skin is thickest in the lower third of the nose. The skin envelope of the upper/ middle thirds is thinner and more mobile.
Musculature: Nasal muscles can be categorized according to their function.
Elevation: M. procerus produces transverse wrinkles at the glabella.
Depression: M. depressor septi nasi alters nasal tip projection during smiling.
Compression: M. nasalis creates typical “bunny lines”.
Dilatation: M. levator labii superioris alaeque nasi maintains patency of the external nasal valve.
Innervation:
Motor function: N. facialis (CN VII)
Sensation: Ophthalmic and maxillary branches of N. trigeminus (CN V)
Olfaction: N. olfactorius (CN I)
Primary blood supply:
A. ophthalmica: Its terminal branch supplies the nasal dorsum (A. dorsalis nasi).
A. facialis: Supplies the nasal tip via A. angularis and A. labii superioris branches. When performing open rhinoplasty with a transcolumellar incision, nasal tip blood supply depends exclusively on A. angularis as columellar branches from A. labii superioris are sacrificed.
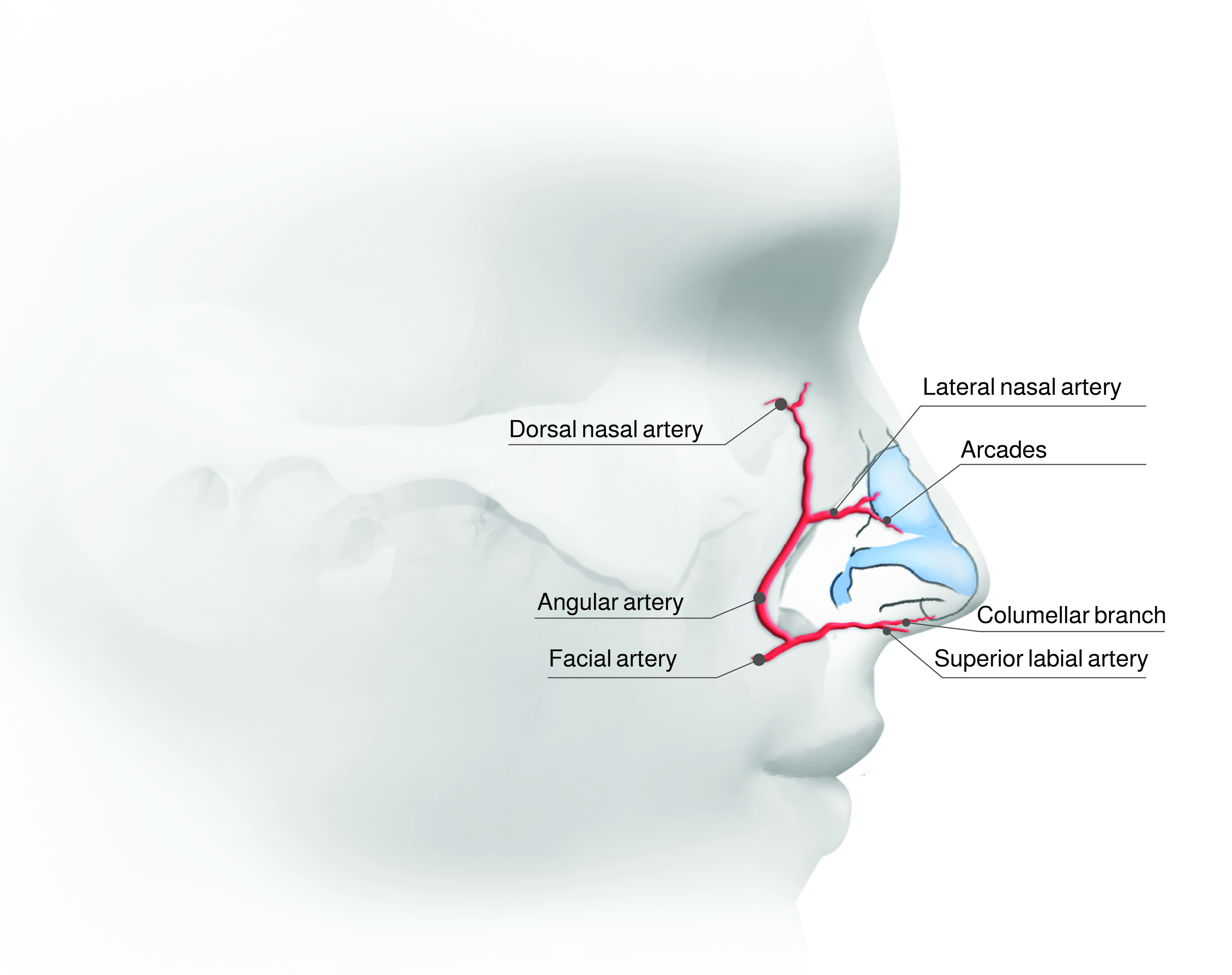
Nasal blood supply
Nasal vaults: The nasal framework is formed by an upper osseous nasal vault and two lower cartilaginous vaults.
Osseous vault (upper third): Consists of paired nasal bones and ascending processes of the maxilla.
Upper lateral cartilage (ULC, middle third): Underlies nasal bone as well as lower lateral cartilage.
Keystone area: Transition zone between ULC and nasal bone.
Scroll region: Transition zone between LLC and ULC.
LLC (lower third): Medial, intermediate (or middle) and lateral crura are LLC subunits.
Septum: Consists of a membranous, quadrangular cartilaginous and an osseous portion (anterior nasal spine of maxilla, perpendicular plate of ethmoid, vomer).
Nasal tip: Medial and lateral crura of LLC supported by accessory ligamentous structures (e.g., domal suspensory ligament, fibrous attachments between LLC and ULC, connections of LLC and piriform aperture) define the nasal tip7.
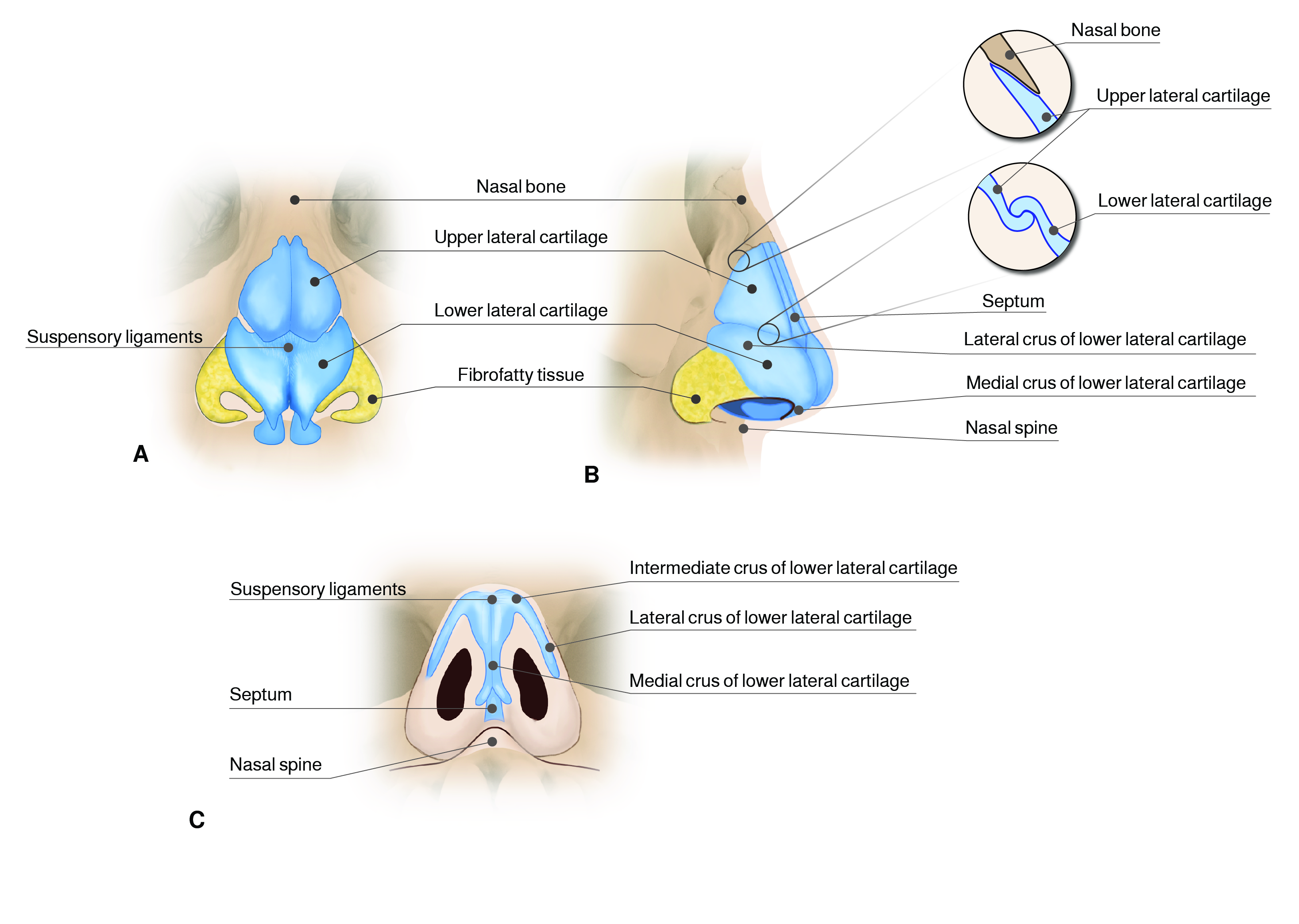
Cartilaginous skeleton
Tripod concept8: Medial and lateral crura of LLC represent the legs of a tripod. The Tripod concept helps to understand how elongation or shortening of medial and/ or lateral crura affect tip rotation and projection.
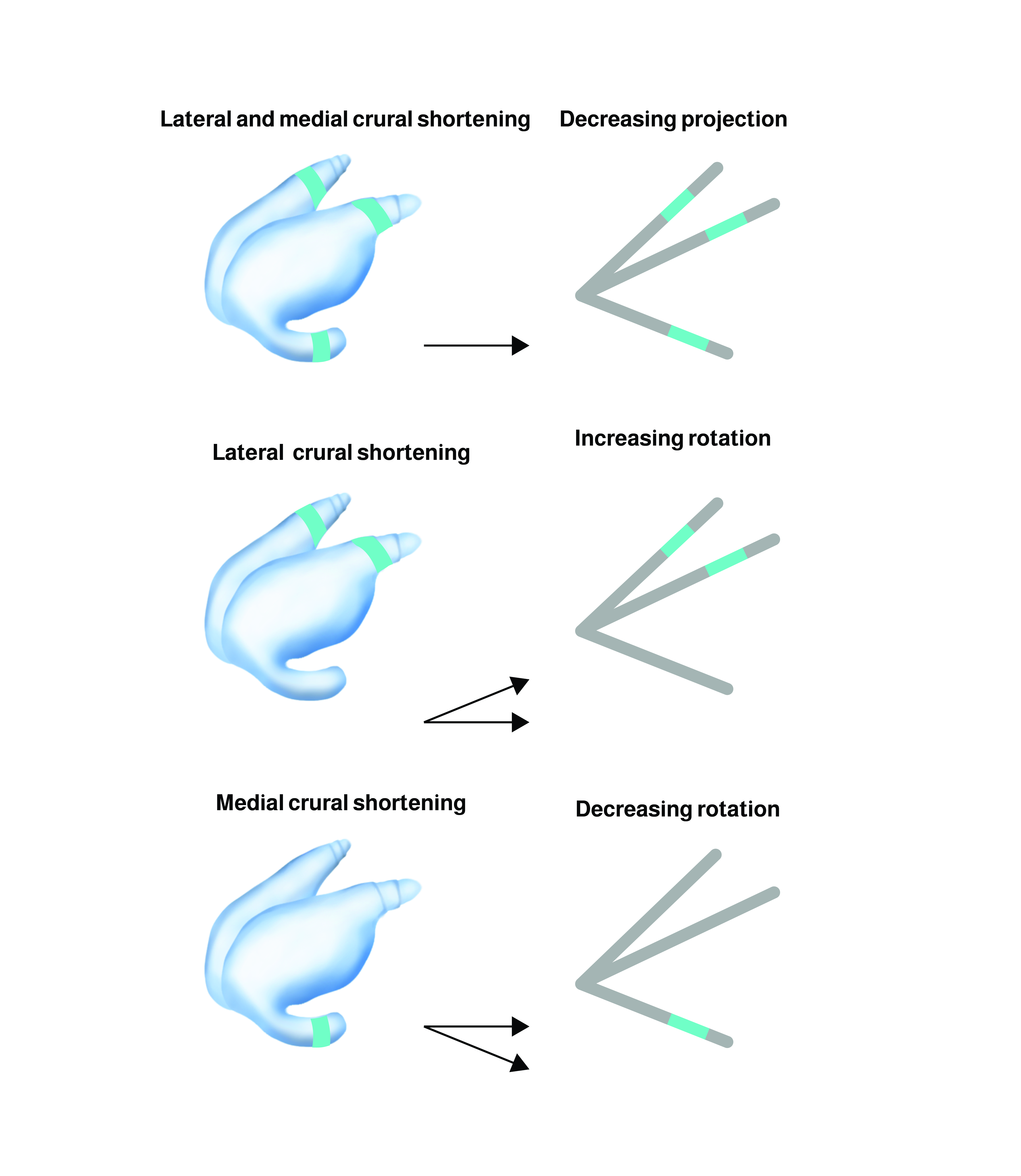
Tripod Concept
Internal nasal valve: Region of greatest nasal airflow resistance9. Formed by junction of dorsal septum, caudal ULC and inferior turbinate. An ideal angle measures between 10-15°. More acute angles lead to airway obstruction.
External nasal valve: Formed by caudal septum, caudal LLC and columellar/ alar soft tissues. Patency is maintained by M. levator labii superioris alaeque nasi.
Paralysis of M. levator labii superioris alaeque nasi can lead to external nasal valve collapse and nasal airway obstruction in facial palsy patients11.
03
Aesthetic and Functional Nasal Analysis
Aesthetic and Functional Nasal Analysis
Meticulous preoperative aesthetic and functional nasal assessment is the first determining step to achieve satisfying rhinoplasty results. Nasal analysis provides the foundation for the development of your surgical treatment strategy. Further, it offers the unique chance to understand the patient’s concerns and objective them. Key to success is an informed patient who has realistic expectations. The patient and surgeon both have to work on the same goals to achieve a favorable outcome. Standardized photography is an essential element of preoperative documentation3.
Aesthetic nasal analysis31214:
Frontal view:
Width: Alar base width should match intercanthal distance. Upper nasal third measures about 80% of alar base width.
Deviation: Determine if nose is straight or crooked.
Dorsal aesthetic lines: Bilateral dorsal aesthetic lines should appear slightly curved, extending from the radix to the tip-defining points.
Tip definition: Assess if the tip appears bulbous or narrow and detect asymmetries. The two tip-defining points should provide symmetrical light reflexes.
Lateral view:
Nasofrontal angle: Ideally estimates about 140°.
Dorsum: Males should have a straight dorsum. A slightly concave dorsum containing a supratip break is aesthetically pleasing in females. Evaluate for cartilaginous, osseous or composite cartilaginous/ osseous humps.
Tension nose: Identify a tension nose. It is characterized by an excessively high septum with inferior displacement and narrowing of the nasal tip15.
Tip projection/ rotation: Assess nasal tip projection and rotation.
Tip projection: Posterior-to-anterior distance that the nasal tip extends from the facial plane.
Tip rotation: Is assessed by determining the nasolabial angle ideally measuring 90-95° in males and 95-110° in females.
Base view: Alar rims should create an equilateral triangle. Evaluate for asymmetries.
Nasal airway obstruction: Seasonal airway obstruction may be caused by allergic rhinitis. A thorough history may unveil nasal airway obstruction that benefits from surgical repair such as the following:
Internal nasal valve collapse: Spreader grafts and autospreader flaps are used to increase internal nasal valve angle16.
Cottle’s maneuvre: The Cottle's maneuver is a test in which the cheek on the side to be evaluated is gently pulled laterally to open the internal nasal valve17. When nasal airway obstruction is relieved by the Cottle’s maneuver, a patient is expected to benefit from spreader grafts or autospreader flaps.
External nasal valve collapse: Alar rim grafts are used to strengthen the external nasal valve18.
Inferior turbinate hypertrophy: Inferior turbinate reduction by outfracturing (lateral displacement) or submucosal resection can improve airway obstruction caused by inferior turbinate hypertrophy.
Septal deviation: Use a speculum to visualize deviations, spurs or perforations of the cartilaginous septum.

Examination sheet
04
Surgical Technique
Surgical Technique
Although closed (endonasal) rhinoplasty has indisputable advantages (e.g., absence of a visible scar, less surgical trauma, minimal edema, faster operation as well as patient recovery) direct visualization of the nasal anatomy and its alterations facilitates a comprehensive understanding and allows safe and most predictable results20. Thus, this chapter has its main focus on primary open rhinoplasty.
1. Closed (Endonasal) Rhinoplasty
Closed rhinoplasty is useful for isolated septal correction and/or mild refinements of the LLC and nasal tip2122. The exact surgical approach is directed to the specific deformity to be addressed:
Cartilage incision:
Intercartilaginous: Located between the ULC and LLC.
Transcartilaginous: Cartilage-splitting of the LLC.
Infracartilaginous: Caudal to the LLC, close to the alar rim.
Septal incision:
Transfixion: Complete transection at junction of caudal septum and medial crura of LLC/ columella.
Hemitransfixion: Unilateral incision at junction of caudal septum and medial crura of LLC/ columella.
Modifications (e.g., partial transfixion, high septal transfixion)
Killian incision: Incision is placed approximately 0.5 cm posterior to edge of the septum preserving septal stability.
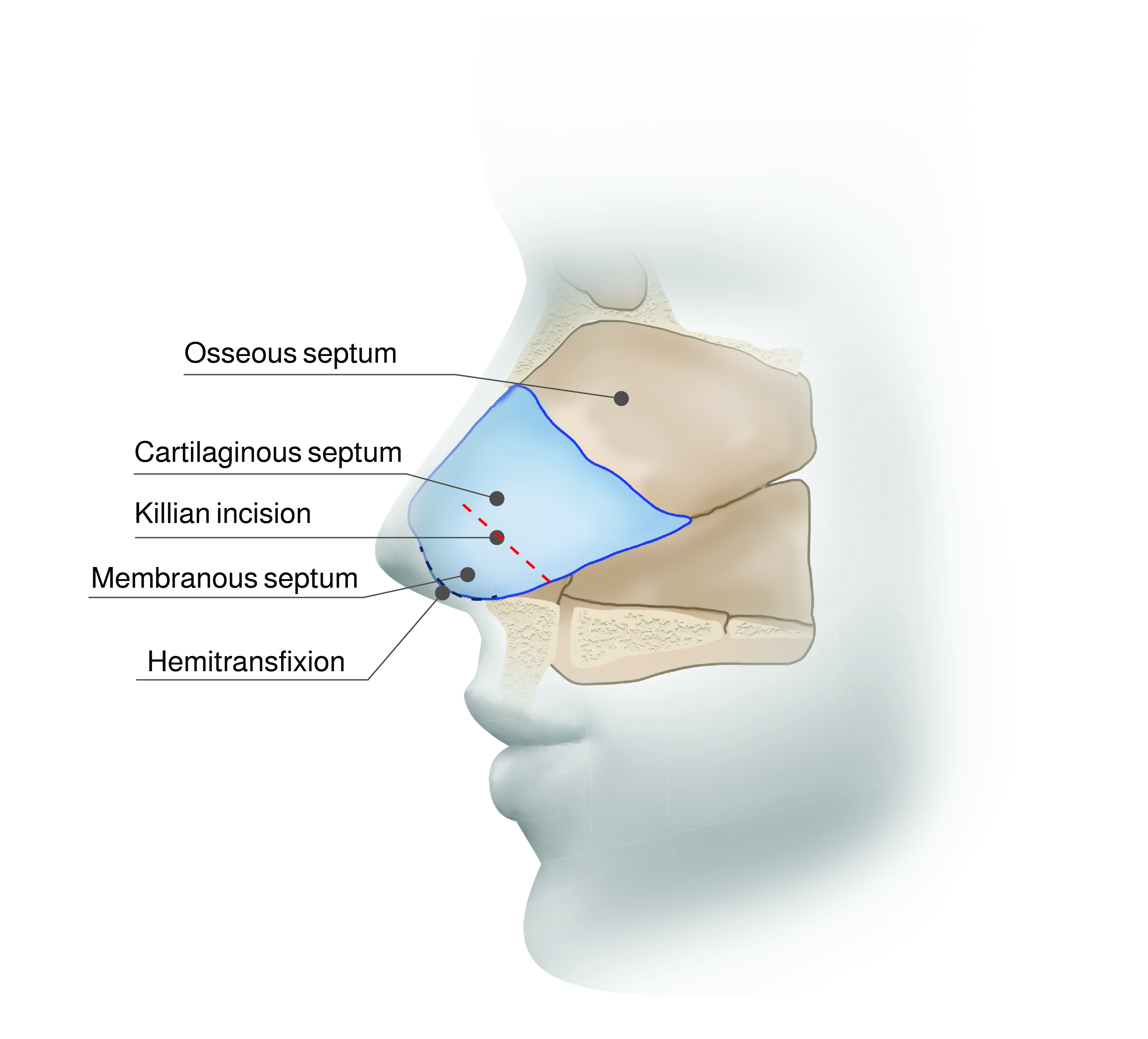
Closed Rhinoplasty Approaches
2. Primary Open Rhinoplasty
The following provides a practical and comprehensible step-by-step approach to primary open rhinoplasty and covers strategies to confidently deal with the most common aesthetic nasal deformities.
Preparation of the surgical field: Cautiously remove nasal fibrissae and inject diluted epinephrine solution (1: 200 000 – 100 000) to minimize bleeding.
Skin incision:
Transcolumellar inverted-V incision24: Use a 15-scalpel blade and coagulate the columellar branch of A. labialis superior carefully.
Vestibular/ paracolumellar incision and infracartilaginous incisions: Use sharp scissors rather than a scalpel. Identify the medial crura. Avoid to incise them and continue your vestibular/ paracolumellar preparation. Dissect along the inferior border of the lateral crus and avoid disrupting the soft triangle.
Skin flap elevation: Dissection has to be slow and meticulous. Elevate the flap as close to the cartilage as possible and expose the nasal tip. Domal ligamentous structures are encountered. Dissection is continued to the nasofrontal angle. The ideal dissection planes with minimum bleeding are supraperichondrial and then subperiosteal. Use of an Aufricht retractor allows optimal exposure.
Septoplasty: Injection of diluted epinephrine solution (1: 200 000 – 100 000) facilitates exposition of the septum tremendously. Separation of domal ligaments exposes the septum. Incise the mucoperichondrium parallel to the columella on each side and elevate mucoperichondrial flaps using a Freer or Cottle elevator. Be careful to avoid septal perforation. In case of septal deviations preparation of mucoperichondrial flaps should start on the side of septal convexity. This strategy lowers the risk of iatrogenic septal perforations. To fully mobilize the septum identify and release the chondro-osseous junctions to the perpendicular plate of the ethmoid and the vomer. Try to maintain the attachment of the septum to the anterior nasal spine of the maxilla. Reduce and straighten the septum for correction of mild septal deviation. In case of a decentralized attachment of the septum at the anterior nasal spine, it can be translocated to the midline and re-anchored according to the swinging-door technique25. Severe septum deviation can also be corrected by extracorporeal septoplasty26. Either the entire septum or an L-framed septal strut can be relocated27.
Use cold saline-soaked gauze to cover the surgical field while processing the septum extracorporeally or preparing any cartilage grafts to reduce nasal swelling.
Hump reduction: Cartilaginous humps can be tangentially removed with a scalpel blade under direct vision. Address osseous/ composite osseo-cartilaginous humps conventionally by an osteotome and hammer or by the use of an ultrasonic piezoelectric device28. Osseo-cartilaginous humps were traditionally removed en-bloc (composite reduction). To avoid destabilization of the keystone area resulting in a collapse of the ULC and a conspicuous inverted-V deformity, dorsal strip component reduction (dorsal split hump technique) with sharp separation of ULC from the dorsal septum has been implemented29.
Osteotomy: An open roof is the natural and inevitable consequence of a hump reduction. Closure can be achieved by medial and lateral osteotomies. Osteotomies are required to mobilize the bony vault thereby closing an open roof or changing the width of the nasal base. Lateral osteotomy can be performed either percutaneous or open, while medial osteotomy should be done under direct vision. Lateral osteotomy is carried out along a line connecting the supero-lateral border of the piriform aperture and the intercanthal line following specific patterns (e.g., high-low-high)30. It is safer to perform internal medial osteotomies with large osteotomes (8-10 mm) to reduce the risk for skull base penetration. Bilateral medial oblique osteotomies are designed to form a V-pattern. Most importantly, osteotomies should not extend more cranial than the intercanthal line to avoid the thick bone of the radix and prevent a rocker deformity31.
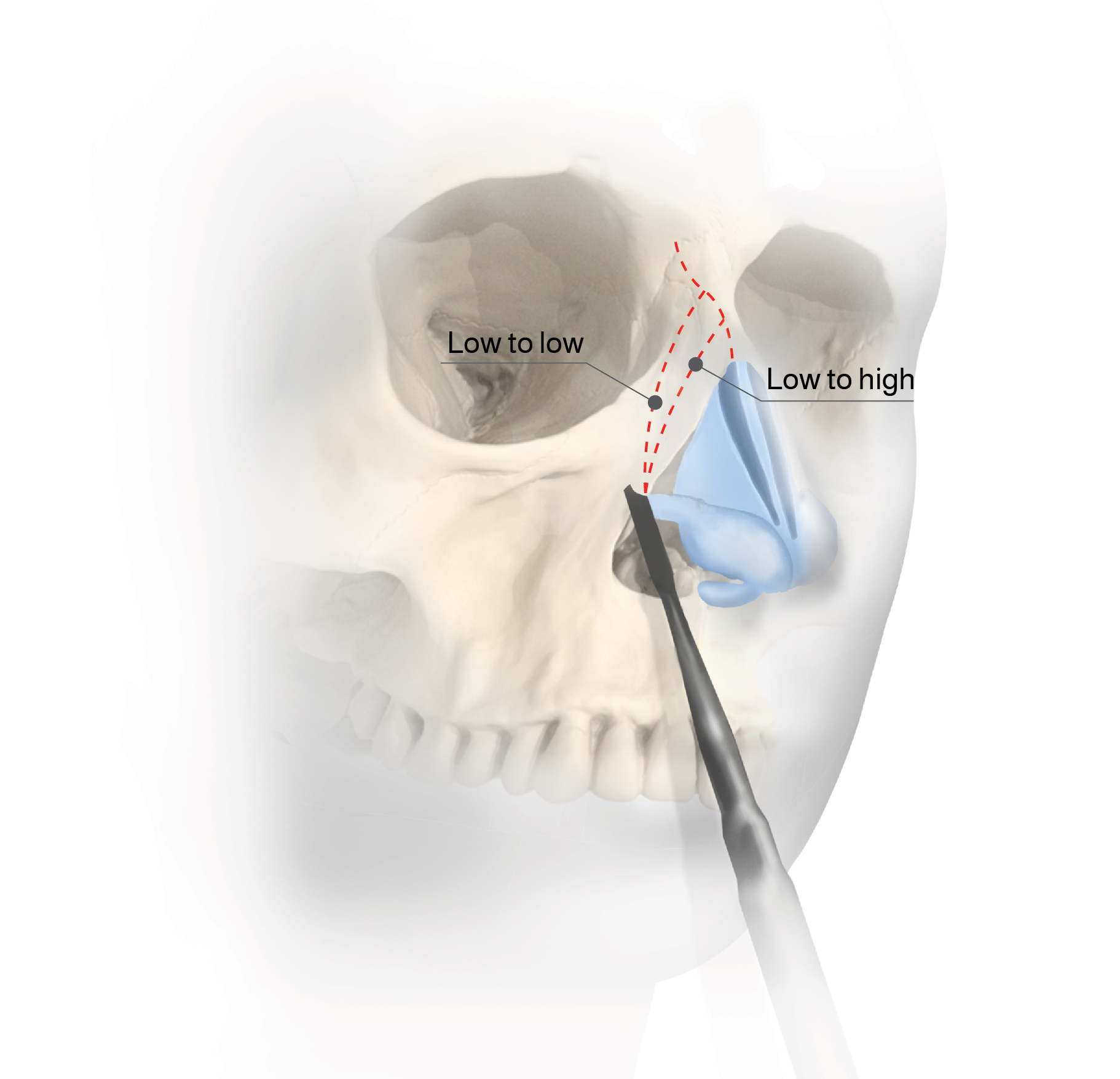
Lateral Osteotomy Variants
Spreader grafts: Spreader grafts or spreader flaps are used for reconstruction of the internal nasal valve. Spreader grafts are rectangular bars (usually sizing about 20-30 x 3-5 x 1-2 mm) fashioned from septal (or conchal) cartilage and placed bilaterally between the dorsal septum and ULC16. Alternatively, autospreader flaps can be formed by rolling the dorsal edge of the ULC on itself and securing it to the dorsal edge of the reduced septum32.
Tip modification: The Tripod concept helps to understand how elongation or shortening of medial and/ or lateral crura affect tip rotation and projection. Medial and lateral crura of LLC represent the legs of a tripod. Isolated shortening (elongation/ strengthening) of the medial crura decreases (increases) tip rotation only. On the contrary, isolated shortening (elongation/ strengthening) of the lateral crura increases (decreases) tip rotation. Shortening (elongation/ strengthening) of both lateral and medial crura maintains rotation while decreasing (increasing) tip projection8. Based on this concept various suturing techniques and cartilage grafts can be used for nasal tip modeling.
Changing tip projection: Columella strut grafts (placement of a rectangular septal cartilage strut between the medial crura), interdomal sutures or tip onlay grafts are usually used to increase tip projection1833.
Changing tip rotation: Trimming of medial and lateral crura is a common technique used to change tip rotation. Medial crura shortening decreases tip rotation while lateral crura trimming increases tip rotation. Further rotation is obtained by caudal excision of the septum8.
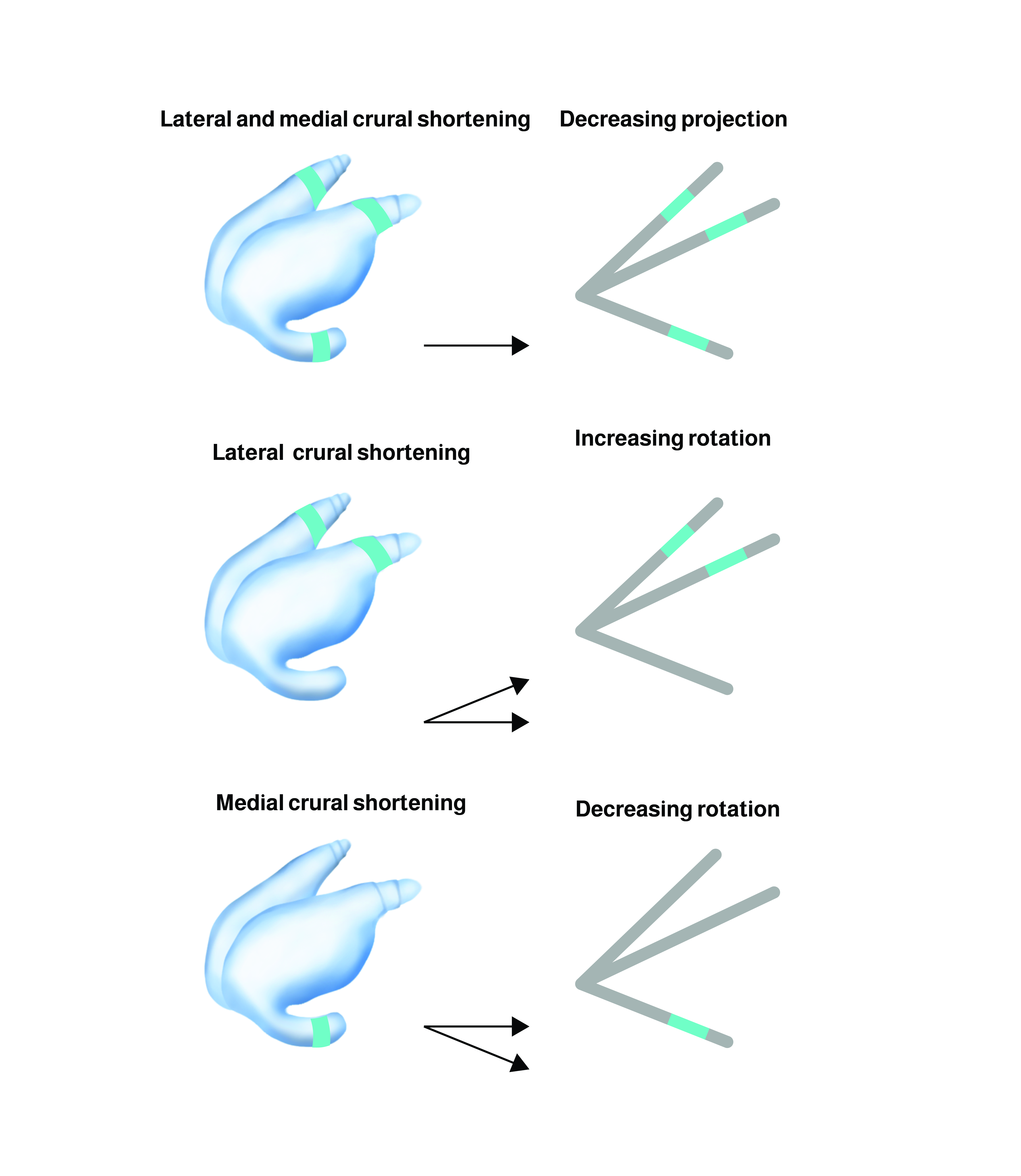
Tripod Concept
Other selected cartilage grafts:
Alar rim grafts18: Alar rim grafts are placed in a pocket along the alar rim. The aim of alar rim grafts is to enhance the contour of the nasal ala thereby supporting patency of the external nasal valve.
Diced cartilage: Small fragments of autologous cartilage (diced cartilage) wrapped by a thin layer temporalis fascia to form a roll can be used for augmentation of the nasal dorsum. Temporal fascia is a useful "lifeboat" to cover the nasal dorsum and optimize overall aesthetic results.
Wound closure: Soft, rapidly absorbable sutures (e.g., Vicryl rapide 5-0) can be used for vestibular and transcolumellar wound closure to avoid painful suture removal in this sensitive region.
Dressing/ splints: The external nasal splint should be molded precisely to secure the final rhinoplasty result36. If any septal manipulation is performed, internal silicone splints are commonly used in addition.
Give careful instructions on postoperative behavior. Swallowing of blood induces nausea and emesis. Thus, instruct your patients to spit out bloody nasal/ pharyngeal secretions. Patients should avoid pressure at the nasal dorsum by wearing glasses in the first postoperative weeks. To reduce postoperative bleeding and edema sports should be abandoned.
05
Typical Complications and How to Avoid or Handle Them
Typical Complications and How to Avoid or Handle Them
Aesthetic complications: Most rhinoplasty complications are associated with poor aesthetics or contour irregularities. Most importantly the surgeon must ensure realistic patients’ expectations prior to performing rhinoplasty.
Specific aesthetic rhinoplasty complications include the following deformities12:
Specific aesthetic rhinoplasty complications include the following deformities12:
Rocker deformity: High fracture at the fronto-nasal junction caused by medial osteotomy carried too far superiorly.
Inverted-V deformity: Middle vault collapse resulting from excessive ULC resection or inadequate reconstruction of keystone area.
Open-roof deformity: Failure of dorsum reconstruction/ closure following hump reduction.
Polly peak deformity: Excessive projection at the supratip region.
Septal hematoma: Use internal nasal splints to avoid dead space and hemorrhage between septum and mucoperichondrial flaps when performing extracorporeal septoplasty to avoid septal hematoma/ necrosis2.
Septal perforation: Handle delicate nasal cartilaginous structures carefully during the course of the surgery to avoid iatrogenic injury2.
Soft tissue edema: Avoidance of hypertensive blood pressure, extensive physical activities, head elevatation and use cool compresses in the early postoperative period to reduce swelling. Persistent edema can mask the final result for months following rhinoplasty3.
Nasal airway obstruction: Most commonly functional impairment is temporary and results from soft tissue edema34.
Skin necrosis: Meticulous dissection in the supraperichondrial and subperiosteal plane is key to maintain a stable skin envelope34.
06
Helpful Hints and Tricks
Helpful Hints and Tricks
Standardized preoperative photographs (frontal, lateral and base views) are a key element of surgical planning.
It is worthwhile to invest time in setting realistic patients’ expectations and preoperative counseling.
To avoid injury to the medial and lateral crura, some surgeons may find it easier to use sharp scissors rather than a scalpel for paracolumellar/ infracartilaginous dissection in open rhinoplasty.
Osteotomies induce maximum edema and bleeding that impairs intraoperative monitoring of your results. Thus, try to postpone osteotomies to the end of the procedure.
Injection of diluted epinephrine solution (1: 200 000 – 100 000) facilitates exposition of the septum tremendously.
Temporal fascia is a useful "lifeboat" to cover the nasal dorsum and optimize overall aesthetic results.
In case of septal deviations preparation of mucoperichondrial flaps should start on the side of septal convexity. This strategy lowers the risk of iatrogenic septal perforations.
07
Key Points
Key Points
A thorough understanding of nasal anatomy and aesthetic principles is fundamental.
Successful rhinoplasty begins with a detailed preoperative analysis of nasal shape and function.
Nasal obstruction is often caused by impairment of external or internal nasal valve patency, septal deviation and inferior turbinate hypertrophy.
Aesthetic concerns that rhinoplasty patients seek advice for commonly regard the correction of cartilaginous/ composite cartilaginous-osseous humps, nasal deviation, broad nasal root/ middle vault, tip refinement and alteration of tip projection/ rotation.
Rhinoplasty can be performed through an open or closed approach.
An open-roof deformity is a surgical complication caused by failure of nasal dorsum reconstruction following hump reduction.
Revision rhinoplasty is even more challenging than primary rhinoplasty.
08
Suggested Readings
Suggested Readings
Alamuti N. Das „12-step-rhinoplasty“ Konzept. Plastische Chirurgie, Dr. R. Kaden Verlag GmbH und Co. KG 2017, edition 1, 2017: 2-8. Article in German
Rohrich RJ, Afrooz PN. Primary Open Rhinoplasty. Plast Reconstr Surg 2019: 144: 102e-17e. CME article and video section
Daniel R, Pálházi P. Rhinoplasty: An Anatomical and Clinical Atlas. Springer Verlag: 1st edition 2018. Anatomical dissections
Images
Closed Rhinoplasty Approaches
Lateral Osteotomy Variants
Tripod Concept
Examination sheet
Nasal blood supply
Cartilaginous skeleton
Videos
Primary open rhinoplasty
References
[1]
Rhinoplasty, Rohrich RJ, Ahmad J, Plast Reconstr Surg, 2011
[2]
Anatomic considerations in aesthetic rhinoplasty, Lam SM, Williams EF 3rd, Facial Plast Surg, 2002
[3]
Rhinoplasty: nasal anatomy, Daniel RK, Letourneau A, Ann Plast Surg, 1988
[4]
An anatomic study of nasal tip supporting structures, Han SK, Lee DG, Kim JB, Kim WK, Ann Plast Surg, 2004
[5]
Nasal tip overprojection: algorithm of surgical deprojection techniques and introduction of medial crural overlay, Soliemanzadeh P, Kridel RW, Arch Facial Plast Surg, 2005
[6]
Nasal tip overprojection: algorithm of surgical deprojection techniques and introduction of medial crural overlay, Soliemanzadeh P, Kridel RW, Arch Facial Plast Surg, 2005
[7]
The airflow resistance profile of healthy nasal cavities, Hirschberg A, Roithmann R, Parikh S, Miljeteig H, Cole P, Rhinology, 1995
[8]
Prospective evaluation of quality-of-life improvement after correction of the alar base in the flaccidly paralyzed face, Lindsay RW, Bhama P, Hohman M, Hadlock TA, JAMA Facial Plast Surg, 2015
[9]
Rhinoplasty, Rohrich RJ, Ahmad J, Plast Reconstr Surg, 2011
[10]
Rhinoplasty, Rohrich RJ, Ahmad J, Plast Reconstr Surg, 2011
[11]
Rhinoplasty: a practical guide for surgical planning, Byrd HS, Hobar PC, Plast Reconstr Surg, 1993
[12]
Nasal and facial analysis, Woodard CR, Park SS, Clin Plast Surg, 2010
[13]
The tension nose: open structure rhinoplasty approach, Johnson CM Jr, Godin MS, Plast Reconstr Surg, 1995
[14]
The value of spreader grafts in rhinoplasty: a critical review, Teymoortash A, Fasunla JA, Sazgar AA, Eur Arch Otorhinolaryngol, 2012
[15]
Effects of the Cottle's maneuver on the nasal valve as assessed by acoustic rhinometry, Tikanto J, Pirilä T, Am J Rhinol, 2007
[16]
Structural grafts and suture techniques in functional and aesthetic rhinoplasty, Gassner HG, GMS Curr Top Otorhinolaryngol Head Neck Surg, 2010
[17]
The merits of the open approach in rhinoplasty, Gunter JP, Plast Reconstr Surg, 1997
[18]
Open and closed rhinoplasty (minus the "versus"): analyzing processes, Tebbetts JB, Aesthet Surg J, 2006
[19]
Transfixion incision as an initial technique in nasal tip deprojection, Solomon P, Rival R, Mabini A, Boyd J, Can J Plast Surg, 2008
[20]
Comparative Columellar Scar Analysis Between W Incisions and Inverted-V Incision in Open Technique Nasal Surgery, Ihvan O, Seneldir L, Naiboglu B, Verim A, Cetiner S, Indian J Otolaryngol Head Neck Surg, 2018
[21]
Principles of nasal septum reconstruction, Wright WK, Trans Am Acad Ophthalmol Otolaryngol, 1969
[22]
The correction of the internally and externally deviated nose, KING ED, ASHLEY FL, Plast Reconstr Surg (1946), 1952
[23]
Surgical correction of the severely deviated nose by extramucosal excision of the osseocartilaginous septum and replacement as a free graft, Rees TD, Plast Reconstr Surg, 1986
[24]
Comparison of piezoelectric and conventional osteotomy in rhinoplasty : A systematic review, Wähmann M, Riedel F, Kovacevic M, Hopf A, Albers AE, HNO, 2019
[25]
Split hump technique for reduction of the overprojected nasal dorsum: a statistical analysis on subjective body image in relation to nasal appearance and nasal patency in 97 patients undergoing aesthetic rhinoplasty, Lohuis PJ, Faraj-Hakim S, Knobbe A, Duivesteijn W, Bran GM, Arch Facial Plast Surg, 2012
[26]
Understanding Why Lateral Osteotomy During Rhinoplasty Can Be Performed Safely, Mowlavi A, Kim JB, Molinatti N, Saadat S, Sharifi-Amina S, Wilhelmi BJ, Eplasty, 2019
[27]
The optimal medial osteotomy: a study of nasal bone thickness and fracture patterns, Harshbarger RJ, Sullivan PK, Plast Reconstr Surg, 2001
[28]
The value of spreader grafts in rhinoplasty: a critical review, Teymoortash A, Fasunla JA, Sazgar AA, Eur Arch Otorhinolaryngol, 2012
[29]
The spreader flap in primary rhinoplasty, Gruber RP, Park E, Newman J, Berkowitz L, Oneal R, Plast Reconstr Surg, 2007
[30]
Nasal tip overprojection: algorithm of surgical deprojection techniques and introduction of medial crural overlay, Soliemanzadeh P, Kridel RW, Arch Facial Plast Surg, 2005
[31]
Structural grafts and suture techniques in functional and aesthetic rhinoplasty, Gassner HG, GMS Curr Top Otorhinolaryngol Head Neck Surg, 2010
[32]
Suture contouring of the nasal tip, Baker SR, Arch Facial Plast Surg, 2000
[33]
Nasal tip overprojection: algorithm of surgical deprojection techniques and introduction of medial crural overlay, Soliemanzadeh P, Kridel RW, Arch Facial Plast Surg, 2005
[34]
Structural grafts and suture techniques in functional and aesthetic rhinoplasty, Gassner HG, GMS Curr Top Otorhinolaryngol Head Neck Surg, 2010
[35]
Customized external nasal splint after rhinoplasty, introduction to the "tissu-modelage", Auclair E, Noel W, Ann Chir Plast Esthet, 2018
[36]
Aesthetic rhinoplasty: Avoiding unfavourable results, Bhangoo KS, Indian J Plast Surg, 2013
[37]
Complications of rhinoplasty, Surowitz JB, Most SP, Facial Plast Surg Clin North Am, 2013
[38]
Complications of rhinoplasty, Surowitz JB, Most SP, Facial Plast Surg Clin North Am, 2013
[39]
Complications of rhinoplasty, Surowitz JB, Most SP, Facial Plast Surg Clin North Am, 2013
[40]
Rhinoplasty, Rohrich RJ, Ahmad J, Plast Reconstr Surg, 2011
[41]
Rhinoplasty, Rohrich RJ, Ahmad J, Plast Reconstr Surg, 2011
[42]
Anatomic considerations in aesthetic rhinoplasty, Lam SM, Williams EF 3rd, Facial Plast Surg, 2002
[43]
Rhinoplasty, Rohrich RJ, Ahmad J, Plast Reconstr Surg, 2011
[44]
Anatomic considerations in aesthetic rhinoplasty, Lam SM, Williams EF 3rd, Facial Plast Surg, 2002