["bdb49f2b89641bd90adefc33e536a81d3e17b4fa","7e2a2f2b3b32a29179d959013e1a74ab0cb7f604","86b23c730e0ae8c60512cb51c9dba2418aad2932","42b4be201f4766cc48df2bfcdd9dcd3e1c4d6a61"]
Gluteal augmentation
buttock augmentation
body contouring
composite gluteal augmentation
gluteal danger zones
gluteal implants
postbariatric buttock lift
body feminisation
hip expansion
5245
5245
Chapter reads
0
0
Chapter likes
7/10
Evidence score
19
19
Images included
01
1
Videos included
01
Introduction
Introduction
Form and dimension of the gluteus in the population is highly variable. Small asymmetries and the variety concerning shape and volume is immense. Form and shape depend on size and shape of the muscle, fat distribution and configuration of the pelvis. Terminology in terms of surgical procedures addressing the aesthetic appearance varies reference10 from gluteoplasty, buttock- or gluteal enhancement, augmentation or lift. Buttock augmentation via autologous fat transfer from area of the body into the subcutaneous layers of the buttock is also known as Brazilian Butt lift. Recently, the term composite or hybrid gluteal surgery was brought up, describing procedures in which gluteal implants and autologous fat grafting was combined reference11. Goal of all mentioned procedures is improvement of the buttocks contour, size and or shape; however, there is no exact definition concerning quantity of added volume, gain in terms of projection or changing ratios to other landmarks. Over the last decades, the professional knowledge around gluteoplasty, its relevant anatomical structures, technical mandatory refinements and specific instruments have been investigated and developed to a high expert level, which is reflected in the number of evidenced based literature, masterclasses and congresses about this field. Gluteal augmentation has moved mainstream among today's plastic surgery procedures.
02
Anatomy
Anatomy of the buttock from a plastic surgical perspective
Due to severe malpractice related morbidity and mortality of gluteoplasty, familiarity with relevant clinical anatomy is mandatory! Besides, precise evaluation of shape, volume, specific superficial anatomical landmarks and tissue quality is key to choose the right technique, analyze limitations and receive the postoperative appearance of desire.
Topical anatomical landmarks
Projection
A buttocks projection is influenced by three factors: thickness of the gluteus maximus muscle, quantity of subcutaneous fat and degree of lumbar lordosis. The amount of subcutaneous fat is usually greater in females versus males, varies among ethical groups and is strongly influenced by weight changes, aging and genetics.
Lateral lumbar Fossae / Venusian dimples
Two distinct indentations that are superficial to the sacroiliac joints formed by a fascial cutaneous insertion to the PSIS (posterior superior iliac spines), which represent attractiveness.
Sacral Space or Sacral triangle/ Rhomb of Michaelis
The sacral space is defined as the area between the lumbar-sacral junction and the upper end of the intergluteal crease length; male skeletons present a sacral triangle, female skeletons a rhomb. The female rhomb/ diamond shapes basic points corelate to the following structures: lateral to Venusian dimples, caudal to the anal rim /third to fourth coccygeal vertebras and cranial to the third to fourth lumbar vertebras. Lengths of the sacral space ideally is 50% to 100% of the intergluteal crease length.
Goal of any gluteoplasty should be preservation, emphasizing or unmasking (in obese patients) the sacral triangle/ rhomb of Michaelis.
According to the senior author, the main goal is changing body proportions mainly in two dimensions:
I) The "waist to hip- ratio" (WTHR) in an anterior- posterior view, which is the correlation between the most narrow point of the waist (between the 12th rib and the iliac crest) versus the diameter of the hips (at the hight of the trochanter). The relation should ideally be around 0,7 , which stands for a feminine WTHR defined by a narrow waist and full hips.
II) The projection index, which corresponds to the WTHR , comparing the most narrow point of the waistline in a lateral view , versus point of maximum buttock projection ideally at the hight of the pubic tubercle.
I) The "waist to hip- ratio" (WTHR) in an anterior- posterior view, which is the correlation between the most narrow point of the waist (between the 12th rib and the iliac crest) versus the diameter of the hips (at the hight of the trochanter). The relation should ideally be around 0,7 , which stands for a feminine WTHR defined by a narrow waist and full hips.
II) The projection index, which corresponds to the WTHR , comparing the most narrow point of the waistline in a lateral view , versus point of maximum buttock projection ideally at the hight of the pubic tubercle.
Infragluteal fold
Reflects the inferior border of the buttock; this well-defined sulcus is formed by thick fascial insertions from the femur and pelvis through the intermuscular fascia to the skin reference12reference13. Length and definition strongly influence aesthetic of the buttocks: medially positioned, short and sharp infragluteal folds contribute to full tight and youthful buttocks reference14 . Aging causes an increase in buttock height and lengthens the infragluteal fold, additional weight gain causes drooping of the infragluteal fold reference12.
Care must be taken with liposuction in the lower outer quadrant of the buttocks. Make sure you do not suction into the buttock pillar, which is often misinterpreted as a so called "banana roll". Manipulation/ Liposuction of the "buttock pillar" can lead to severe unaesthetic consequences and discomfort while sitting.
Iliac crest
Palpable, sometimes visible landmarks concerning the superior border of the buttock.
Exaggerated liposuction below iliac crest level is challanging, as overtreatment can lead to a sceletonized deformity.
Lateral trochanteric depression
Is formed by the greater trochanter and insertion of thigh and buttocks muscles. The existence of lateral trochanteric depressions may be desired in males, where it contributes to an athletic look.
One of the main differences in female and male buttock shaping is the filling of the zones of trochanteric depressions as significant female feature.
Pay attention to the female waist to hip ratio (WTHR)- it plays a key role in the attractive buttock presentation!
Intergluteal crest
The ideal intergluteal crease measures ideally less than the hight of the sacral space and half of the gluteus muscle height, with more volume above the end of the crease reference18 .
Intergluteal crest variations
Deep muscular- and neurovascular anatomy
There are three gluteal compartments: the gluteus maximus compartment, the gluteus medius-minimus compartment and the tensor fascia lata compartment. The gluteus maximus muscle origins at the lateral sacrum/ coccyx and posterior superior iliac spine (PSIS), is attached to the iliac crest and inserts at the iliotibial tract and lateral rim of the greater trochanter. Delicate neurovascular structures (superior and inferior gluteal vessels and sciatic nerve) are part of the medius- minimus compartment. Cadaver dissections addressing vessel diameters of veins in different tissue layers of the buttocks determined vein sizes of 1.05 +/- 0.22mm, inside the gluteus maximus of 1.3 +/- 0.3mm and inside the submuscular space of up to 13.65 +/- 6.55mm (Inferior gluteal vein) reference07
Fatgrafting into the gluteal muscle is obsolete. Even without direct intravascular injection, fat emboli can migrate into the deep venous system and cause potential lethal macro fat-embolism and consecutive right heart failure.To ensure one does not inadvertently inject into the muscle, avoid manual syringe injections! State of the art in terms of autologous gluteal lipofilling is expansion vibration lipofilling (EVL) with rigid, blunt cannulas and continuous flow (check Technique).
The sciatic nerve originates from L3 to S4 has no gluteal branch except one to the hip joint. It emerges throught the greater sciatic foramen between piriformis and superior gemellus muscle and enters theposterior compartment of the thigh. Compromising the sciatic nerve is followed by inactive thigh muscles of the posterior thigh compartment and all muscles of the rest of the leg, as well as lateral leg and complete foot sensation. Cutaneous sensation of the Buttock: the superior clunial nerves (L1 – 3), medial - (S1 – 3) and lateral clunial nerves, which innervate the superior, medial and caudal area of every side of the gluteus; the superolateral unit is innervated by the lateral cutaneous branch of the iliohypogastric (L1) and the lateral femoral cutaneous nerves (L2, 3). After autologous gluteal augmentation, protective cutaneous sensation is likely to be impaired!
Make sure to meticulously check the skin for lacerations caused by compression garments!
03
Indication
Indication for Gluteoplasty
Gluteoplasty is suitable for
Adults in good physical health status who desire to optimize/ dramatize shape, contour, volume or tissue quality (irregular skin surface, dimples) of their buttocks
Transgender (male to female) patients, who aim to feminize their body’s silhouette by feminizing the waist to hip ratio and creating a hourglass- shape reference15reference16.
Focus on Hip Expansion to mimic a wider pelvis and cover an androgynous habitus
Massive weight loss patients, who aim to redefine their buttocks contour and get rid of excessive loose gluteal tissue reference17

Pre and Postoperaive autologous gluteal fat infiltration
04
Contraindication
Contraindication
Gluteoplasty is contraindicated for
Patients presenting with unstable body weight over the last three months
Patients suffering from severe comorbidities in terms of ASAIII status (American Society of Anesthesiologist: Physical status classification system)
Relative contraindications are patients with ASAII health status; if comorbidities are under control and und a specialist’s therapy, surgery can be discussed together with the anesthesiologist
05
Preoperative Evaluation
Preoperative Evaluation
Know the anatomy (see chapter anatomy of the buttock from a plastic surgical perspective)!
Ask and check for previous liposuctions
Patients who underwent previous liposuction sometimes present with severe fibrotic subcutaneous tissue; harvesting and quantity of aspirated material may become less and more difficult than expected
Check Lipoharvesting areas and fat – depots: suitable are abdomen, flanks (women), back, inner thighs, upper arms
Pinch-test the gluteal skin: the skin envelope and its elasticity determine the amount of fat that can be subcutaneously infiltrated
Patients presenting with very tight and tense skin need to be prepared, that augmenting their buttocks to a certain degree may require more than one infiltration-session as the skin envelope needs to be conditioned. Overfilling impaires perfusion and bears the risk of oil- cysts and skin necrosis!
Understand the gluteal aesthetic units, identify the buttock type and if present, classify the grade of ptosis reference15reference18: studying the gluteal units gives orientation which areas benefit from liposuction and which profit from additional volume
Asymmetry is common; it may be subtle; however, each buttock side needs to be evaluated separately as mixed shapes exist.
Mendieta described 10 aesthetic units to the posterior region reference18 . Additionally, he and Sood classified four different basic frame types: A-shaped (30%), V- shaped (15%), Square (40%) and round (15%).
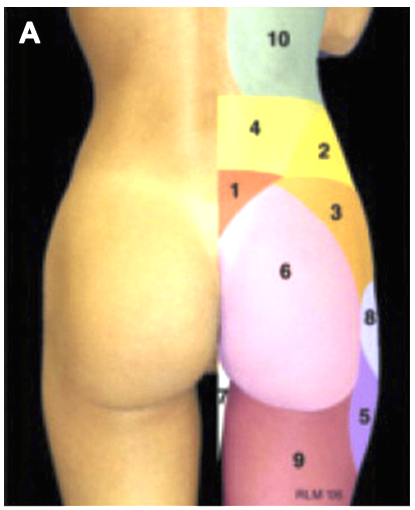
Gluteal aesthetic units
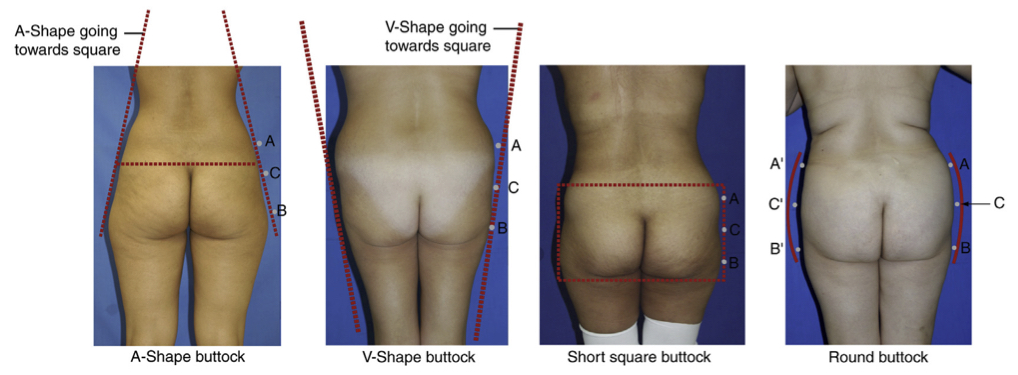
The 4 buttocks shapes
Among the other gluteal components (skin, muscle and skeleton), fat topography is the most important component of the frame and the easiest to modify!
The buttocks height can be tall, intermediate or short; square shapes, which present with a short hight (width to height ratio of the gluteus muscle from 1:1) are a typical male feature. The round shaped buttock bears the risk of unpleasant, excess fat in the lower-inner (transition between the intergluteal and intragluteal folds) gluteal fold area. V- shape buttocks tend to have a tall pelvis, thin legs, and a tendency toward central obesity.
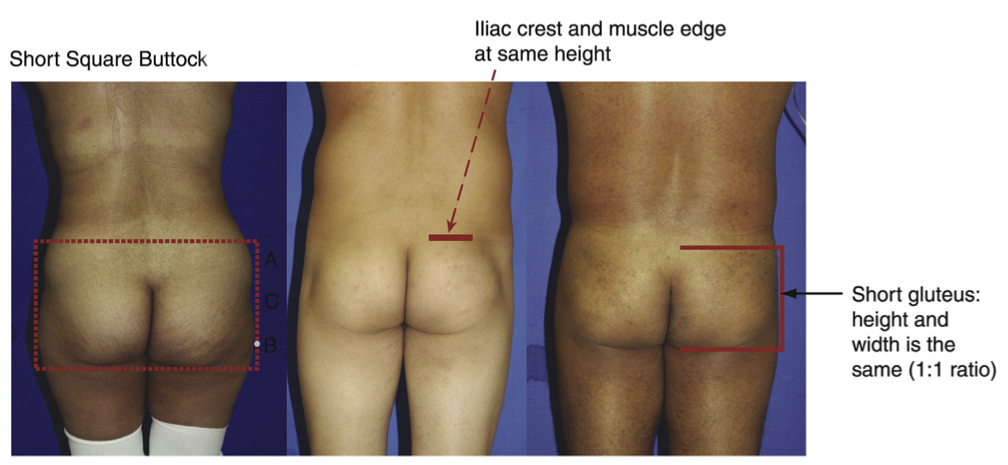
The square buttock demonstrating the role of the width to hight- ratio
The inferior gluteal base width can also be narrow (0% beyond the central vertical line), normal (10 – 30% beyond the central, mid- buttck line), or wide (40 – 50% beyond the central line). Characteristic of a young aesthetic buttock is the short clear defined ending at the mid-buttock line and a downward slope .
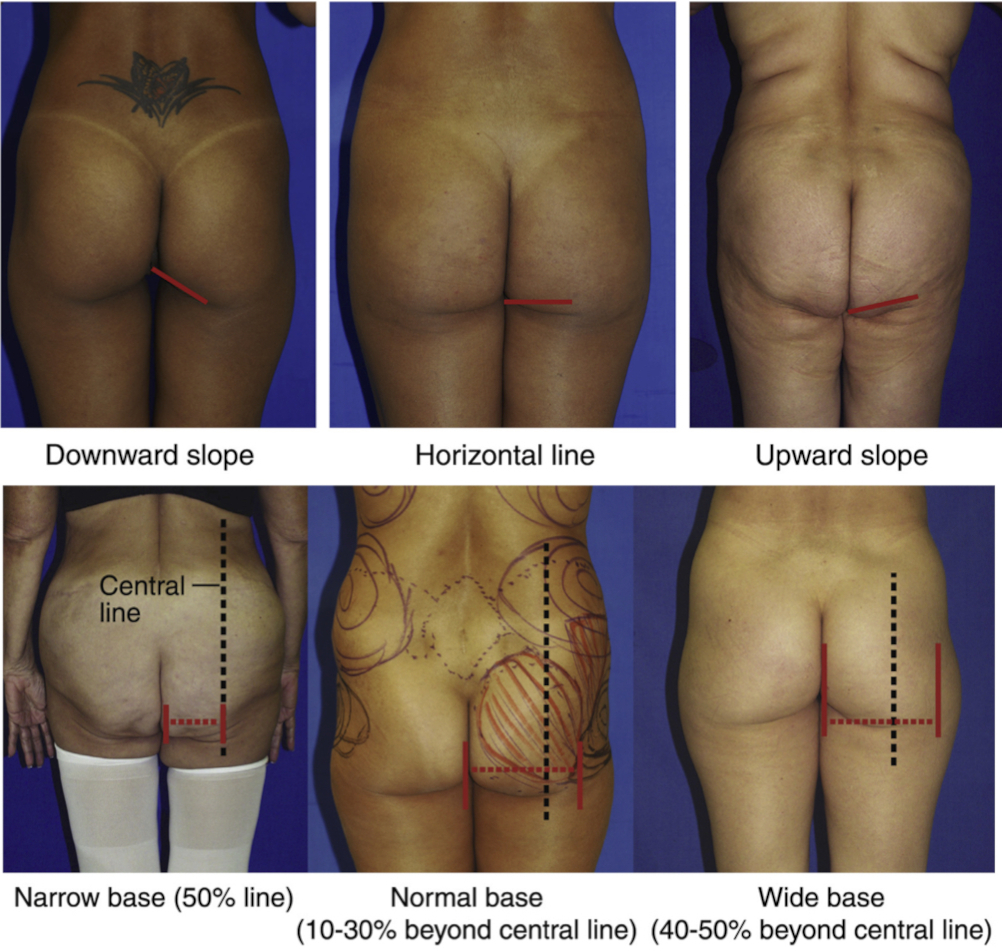
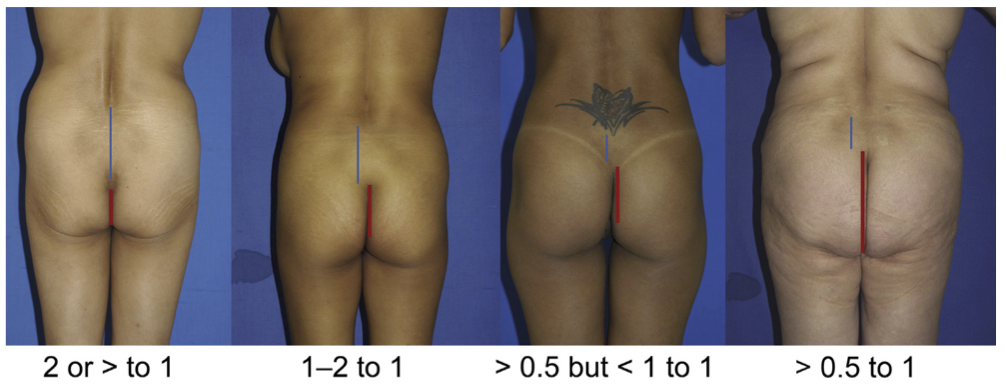
Inferior gluteal base width and slope
Concerning volume- analysis of tissue above the greater gluteus muscle it helps to devide the buttock into four quadrants (vertical and horizontal midbuttock line): in the perfect buttock, volume distribution is equal in all four quadrants with the apex of projection where both lines cross each other .
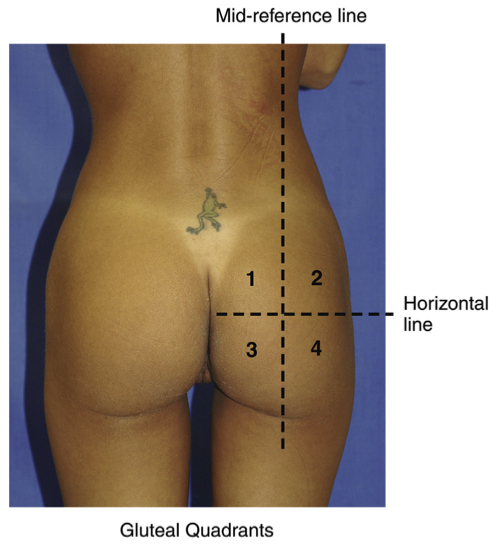
Gluteus maximus muscle volume distribution
Finally, the lateral buttock presents 3 zones: upper, central, and lower zone. This division helps determine where most of the buttock bulk or volume is and/or should be located.
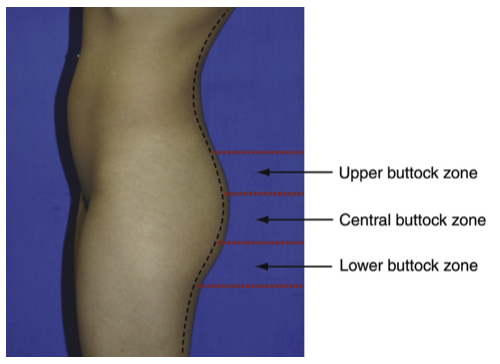
Lateral buttock zones
Mostly in weight loss or patients of advanced age, gluteal ptosis may play an important role in choosing the most suitable buttock reshaping technique: Ptosis exists, when skin droops over the infragluteal fold and the fold is appreciated at the lateral view between grade I and III according to the skinfolds angle .
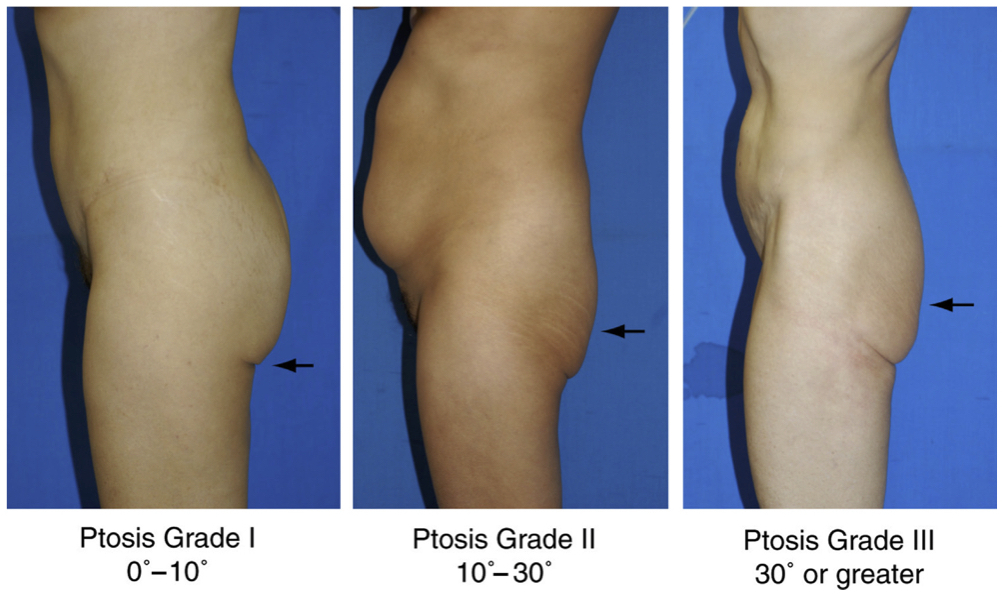
Gluteal Ptosis grade
06
Informed consent
Informed consent
Make sure that patients avoid medications and nutrition supplements that influence rheology (keep the risk for bleeding low). A hemoglobin level of at least 12 g/dl should be checked beforehand. Patients getting implants need to be informed about the specific risk of seroma, implant displacement, temporary sciatic nerve affection, capsular dehiscence, infection till implant exposure, asymmetry and anaplastic large cell lymphoma reference19. In transgender patients, pause hormone- therapy two weeks before and two weeks after surgery reference20.Work under general anesthesia or intravenous sedation! For patients getting implants: we highly recommend additional epidural anesthesia.
Emphasize that gluteoplasty requires extra high postoperative hygienic and positioning requirements and a consequent compression- garment regimen to guarantee a low complication level and assure a long-lasting result.
07
Equipment
Equipment
Autologous fat grafting
Predicting fat graft volume resorption remains challenging and varies from 20 – 90%; it is influenced by a large number of variables including graft size, procedure techniques, graft microenvironment etc. reference21. Mechanisms concerning adipose tissue graft survival remain subject of scientific studies, however well supported theories exist.
Tumescence fluid
Earlier investigations have shown that lidocaine has potential cytotoxic effects on adipocyte stem cells in vitro, which is crucial in terms of transplant survival reference22 . Other investigations found no evidence for banning lidocaine from its use in lipotranser reference23 as it had no adverse effect on the relative distribution, cell number, or viability of adipocyte stem cells, preadipocytes, mature adipocytes, or leukocytes in the stromal- vascular fraction. However, the dosage of lidocaine depends on patient’s bodyweight as well as well as the additional use of epinephrine and often is maxed out in large volume lipoaspiration.
Avoid the risk of potential cardiovascular side effects of lidocaine by disclaiming it from the tumescence fluid in high volume lipo- aspiration procedures and work under general anesthesia with or without additional spinal anesthesia.
Cannulas
Several studies have been made studying the influence of the lipoaspiration- cannulas diameter on fat graft viability and found out: fat cell viability increases according to the diameter of the cannula reference24reference25reference26. And blunt bore cannulas of 4 to 5mm should be used for fat harvesting.
Don’t be afraid of large cannulas: blunt, bore cannulas are safer, as they pierce less easy and bear a lower risk for perforation!
Key to safe lipofilling is the permanent palpable and or visual control of the cannulas tip. Many experts bend their infiltration cannulas about 30 to 45 degrees, which eases aiming the tip towards the skin surface reference71.

Handling the infiltration cannula
Roller Pump
Autologous fat grafting for gluteoplasty affords infiltrating graft amounts of 300 to more than 1000cc per side; for this maneuver, manual graft preparation and injection is not advisable: roller pumps provide even application in “no touch”- technique using a closed system. Additionally, a roller pump shortens the procedure time and the risk for thromboembolic complications reference28
Gluteal Implant Instruments
Accurate Pocket preparation is key in implant-based buttocks augmentation; besides light hooks, instruments such as a Bayonet dissector and spatulas ease muscle dissection and keep it less traumatic reference11.
Avoid sharp instruments and cautery inside your muscle pocket. Three step blunt instrument dissection is a safe, atraumatic and efficient way to get your pocket prepared reference11
Gluteal Implants
Patient anatomy dictates implant selection reference29; likewise in breast surgery, there are various forms of silicone implants approved for gluteoplasty: round, anatomical and spherical; they vary in terms of projection, diameter, width and surface. In 2019 the first case of ALCL after implant based gluteoplasty had been described reference19, proofing that gluteal implants require identical precautions as silicone breast implants.
08
Technique
Technique
Do not let the patient choose the technique - use the technique needed to get the result, the patient asks for!
Temperature management is key to lower the thromboembolic risk to a minimum: Control the temperature management and make sure patients do not cool down: heating blankets/ prewarmed warmed tumescence fluid and or preheating the patient is essential, as a majority of the body will not be coverable during the procedure addressing the entire core and if necessary extremities during lipoaspiration
No matter which technique is used: always mark the patient standing!
Gluteoplasty by autologous fatgrafting reference08reference31reference32reference33reference34reference35reference36
Gluteal Lipoinjection performed in a systematized manner, following protocols will provide predictable and standardized results:
Preoperative markings
Markings, identifying the zones of liposuction and lipofilling are obvious.
Horizontal and vertical buttock midlines as well as the infragluteal fold serve as very important checkpoints
Additionally, danger triangles (content: major gluteal vessels and sciatic nerve) can be useful, when drawn on each buttock side: apex of the triangle ist the posterior superior iliac spine. The inferior lateral point is located at the greater trochanter and the inferior medial post is at the ischial tuberosity reference09.
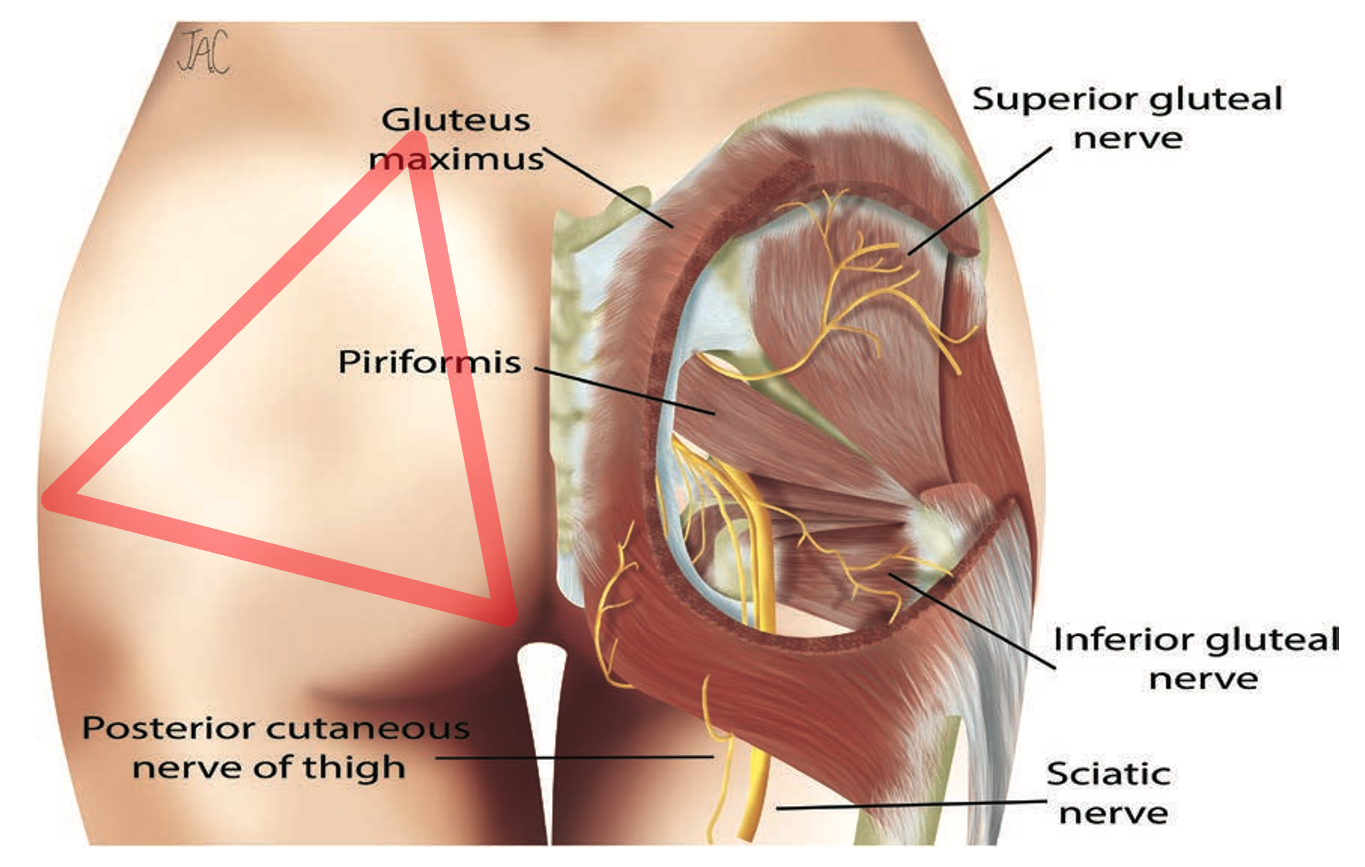
Danger triangle in buttock augmentation.
Lipoaspiration/ Fat- graft harvesting
When performing larger volume (>100 cc) fat transfer, there is no significant difference in adipose cell viability and later take rates among donor sites such as abdomen, flank, thighs, or knees. reference64
Lipoharvest will be performed according to zones in various positions: supine, lateral prone and or decubitus ensure that the patient is quite mobile on the operation table. Access incisions next to the buttocks should be placed suitable for later infiltration: in the gluteal crease, natal cleft and posterior iliac crest.
Many ways of conventional liposuction exist. No matter which method is used, it should be fast, sterile, gentle to the donor site and gentle to the harvested fat cells, leave no irregularities and it should be less exhausting for the surgeon.
Simultaneous separation and tumescence of fat reference31 reference65 or "SAFE- Lipo" - Separation, Aspiration and Fat Equalization - Liposuction Technique is the recommended technique of preparing the donor site before liposuction: Separation of the subcutaneous fat layer emulsifies the target fat without injuring the stromal blood vessel network. After aspiration, the remaining fat emulsion prevents adherence or collapse of the dermis down to the fascia. The act of liposuction can be performed in various ways, waterjet- assisted, ultrasound assisted, pure manually or power assisted; altogether, larger bore multi-whole cannulas (>4,1mm) and low-pressure suction is recommended to minimize blood loss and improve adipocyte viability reference66 .There is no evidenced based knowledge concerning a superior method for fat processing reference67 .However, closed systems, such as large sterile canisters with fluid taps are highly recommended as they prevent contamination, enable simultaneous separation and tumescence of fat and keep the quantity of manipulation and potential damage to the transplant tissue as low as possible.
Once the fat layer and excess liquid (blood and tumescence) separate, the liquid is decanted off and the lipoaspirate is transferred to injection cannulas, ideally power assisted. Centrifugation in large volume lipo- transfer cases is uncommon, neither is there enough data support to recommend adding antibiotics to the harvested fat reference37.
Positioning (see picture under Handling the infiltration cannula/ Equipment- Chapter)
For lipo-infiltrating the gluteus, the patient is placed in a prone position, “jackknife” position (hips flexed in about 30 degrees) by placing silicone roles underneath the anterior superior iliac spines. Additional knee bending avoids lower extremity venous stasis and venous thrombosis. The buttocks being the punctum maximum in this position in combination with an angled infiltration canula eases the surgeon control of the canula tip and remaining strictly above the muscle.
Lipo- Infiltration
After numerous reports of fatal and nonfatal pulmonary fat embolism resulting from gluteal lipofilling, the Aesthetic Surgery Education and Research Foundation (ASERF) formed a Task Force and worked out nine major recommendation for a safe procedure reference38:
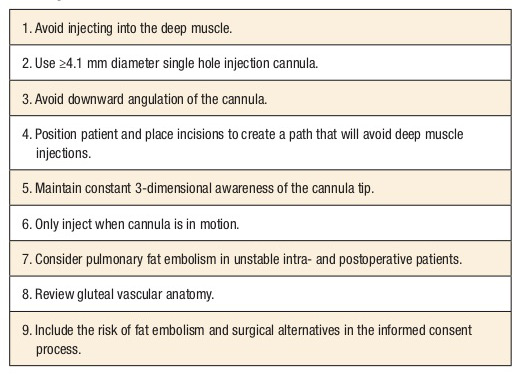
Recommendations from the ASERF Task Force on Gluteal Fat Grafting
The following key principles need to be respected during the process of gluteal fat infiltration: working with rigid, angulated large-bore (4- to 5 mm) blunt cannulas minimizes the risk of venous injury reference39 or penetration into the musculature due to better control. Additionally, viability of adipocytes is improved reference68.
We infiltrate with blunt exploding-tip basket cannulas, which further increases the diameter of the cannula tip.
Injecting only while cannula is in motion has two reasons: it prevents direct and continuous injection into a vessel and spreads the fat grafts even into the subcutaneous tissue scaffold with a higher chance of adequate lobular diffusion and graft take. The risk of Bolus infiltration and consecutive oil cysts is minimized. By using a power-assisted liposuction device and automated roller pump in an off-label manner Expansion, Vibration and automated Lipofilling reference33 has become safer compared with manual axial grafting! Instead of wasting muscular energy, the nondominant hand remains free to continually palpate and control the injection cannulas exact position and tip reference09 reference33.
Any learning curve is accelerated by a visualized feedback: getting to know the total thickness of the gluteal subcutaneous fat (i.e., the safe space) allows surgeons to estimate their cannulas motion range: ultrasound is a suitable, quick and non-invasive way to confirm safe performance during buttock augmentation reference40
Overfilling the recipient site with excessive graft pressure should be avoided reference41reference42reference43 ! Overfilling theoretically bears the risk of fat embolism: it can lead to pressure gradients that favor fat entrance into a possibly injured lower pressure vein lumen. Besides, overfilling can reduce oxygen diffusion capabilities, decreases the amount of graft survival, impairs skin perfusion and leads to oil cysts. However, there is no formula for optimal fill volumes as quantities applied depend on individual tissue characteristics and tissue compliance.
Infiltrate zone by zone altering from side to side and to overview the amounts applicated each area.
You notice the point of maximal infiltration when the tissue feels similar to that achieved during tumescent infiltration; another sign of maximal filling of one zone is achieved, when fat starts pouring out the incision port during grafting
Postoperative Care
Compression garments need to be placed postoperatively reference37 supporting the liposuction donor sites and minimizing the risk for bleeding.
Don’t choose compression garments, that are too tight , as they bear additional risk for thromboembolism and skin burns due to initial numbness.
Standard postoperative deep venous thrombosis prophylaxis depending on the patients Caprini Score is as evident as early mobilization reference69. In terms of postoperative positioning, again, there is not enough data support to confirm keeping the patient away from sitting in order to avoid pressure off the grafted zones; nevertheless no direct sitting is strongly recommended for a minimum of 2 weeks reference44reference45.
Our patients are equipped with a foamed bar that they can start sitting on; while placing it underneath the posterior thighs, the gluteus remains free. Our patients go back to normal daily routine after four weeks.
Consider Lymph drainage to speed up the process of postoperative swelling and edema
Gluteoplasty by Gluteal Implants/ Composite- or Hybrid- Buttock Augmentationreference11reference46reference47reference48reference49reference50
Aesthetic buttocks augmentation started as “implant dominant” procedure; the reason why aesthetic approaches recently favored fat transplantations was the high complication rate resulting from early trial and error methods used for gluteal implants reference51referece52 : Especially superficial augmentation planes (subcutaneous and subfascial planes) are prone to dislocation, visibility, late seroma and discomfort(48), sometimes after some years, when connective tissue including the fascia loosens. A recent Metanalysis investigating differences in complication rates showed buttock implants having the highest complication rate of 31.4%, whereas fat grafting had the lowest 6.8% amongst gluteoplasty procedures(53). Nevertheless, implants do have a value set, especially in thin patients with a BMI from under 20 to 25kg/m2, not providing enough transplant material or patients with flat buttocks particularly asking for projection. Therefore, sophisticated methods, mostly with intramuscular muscle pocket positioning have been developed and deep sub- and intramuscular pocket dissection for implant based buttock augmentation optimized reference48referece52reference54. Similar to breast augmentation surgeons lately started combining both techniques, alloplastic and autologous gluteus augmentation, called hybrid or composite buttock augmentation; this guarantees reliable core projection and surrounding the implant by autologous fat for the natural feeling, appearance and if desired hip management reference11.
Composite buttock augmentation is said to de- risk the complication rate of both methods as smaller implants for core projection and less amounts of fat are needed than in a procedure using only alloplastic or autologous implants reference11

Eight weeks after composite Buttock augmentation
General anesthesia and additional spinal blocks are recommended for this procedure.
Preoperative Markings
Markings depend on the implant pocket and if planned, additional fat grafting in terms of composite buttock augmentation:
In case of intramuscular implant positioning, only incisions need to be marked, pocket location is determined by course and dimension of the gluteal muscles. If composite buttock augmentation is planned, Aslani recommends marking not only the implant incisions, but also the target zone of autologous lipofilling:
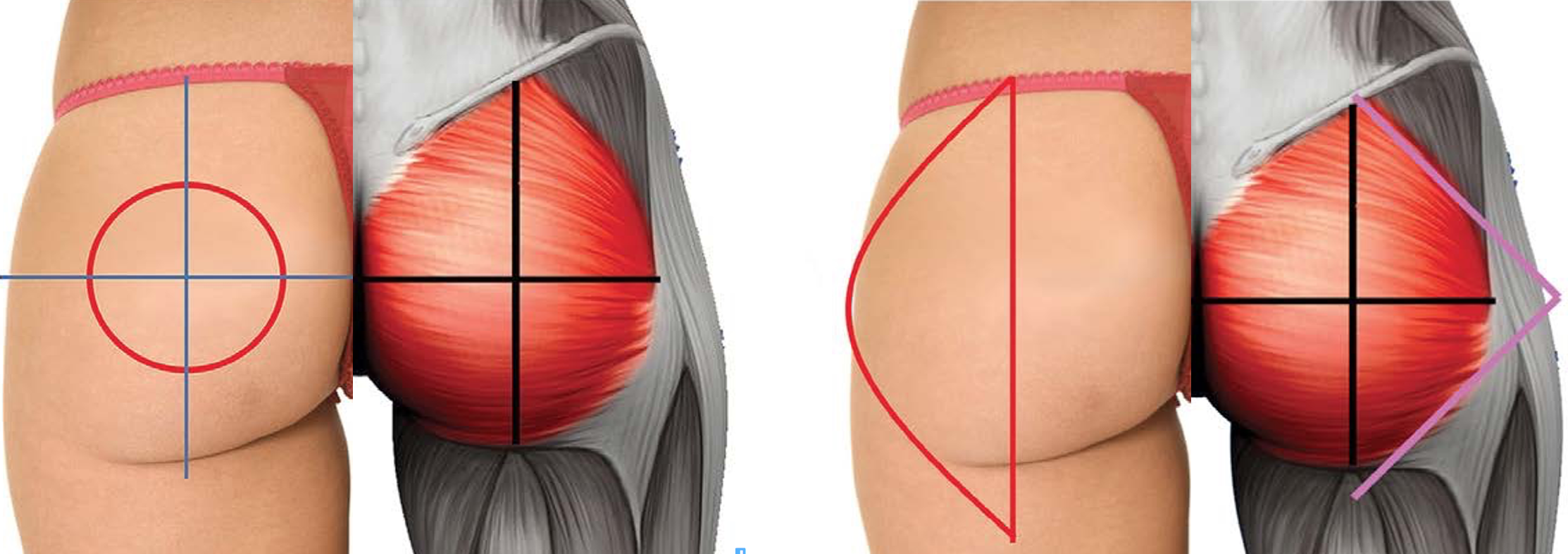
Vertical- horizontal buttock lines and Medietas C- Point for composite buttock augmentation
Incision Marking
Various access options have been reported: The choice of incision is either single intergluteal or bilateral paramedian. Also inverted heart shaped incisions with the base of the heart being the most cranial ending of the natal crease have been described, as it exposes the muscle reference48. In a 2013 survey by Mofid and colleagues of US and international surgeons, 53% preferred a single midline incision(55). Using two separate incisions prevents soft tissue dehiscence and unpleasant pterygium development inside the natal cleft; additionally potential communication between both pockets is impossible in case one side develops seroma, infection etc.. In case two separate incisions are planned: paramedian markings, approximately 1cm lateral to both sides of the natal cleft running vertical for five to six centimeters are drawn reference11.
The experts preference are two separate incisions; if placed correct, they will be covered by swim- and underwear, scarring usually is very pleasing in this area and in case dehiscence, seroma, etc. affects one side, affection of the other side/ pocket is no option.
Fat Harvesting
We kindly refer to chapter "Gluteoplasty by autologous fat harvesting".
Pocket Dissection
Choice of plane: Buttock implants have been placed deep (sub- or intramuscular) or superficial (subfascial or subcutaneous).
Implant based buttock augmentation is a clear indication for thin patients not providing enough autologous fat. Therefore, validity of superficial buttock implant planes is doubted as the risk of visibility in thin patients is high.
The expert exclusively performs intramuscular or dual plane pocket dissection. Dual plane implant positioning is characterized by a sub muscular pocket design in the superior part and an intramuscular plane in the inferior part of the implant pocket.
Deep placement is least likely to present implant visibility and is best suited for thin patients that lack enough autologous fat and depend on alloplastic buttocks augmentation: Incisions are made where marked and dissection towards the muscle is completed; make sure to leave enough tissue on the natal crease to prevent perfusion impairment. If available, ease pocket dissection by hydrodissection using temeszenz fluid. Using a sequence of different instruments (Progressive instrument dissection) enables define a proper pocket. Before blunt pocket dissection: Paramedial cut the gluteus muscle vertical to a depth of 2- 4 cm about 2 cm lateral from its sacral/ coccyx origin. Important is a thick muscle flap plane to perfectly cover the implant and primarily close the incision after implant positioning. This step is followed by even horizontal undermining along the course of the muscle fibers in terms of muscle splitting leaving the same amount of muscle above and behind the future implant comparable to a sandwich reference48.
Keep the angle of your instrument parallel to the muscle which curves anteriorly to preserve enough muscle thickness reference11reference48
In case of Composite Buttock augmentations: Lipo-Infiltration
Periprosthetic fat grafting is defined as fat infiltration through separate incisions other than the implant, into distinct, subcutaneous planes around the implant reference11. During the infiltration process, soaked towels serve as spacer inside the intramuscular pockets, hemostasis- control and as discrete blunt pocket enlargement.
Implant Insertion
Drains are placed into pockets after meticulous hemostasis. Inserting gluteal implants is comparable to breast implants and the same rules need to be respected
During alloplastic gluteal augmentation, temporarily close the anus with a betadine-soaked gauze
Implant size is limited by anatomy of the muscle: if the muscle coverage is too thin or the implant to big, superficial muscle fibers will spread apart at the weakest point “implant show” will occur (often laterally). If the muscle base is too thin ischiatic neurapraxia may occur. In 2019 the expert published a level 4 evidence based retrospective study of a series of 147 implant based composite buttock augmentations: a trend towards the end of this series demonstrated a clear preference towards round implants (volumes from 180 to 370 cc) due to malrotation of anatomical implants reference11.
Key to proper healing and pocket stability is meticulous closure of a dry pocket via readdressing muscle, fascia and skin by.
Postoperative Management
Postoperatively, patients are dressed in compression garments, drains should remain 5- 7 days and buttocks offload is strictly recommended 4 to 6 weeks.
Gluteoplasty by Autologous Flap Augmentation reference56/ Postbariatric Gluteoplasty
Similar to cosmetic patients, management of postbariatric patients is described in literature and includes completion of certain conditions: weight loss with a stable body mass index of ideally less than 32, smoking cessation, nutritional assessment, anemia screening, usage of mechanical prophylaxis against thromboembolism and consideration for usage of chemoprophylaxis with low molecular weight or unfractionated heparin. Facilities need to be accredited and special attention needs to be payed concerning positioning and patients body temperature. Massive weight loss patients have excess skin and fat between the iliac crest and superior gluteal margin, in extreme cases sagging down towards the posterior thigh. Like cosmetic patients they are seeking for a round harmonic buttock contour not just losing the excess of skin. All procedures common is the resection of excessive skin for a buttock lift. However methods vary in, how projection is gained: either autologous pedicled flaps, autologous fat grafting or alloplastic augmentation is described reference17. Focus of the following description is the pedicled flap based autologous gluteoplasty: various methods of adipocutaneous gluteal flaps (mostly superiorly based) exist as profound knowledge concerning soft tissue perfusion of the gluteal region is present in form of : 20 to 25 perforating branches reference57reference58. The ideal flap should be versatile, rely on a constant vascularization, give good projection. Scars need to be covered easy by apparel.
Preoperative Planning
The estimated final scar is marked after the patient is asked for her/ his favorable under- and swimwear habits for future scar concealing. By moving the central gluteal tissue upwards, one can estimate the curvilinear upper border of the buttocks, which is fused at the sacrum to an aesthetically pleasing V- shape crease. Then, the pinch method is used to estimate the amount of possible skin resection.
Double Check the resection zone by letting the patient bend forward to prevent over-resection.
Similar to abdominoplasty, the upper and lower resection lines may meet slightly ventral at the flanks to avoid dog ears. Additional liposuction of the transitory zone around the waist and sacrum may be helpful in patients still providing accumulated fat deposits in the flanks, so called love handles. Besides, lipofilling may be the ideal tool to camouflage irregularities or slightly visible borders of the flaps.
Whether additional projection needs to be reconstructed has to be discussed with the patient; Schmitt et al published a Classification of the gluteus initial situationreference59 as well as an additional algorithm for operative planning (see table and algorithm concerning patient classification after massive weight loss focusing on back fat distribution and buttock augmentation) :
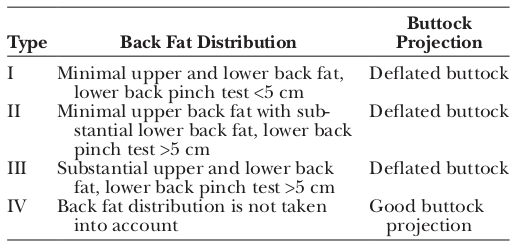
Patient classification after massive weight loss focusing on back fat distribution und buttock projection
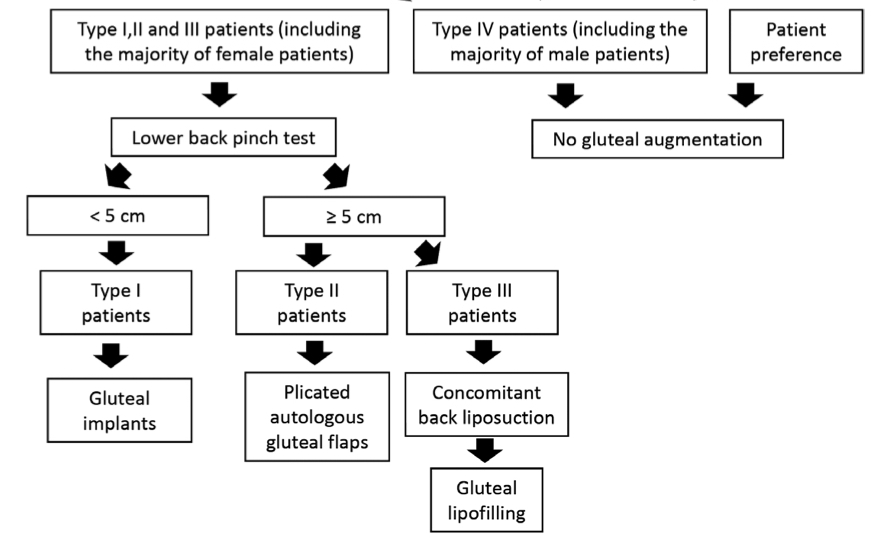
Algorithmic approach to gluteal augmentation in massive weight loss patients undergoing a lower body-lift procedure
Patient Positioning
Patients should be placed in a prone “jackknife” (hips flexed in about 30 degrees) position, by placing silicone roles underneath the anterior superior iliac spines and ankles avoiding lower extremity venous stasis.
Technique
There are various techniques for simultaneously addressing not only the loose and ptotic skin excess, but also regain natural projection after weight loss by pedicled tissue augmentation: All have in common the auto- implant based creation of buttock projection via perforator-, a random or perforator based pedicled flaps reference72: in general, the marked flap is deepithelialized dissected down to the fascia and fixed epimuscular into an undermined pocket; partial splitting of the muscle to ease flap mobilization has been described reference56. Depending on the rigidity of the subcutaneous tissues, it is sometimes favorable to transpose the flap as a turn-down flap rather than to rotate the flap inferiorly. Coverage of the flaps is gained by pulling the mobile buttock skin together.
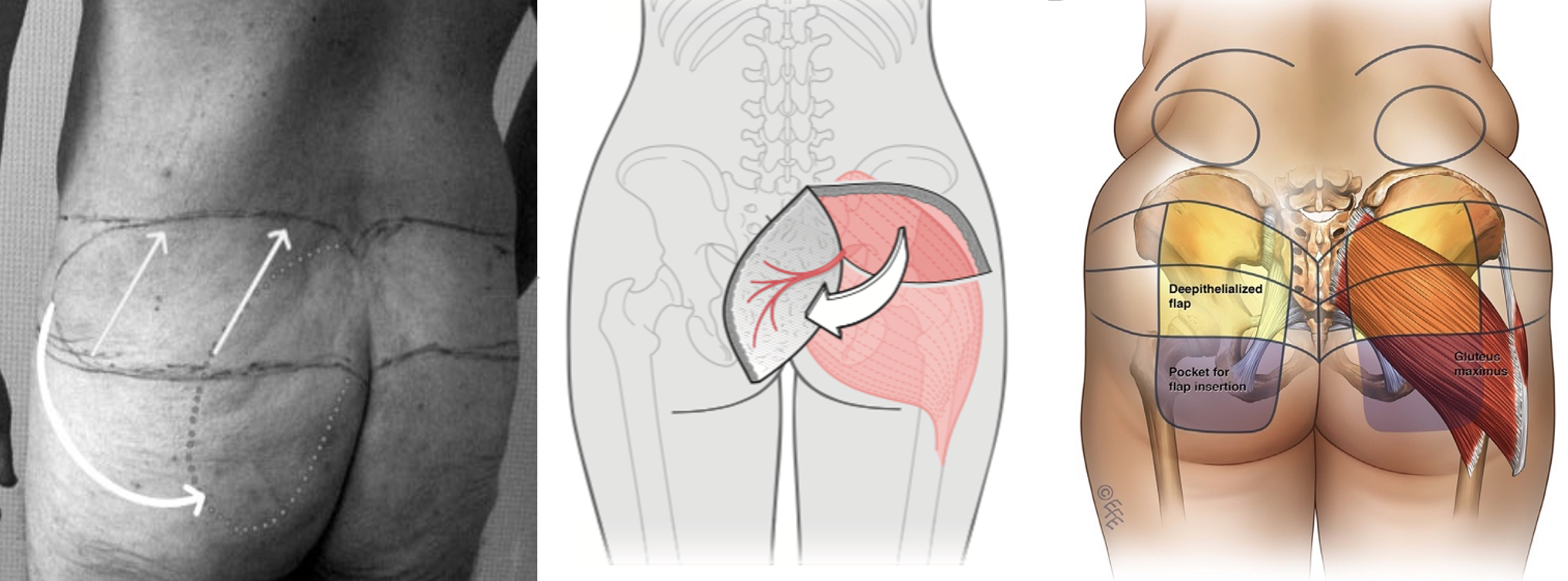
Autoimplant based creation of buttock projection via perforator-, random or perforator based pedicled flaps
Doppler and Indocyanine Green perfusion mapping are a valid tool for intraoperative testing of flap perfusion and perforators.
Complications
Seroma is the most common complication of postbariatric buttock- surgery and can be prevented by avoiding dead space, using progressive tension sutures and use drains. Fibrin glue or preservation of a thin fat layer is also described to reduce the incidence of seroma without scientific proof reference70 . Minimizing skin tension, respecting tissue perfusion and modifying the procedure to the patient anatomy allows a safe gluteal augmentation!
Postprocedural Care
Postoperative care is similar to other gluteal procedures including compression garments, drainages, positioning restrictions and antithrombotic prophylaxis; most important: early mobilisation is key. However it may vary from surgeon to surgeon.
09
Conclusion
Conclusion
Gluteoplasty used to be underestimated and had a simple procedure reputation; with increasing demand, simultaneously increasing nontolerable complications such as lethal pulmonary embolism after intramuscular fat infiltration occurred; buttock augmentation was about to be banned and forbidden. Thanks to meticulous investigation, experimental and clinical studies, task forces, and published papers the technical error is well-known: intramuscular fat embolism bears high risk of venous vessel damage and direct or indirect fat embolism: as a consequence, sophisticated maneuvers and mandatory safety recommendations have been developed; in terms of techniques, operative strategies and respect for deep anatomic structures and proper patient positioning besides industry catched up and specialists have grown as well as gluteoplasty societies and educational and congress meetings started. Bodycontouring, large Volume Fat harvesting and Fat grafting are fields that are key to a successful management of the entire spectrum of gluteoplasties and need to be mastered as well as implant handling or experience in Flap surgery: However key to successful buttock surgery is understanding the buttocks anatomy and concomitant appearance and tissue behavior of this region. Performing gluteoplasty requires proper instrumentation, knowledge and training reference33. With respect and a repertoire of various techniques for various conditions highly pleasant results can be achieved and rewarded by the patient.
Images
Intergluteal crest variations
Gluteal aesthetic units
The 4 buttocks shapes
The square buttock demonstrating the role of the width to hight- ratio
Inferior gluteal base width
Inferior gluteal base width and slope
Gluteus maximus muscle volume distribution
Lateral buttock zones
Gluteal Ptosis grade
Handling the infiltration cannula
Danger triangle in buttock augmentation.
Recommendations from the ASERF Task Force on Gluteal Fat Grafting
Vertical- horizontal buttock lines and Medietas C- Point for composite buttock augmentation
Patient classification after massive weight loss focusing on back fat distribution und buttock projection
Algorithmic approach to gluteal augmentation in massive weight loss patients undergoing a lower body-lift procedure
Autoimplant based creation of buttock projection via perforator-, random or perforator based pedicled flaps
Pre and Postoperaive autologous gluteal fat infiltration
Pre and postoperative autologous gluteal fat infiltration
Eight weeks after composite Buttock augmentation
References
[1]
A Changing Paradigm: The Brazilian Butt Lift Is Neither Brazilian Nor a Lift-Why It Needs To Be Called Safe Subcutaneous Buttock Augmentation, Del Vecchio DA, Rohrich RJ, Plast Reconstr Surg , 2020
[2]
Composite Buttock Augmentation: The Next Frontier in Gluteal Aesthetic Surgery, Aslani A, Del Vecchio DA, Plast Reconstr Surg, 2019
[3]
Clinical Anatomy in Aesthetic Gluteal Contouring, Centeno RF, Sood A, Young VL, Clin Plast Surg , 2018
[4]
Gluteal Ligamentous Anatomy and Its Implication in Safe Buttock Augmentation, Ghavami A, Villanueva NL, Amirlak B, Plast Reconstr Surg, 2018
[5]
Gluteal region morphology: the effect of the weight gain and aging, Babuccu O, Gozil R, Ozmen S, et al, Aesthetic Plast Surg , 2002
[6]
Clinical Anatomy in Aesthetic Gluteal Contouring, Centeno RF, Sood A, Young VL, Clin Plast Surg , 2018
[7]
Classification System for Gluteal Evaluation: Revisited, Mendieta CG, Sood A, Clin Plast Surg, 2018
[8]
Objectifying the Risk of Vascular Complications inGluteal Augmentation With Fat Grafting: A Latex Casted Cadaveric Study, Ordenana C, Dallapozza E, Said S, et al, Aesthet Surg J , 2020
[9]
Gluteal Augmentation and Enhancement of the Female Silhouette: Analysis and Technique, Mendieta C, Stuzin JM, Plast Reconstr Surg, 2018
[10]
Universal allure of the hourglass figure: an evolutionary theory of female physical attractiveness, Singh D, Clin Plast Surg, 2006
[11]
Gluteal Implants Versus Autologous Flaps in Patients with Postbariatric Surgery Weight Loss: A Prospective Comparative Study of 3-Dimensional Gluteal Projection After Lower Body Lift, Levan P, Bassilios Habre S, Aesthet Surg J , 2017
[12]
Gluteal Augmentation and Enhancement of the Female Silhouette: Analysis and Technique, Mendieta C, Stuzin JM, Plast Reconstr Surg, 2018
[13]
Classification System for Gluteal Evaluation: Revisited, Mendieta CG, Sood A, Clin Plast Surg, 2018
[14]
Classification System for Gluteal Evaluation: Revisited, Mendieta CG, Sood A, Clin Plast Surg, 2018
[15]
Gluteal Implant-Associated Anaplastic Large Cell Lymphoma, Mendes J, Jr., Mendes Maykeh VA, Frascino LF, et al, Plast Reconstr Surg, 2019
[16]
Perioperative Management of Female Hormone Medications, Seim LA, Irizarry-Alvarado JM, Curr Clin Pharmacol , 2017
[17]
The Science of Fat Grafting, Shih L, Davis MJ, Winocour SJ, Semin Plast Surg , 2020
[18]
Local anesthetics have a major impact on viability of preadipocytes and their differentiation into adipocytes, Keck M, Zeyda M, Gollinger K, et al, Plast Reconstr Surg, 2010
[19]
The Impact of Lidocaine on Adipose-Derived Stem Cells in Human Adipose Tissue Harvested by Liposuction and Used for Lipotransfer, Grambow F, Rutkowski R, Podmelle F, et al, Int J Mol Sci , 2020
[20]
The impact of liposuction cannula size on adipocyte viability, Kirkham JC, Lee JH, Medina MA, 3rd, et al, Ann Plast Surg, 2012
[21]
The role of cannula diameter in improved adipocyte viability: a quantitative analysis, Ozsoy Z, Kul Z, Bilir A, Aesthet Surg J , 2006
[22]
The effects of the size of liposuction cannula on adipocyte survival and the optimum temperature for fat graft storage: an experimental study, Erdim M, Tezel E, Numanoglu A, et al, J Plast Reconstr Aesthet Surg, 2009
[23]
Vermeiden von Komplikationen beim „Brazilian butt lift“, Aslani Alexander, Mandlik Veronika, del Vecchio Daniel, Springer Science and Business Media LLC, 2018
[24]
Safest Practices for Autologous Buttock Augmentation With Fat Grafting Using a Roller Pump Injection Technique, Everett M, Morales R, Jr., Newall G, et al, Aesthet Surg J, 2018
[25]
Composite Buttock Augmentation: The Next Frontier in Gluteal Aesthetic Surgery, Aslani A, Del Vecchio DA, Plast Reconstr Surg, 2019
[26]
Composite Buttock Augmentation: The Next Frontier in Gluteal Aesthetic Surgery, Aslani A, Del Vecchio DA, Plast Reconstr Surg, 2019
[27]
Practice-Based Patient Management Strategies in Gluteal Augmentation with Implants, Senderoff DM, Aesthet Surg J, 2018
[28]
Gluteal Implant-Associated Anaplastic Large Cell Lymphoma, Mendes J, Jr., Mendes Maykeh VA, Frascino LF, et al, Plast Reconstr Surg, 2019
[29]
Safe Gluteal Fat Graft Avoiding a Vascular or Nervous Injury: An Anatomical Study in Cadavers, Alvarez-Alvarez FA, Gonzalez-Gutierrez HO, Ploneda-Valencia CF, Aesthet Surg J , 2019
[30]
Staying Safe during Gluteal Fat Transplantation, Villanueva NL, Del Vecchio DA, Afrooz PN, et al, Plast Reconstr Surg, 2018
[31]
Separation, Aspiration, and Fat Equalization: SAFE Liposuction Concepts for Comprehensive Body Contouring, Centurion P, Savitzky MJ, Plast Reconstr Surg , 2017
[32]
Improvement of the Gluteal Contour: Modern Concepts with Systematized Lipoinjection, Cardenas-Camarena L, Duran H, Clin Plast Surg, 2018
[33]
Expansion Vibration Lipofilling: A New Technique in Large-Volume Fat Transplantation, Del Vecchio D, Wall S, Jr, Plast Reconstr Surg , 2018
[34]
Expansion Vibration Lipofilling: A New Technique in Large-Volume Fat Transplantation: Correction, Wall S, Jr, Plast Reconstr Surg, 2018
[35]
Subcutaneous-Only Gluteal Fat Grafting: A Prospective Study of the Long-Term Results with Ultrasound Analysis, Cansancao AL, Conde-Green A, David JA, et al, Plast Reconstr Surg , 2019
[36]
Gluteal Augmentation With Fat: Retrospective Safety Study and Literature Review, Kalaaji A, Dreyer S, Vadseth L, et al, Aesthet Surg J , 2019
[37]
Staying Safe during Gluteal Fat Transplantation, Villanueva NL, Del Vecchio DA, Afrooz PN, et al, Plast Reconstr Surg, 2018
[38]
In Search of Improved Fat Transfer Viability: A Quantitative Analysis of the Role of Centrifugation and Harvest Site, Rohrich Rod J., Sorokin Evan S., Brown Spencer A., Ovid Technologies (Wolters Kluwer Health), 2004
[39]
Separation, Aspiration, and Fat Equalization: SAFE Liposuction Concepts for Comprehensive Body Contouring, Centurion P, Savitzky MJ, Plast Reconstr Surg , 2017
[40]
Breast Reconstruction and Augmentation Using Pre-Expansion and Autologous Fat Transplantation, Khouri Roger, Del Vecchio Daniel, Elsevier BV, 2009
[41]
Fat Grafting, Gir Phanette, Brown Spencer A., Oni Georgette, Kashefi Nathalie, Mojallal Ali, Rohrich Rod J., Ovid Technologies (Wolters Kluwer Health), 2012
[42]
A Classification of Clinical Fat Grafting, Del Vecchio Daniel, Rohrich Rod J., Ovid Technologies (Wolters Kluwer Health), 2012
[43]
Fat Grafting for Gluteal Augmentation: A Systematic Review of the Literature and Meta-Analysis, Conde-Green A, Kotamarti V, Nini KT, et al, Plast Reconstr Surg, 2016
[44]
Report on Mortality from Gluteal Fat Grafting: Recommendations from the ASERF Task Force, Mofid MM, Teitelbaum S, Suissa D, et al, Aesthet Surg J , 2017
[45]
Commentary on: Report on Mortality from Gluteal Fat Grafting: Recommendations from the ASERF Task Force, Wall S, Jr., Del Vecchio D, Aesthet Surg J , 2017
[46]
Fat Grafting, Gir Phanette, Brown Spencer A., Oni Georgette, Kashefi Nathalie, Mojallal Ali, Rohrich Rod J., Ovid Technologies (Wolters Kluwer Health), 2012
[47]
Expansion Vibration Lipofilling: A New Technique in Large-Volume Fat Transplantation, Del Vecchio D, Wall S, Jr, Plast Reconstr Surg , 2018
[48]
Staying Safe during Gluteal Fat Transplantation, Villanueva NL, Del Vecchio DA, Afrooz PN, et al, Plast Reconstr Surg, 2018
[49]
Expansion Vibration Lipofilling: A New Technique in Large-Volume Fat Transplantation, Del Vecchio D, Wall S, Jr, Plast Reconstr Surg , 2018
[50]
Influence of Age, Sex, and Body Mass Index on the Thickness of the Gluteal Subcutaneous Fat: Implications for Safe Buttock Augmentation Procedures, Frank K, Casabona G, Gotkin RH, et al, Plast Reconstr Surg , 2019
[51]
Determining the Safety and Efficacy of Gluteal Augmentation: A Systematic Review of Outcomes and Complications, Sinno S, Chang JB, Brownstone ND, et al, Plast Reconstr Surg , 2016
[52]
Results and long-term patient satisfaction after gluteal augmentation with platelet-rich plasma-enriched autologous fat, Willemsen JC, Lindenblatt N, Stevens HP, Eur J Plast Surg , 2013
[53]
The graft-to-capacity ratio: volumetric planning in large-volume fat transplantation, Del Vecchio DA, Del Vecchio SJ, Plast Reconstr Surg, 2014
[54]
Fat Grafting for Gluteal Augmentation: A Systematic Review of the Literature and Meta-Analysis, Conde-Green A, Kotamarti V, Nini KT, et al, Plast Reconstr Surg, 2016
[55]
Assessment of Postoperative Venous Thromboembolism Risk in Plastic Surgery Patients Using the 2005 and 2010 Caprini Risk Score, Pannucci Christopher J., Barta Ruth J., Portschy Pamela R., Dreszer George, Hoxworth Ronald E., Kalliainen Loree K., Wilkins Edwin G., Ovid Technologies (Wolters Kluwer Health), 2012
[56]
Contouring of the gluteal region in women: enhancement and augmentation, Ali A, Ann Plast Surg, 2011
[57]
Autologous gluteal lipograft, Nicareta B, Pereira LH, Sterodimas A, et al, Aesthetic Plast Surg , 2011
[58]
Composite Buttock Augmentation: The Next Frontier in Gluteal Aesthetic Surgery, Aslani A, Del Vecchio DA, Plast Reconstr Surg, 2019
[59]
Gluteal Augmentation with Silicone Implants: A New Proposal for Intramuscular Dissection, Andrade GA, Coltro PS, Ando A, et al, Aesthetic Plast Surg, 2017
[60]
Subfascial Gluteal Implant Augmentation, de la Pena Salcedo JA, Gallardo GJ, Alvarenga GE, Clin Plast Surg , 2018
[61]
Intramuscular Gluteal Augmentation: The XYZ Method, Gonzalez R, Gonzalez R, Clin Plast Surg , 2018
[62]
Intramuscular Gluteal Augmentation with Implants Associated with Immediate Fat Grafting, Godoy PM, Munhoz AM, Clin Plast Surg , 2018
[63]
Tridimensional Combined Gluteoplasty: Liposuction, Buttock Implants and Fat Transfer, Cardenas-Camarena L, Trujillo-Mendez R, Diaz-Barriga JC, Plast Reconstr Surg, 2020
[64]
Complications of buttocks augmentation: diagnosis, management, and prevention, Bruner TW, Roberts TL, 3rd, Nguyen K, Clin Plast Surg, 2006
[65]
Intramuscular gluteal implants: 15 years' experience., Vergara R, Amezcua H, Aesthet Surg J , 2003
[66]
Intramuscular Gluteal Augmentation: The XYZ Method, Gonzalez R, Gonzalez R, Clin Plast Surg , 2018
[67]
Intramuscular gluteal implants: 15 years' experience., Vergara R, Amezcua H, Aesthet Surg J , 2003
[68]
Intramuscular technique for gluteal augmentation: determination and quantification of muscle atrophy and implant position by computed tomographic scan., Serra F, Aboudib JH, Marques RG, Plast Reconstr Surg, 2013
[69]
Composite Buttock Augmentation: The Next Frontier in Gluteal Aesthetic Surgery, Aslani A, Del Vecchio DA, Plast Reconstr Surg, 2019
[70]
Composite Buttock Augmentation: The Next Frontier in Gluteal Aesthetic Surgery, Aslani A, Del Vecchio DA, Plast Reconstr Surg, 2019
[71]
Intramuscular Gluteal Augmentation: The XYZ Method, Gonzalez R, Gonzalez R, Clin Plast Surg , 2018
[72]
Composite Buttock Augmentation: The Next Frontier in Gluteal Aesthetic Surgery, Aslani A, Del Vecchio DA, Plast Reconstr Surg, 2019
[73]
Intramuscular Gluteal Augmentation: The XYZ Method, Gonzalez R, Gonzalez R, Clin Plast Surg , 2018
[74]
Composite Buttock Augmentation: The Next Frontier in Gluteal Aesthetic Surgery, Aslani A, Del Vecchio DA, Plast Reconstr Surg, 2019
[75]
Intramuscular Gluteal Augmentation: The XYZ Method, Gonzalez R, Gonzalez R, Clin Plast Surg , 2018
[76]
Composite Buttock Augmentation: The Next Frontier in Gluteal Aesthetic Surgery, Aslani A, Del Vecchio DA, Plast Reconstr Surg, 2019
[77]
Composite Buttock Augmentation: The Next Frontier in Gluteal Aesthetic Surgery, Aslani A, Del Vecchio DA, Plast Reconstr Surg, 2019
[78]
Autologous Flap Gluteal Augmentation: Split Gluteal Flap Technique, Sozer SO, Erhan Eryilmaz O, Clin Plast Surg, 2018
[79]
Gluteal Implants Versus Autologous Flaps in Patients with Postbariatric Surgery Weight Loss: A Prospective Comparative Study of 3-Dimensional Gluteal Projection After Lower Body Lift, Levan P, Bassilios Habre S, Aesthet Surg J , 2017
[80]
Optimization of patient safety in postbariatric body contouring: a current review, Colwell AS, Borud LJ, Aesthet Surg J , 2008
[81]
The microvascular anatomy of superior and inferior gluteal artery perforator (SGAP and IGAP) flaps: a fresh cadaveric study and clinical implications, Georgantopoulou A, Papadodima S, Vlachodimitropoulos D, et al, Aesthetic Plast Surg , 2014
[82]
Lower Body Lift in the Massive Weight Loss Patient: A New Classification and Algorithm for Gluteal Augmentation, Schmitt T, Jabbour S, Makhoul R, et al, Plast Reconstr Surg , 2018
[83]
Post-Bariatric Buttock Contouring with Autogenous Tissue Augmentation, Gerut Zachary E, Georg Thieme Verlag KG, 2006
[84]
Autologous Flap Gluteal Augmentation: Split Gluteal Flap Technique, Sozer SO, Erhan Eryilmaz O, Clin Plast Surg, 2018
[85]
Progressive Tension Sutures: A Technique to Reduce Local Complications in Abdominoplasty, Pollock Harlan, Pollock Todd, Ovid Technologies (Wolters Kluwer Health), 2000
[86]
Expansion Vibration Lipofilling: A New Technique in Large-Volume Fat Transplantation, Del Vecchio D, Wall S, Jr, Plast Reconstr Surg , 2018