["a8c44dc59b3925416e41a96fd36b4c49b244b6f4"]
Otoplasty and Ear Reduction
prominent ear
otapostatis
ear correction
cartilage
3264
3264
Chapter reads
0
0
Chapter likes
5/10
Evidence score
07
7
Images included
01
1
Videos included
01
Abstract
Introduction
The bilateral prominent ear deformity is the most common auricular shape pathology. It is defined by an underdeveloped antihelix combined with an increased mastoid-helix angle. Primary surgical goal is to restore the antihelical fold and reduce the mastoid-helical distance. Various operative procedures have been described and may be divided into cartilage sparing and cartilage invasive techniques. In this article, we present our decision-making protocol on which procedure to choose. In our experience, several techniques may be combined to achieve the optimal esthetic result. For the top auf ear, we prefer scoring rather than cartilage excision to avoid instability and suturing if further correction is needed. In cases of a mastoid-helical angle >50°, cavum reduction often is necessary and should be preferred over ear rotation. An external pressure dressing should be applied after the operation to support the new auricular shape for 1-2 weeks.
02
Introduction
Introduction
The development of the ear conch, middle ear and auditory canal derives from the first and third embryogenic branchial arch. This usually occurs during the first and second trimester of the pregnancy. The external and internal anatomy of the ear prone to ototoxic medication may be affected in different extent during this vulnerable period. Ear dysplasia may be isolated or part of a genetic syndromal disorders. Therefore, extended diagnostics may be necessary to adequately analyze and understand the characteristics of each disease. During the clinical routine of plastic surgeons, a common reason for consultation regarding ear pathologies are prominent ears or otapostasis. This is one of the most common abnormalities with an incidence of about 5% 9 . A genetic inheritance with an an autosomal dominant trait has been described.
Pathophysiologic reason for this appearance are an underdeveloped antihelix combined with an increased mastoid-helix angle (>30°). Furthermore, the skin plication in the upper third of the ear helix may be missing or sparsely developed. The bilateral prominent ear is one of the most common auricular shape pathology5. Unilateral variants are possible but syndromal disorders need to be ruled out. Before planning surgery, exact preoperative analyses of the deformity is necessary to adapt the surgical approach. Exacerbating variants like the Stahl´s ear, Darwin´s tubercle or Mastoid prominence need to respected as well an if present discussed with the patient.
Pathophysiologic reason for this appearance are an underdeveloped antihelix combined with an increased mastoid-helix angle (>30°). Furthermore, the skin plication in the upper third of the ear helix may be missing or sparsely developed. The bilateral prominent ear is one of the most common auricular shape pathology5. Unilateral variants are possible but syndromal disorders need to be ruled out. Before planning surgery, exact preoperative analyses of the deformity is necessary to adapt the surgical approach. Exacerbating variants like the Stahl´s ear, Darwin´s tubercle or Mastoid prominence need to respected as well an if present discussed with the patient.
In general, there are invasive and non-invasive surgical procedures to correct the prominent ear deformity. The invasive procedures may be further subdivided into cartilage sparing, e.g. suturing techniques and cartilage invasive surgery e.g. scoring, cartilage incision and excision. Main focus of the operative intervention lies upon the reconstruction of the antihelical fold.
If a prominent ear deformity is noted during birth, non-invasive glue or splinting techniques may be used to attach the main body of the conch to the mastoid overlying skin. Results are heterogeneous and newborns are rarely presented to the plastic surgeon consulting for ear corrections. Therefore, it is essential to time invasive surgery and adapt to the child’s development. At the end of the third year of life, the ear conch has reached almost 85% of its final size, and surgical interventions are less likely to lead to growth impairment . Furthermore, sociocultural aspects need be considered as school enrollment using starts around this age and bullying as a reason of physical differences may be prevented.
03
Anatomy
Anatomy
Blood supply
The arterial blood supply of the external ear derives from the external carotid artery. Towards the tragus, superior and inferior aspect of the ear, approximately three vessels (superior, medial and inferior auricular artery) deriving from the superficial temporal artery irrigate most of the tissue. The middle and dorsal aspect are supplied by the posterior auricular artery.
Clinical advice: During surgery, the dorsal blood supply may be ligated without concern if exposure of the dorsal concha or mastoid is needed. In trauma situations, the inferior auricular artery most often carries enough blood for nourishing the whole ear.
Clinical advice: During surgery, the dorsal blood supply may be ligated without concern if exposure of the dorsal concha or mastoid is needed. In trauma situations, the inferior auricular artery most often carries enough blood for nourishing the whole ear.
Innvervation
The external ear has has a combined cranial and spinal sensory nerve innervation. The tragus and upper anterior aspect are supplied by the auriculotemporal branch of the mandibular nerve (V3). The lesser occipital (C2, C3) and greater auricular nerve (C2, C3) run with the posterior auricular artery and supply most of the lateral and dorsal skin. The very medial aspect of the ear and the external auditory canal are supplied by the branches from the facial and vagus nerve (stimulation of the auditory canal leeds to coughing during tympanic inspection) . Motor innervation to the intrinsic and extrinsic muscles derive from the facial nerve.
Muscles
There are three extrinsic ear muscles: auricularis anterior, superior and posterior. Their location around the ear is indicated by their names. While the auricularis posterior originates from the mastoid bone, all others derive from the galea aponeurotica. The small anterior muscle inserts into the adjacent helix while the superior and posterior insert into the body of the concha. Clinical advice: Muscle fibers are very subtle are most often not visible during surgery. If found, the may be dissected without concern or need of refixation.
Remind during surgery
To plan individual surgery, the anatomy of the cartilage covering layers needs to be respected. The posterior of the ear comprises of five layers starting from the outside: 1 skin (epidermis/dermis), 2 subcutaneous tissue, 3 postauricular fascia, 4 perichondrium and 5 cartilage. The fascia is the leading structure for the neurovascular supply from the posterior auricular artery and greater auricular nerve.
Benchmark values for the mastoid helical distance for pre- and postoperative evaluation of the ear position 2:
Top of helix
12 mm
Middle third of helix
17 mm
Lobule
20 mm
04
Surgical approach
Surgical approach
For the surgeon, it is possible to choose between nonsurgical, cartilage sparing and cartilage invasive techniques. If chosen, the nonsurgical treatment must be started within the fist 72 hours after birth. It takes advantage of circulating maternal hormones resulting in more pliable cartilage, facilitating the modulation by an external dressing. Different materials like glue, tape or a splint may be chosen for modulation. These need to remain for up to 6-8 weeks to avoid a surgical intervention 10.
If the cartilage sparing procedures the suturing technique described by Mustardé is the basis of what we use in our clinical routine (Figure 3). It allows the creation of the antihelical fold by using permanent side-to-side mattress sutures without damaging the cartilage itself 1
If the cartilage sparing procedures the suturing technique described by Mustardé is the basis of what we use in our clinical routine (Figure 3). It allows the creation of the antihelical fold by using permanent side-to-side mattress sutures without damaging the cartilage itself 1
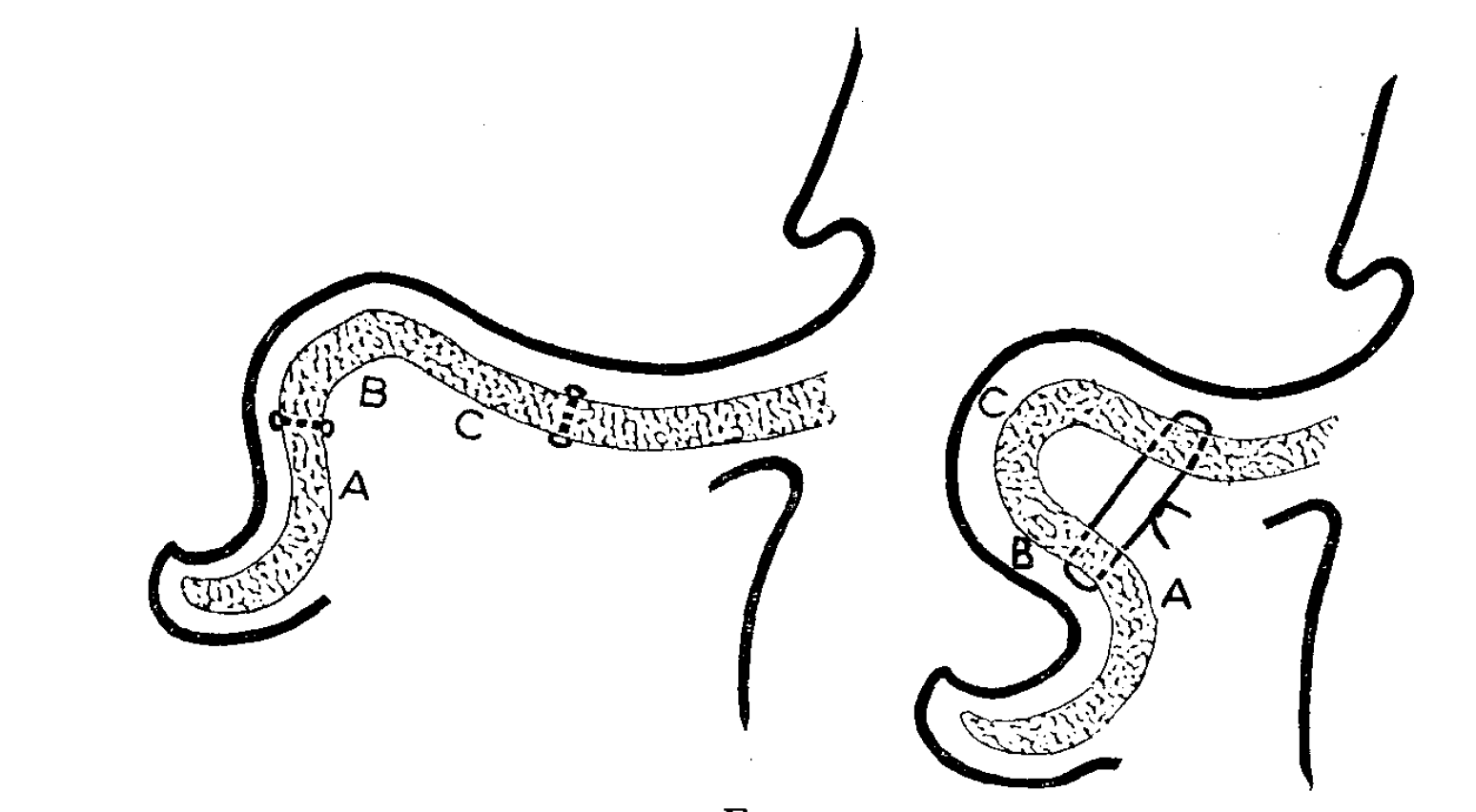
Figure 3
During preoperative planning, the ear is folded back and the new apex of the antihelical fold is marked. In surgery, the position of the sutures is assigned through a full thickness puncture by an inked covered needle at least 7mm medial or lateral from the new summit line. To prevent skin plication after ear reduction, an ellipse of about 3 x 1 cm of the medial side to the proposed new antihelix is resected followed by blunt skin preparation until the medial and lateral dye markings are visible. Then the full thickness permanent mattress sutures are placed through the cartilage and perichondrium, meticulously avoiding the skin on the anterior aspect of the ear. By using this technique, the suture tension as well as suture placement allows for individual modulation of the anatomy of each patient 1. If conceal excess is present with a deformity in the upper two thirds of the ear, the Furnas technique may be chosen. This cartilage sparing technique places conchomastoidal sutures from the ear cartilage capturing the anterior perichondrium to the mastoid periosteum. Therefore it is necessary to remove some of the overlying mastoid fascia. Attention must be paid to branches of the greater auricular nerve. Excess skin on the dorsal aspect of the ear, may be excised with an elliptical shape. Regarding the cartilage invasive procedures, the cartilage scoring described by Stenström and cartilage incision by Converse remain the groundwork of our technique. (Figure 4-6)
Figure 4
Figure 5
Figure 6
The Stenström technique relies on cartilage weakening and recovery in a modified anatomic position. Operative goal remains the antihelical fold plication to reduce the mastoid-helical distance which is considered to be ideal when measuring 17mm in the middle. The surgical approach starts with a vertical ellipse skin excision of about 6mm x 4cm on the dorsal side of the antihelix. Then the layer between the cartilage and perichondrium is bluntly dissected and a tunnel to the anterior aspect of the ear is created. Care needs to be taken to create the tunnel wide enough to pass through a rasp for the cartilage weakening without damaging the skin. After anterior vertical scoring, cartilage fragments have to be flushed out. Except for the skin sutures, the Stenstöm technique remains a sutureless procedure with an external dressing modulating the antihelical plication for one to two weeks postoperative. In various cases, the skin sutures may be extended into the mastoid periosteum to reduce tension from the external dressing. Another basic cartilage invasive procedure is the Converse technique 3. During preoperative examination, thumb pressure to the scaphal region forms the newly antihelical fold and superior crus. This simple method also proposes the skin area on the dorsal side that later needs to be resected to prevent skin plication. Surgery starts by an ellipse skin and subcutaneous tissue excision, exposing the perichondrium. The centerline of this ellipse is previously marked by inked needles passed through the body of the new antihelical fold. Further needles may be passed through the margin of the ellipse to mark the area of cartilage excision on the dorsal side. Then three vertical wedge-shaped excisions are made on the medial and lateral border, as well as in the center line of the ellipse. It is important to leave a few millimeters between the excisions to not cause an instability and preserve blood supply. The body of the antihelical fold may vary in size and electrical brush thinning may be necessary prior excision. When the cartilage stripes are removed, the ear is folded by gentle pressure to the scaphal region and permanent sutures are placed below and above the junction of the crura of the antihelix. After the procedure, a pressure dressing is applied for seven days to hold the non-anatomic position and take tension of the sutures.
If the concha mastoid angle is <50°, or a slight asymmetries are noticed after performing surgery of any kind, an additional ear rotation might help to reach the desired auricular shape. Care needs to be taken on the auditory canal and its opening. In case of a narrow anatomy, extensive ear rotation might lead to occlusion and uni- or bilateral hearing loss. The slow or non-absorbant sutures are usually fixed from the dorsal conchal are to the back of the auditory canal. Blunt dissection of the dorsal skin is necessary up to the tip of the ear to reach full flexibility.
If the concha mastoid angle is <50°, or a slight asymmetries are noticed after performing surgery of any kind, an additional ear rotation might help to reach the desired auricular shape. Care needs to be taken on the auditory canal and its opening. In case of a narrow anatomy, extensive ear rotation might lead to occlusion and uni- or bilateral hearing loss. The slow or non-absorbant sutures are usually fixed from the dorsal conchal are to the back of the auditory canal. Blunt dissection of the dorsal skin is necessary up to the tip of the ear to reach full flexibility.
Cartilage invasive
Stenström 26
Skin excision, anterior cartilage weakening with rasp
Converse 3
Cartilage excision combined with suture technique
Cartilage sparing
Mustardé 1
Furnas 10
Furnas 10
Mattress suturing technique
Conchamastoid suture
Conchamastoid suture
Non-invasive
10
Glue, splinting, taping
05
Decision Making
Once a proper indication has been ascertained, the initial preoperative assessment should include the anatomic circumstances. This eventually leads to assigning the surgical goal and the operative procedure. In case of a complex anatomy or individual desires, techniques may be combined at a last stage.
Decision Making Flow Chart
06
Tipps and Tricks
Tips and tricks
Depending on the clinical picture, the surgical intervention and surgical steps must be planned. In order to achieve optimal esthetic results, the surgical procedure must create a new antihelical fold and reduce the mastoid helical distance. By solely focusing on a single technique, ear reduction may be insufficient at some point and overcorrection or instability may be the result. We therefore rarely use a single technique but combine cartilage sparing and invasive procedures. Usually a triangular cartilage resection in the middle of the new antihelical fold is our basic concept. The top of the antihelix is the most fragile and susceptible to cartilage resection. To avoid a floppy, instable ear, we prefer to use the electric brush for scoring rather than doing an excision with the scalpel. If insufficient, additional mattress sutures are set for final correction of the top. In cases of a mastoid-helical angle >50°, an additional cavum reduction is preferred over an ear rotation as extensive rotation narrows the auditory canal. For the cavum reduction, we excise a triangular cartilage stripe of about 2mmx 4 cm and use slow absorbent epichondral sutures for additional stabilization. In case of ear rotation, care must be taken to fully release the chondral attachment to the mastoid.
Tipp 1: Less is more: consider scoring instead of cartilage excision especially at the top to prevent instability
Tipp 2: Combine techniques, use additional sutures if cartilage resection seems insufficient
Tipp 3: Prefer cavum reduction over ear rotation if mastoid-helical angle is >50°
Common complications and how to treat them
Hematoma: conservative, if large consider puncture or reoperation as it may lead to necrosis
Instability: consider reoperation
07
Conclusion and Case Report
Case report
5-year-old male patient with bilateral mastoid-helical angle >50°:
Creation of anti helix
Cavum reduction
No ear rotation
Consider scoring at the top
Figure 1
Postoperative Results
Figure 2
Conclusion
Various operative procedures have been described to treat the prominent ear deformity Cartilage sparing and cartilage invasive techniques are available to recreate the antihelical fold. In our experience, several techniques may be combined to achieve the optimal esthetic result. For the top auf ear, we prefer scoring over cartilage excision to avoid instability and suturing for additional correction. In cases of a mastoid-helical angle is >50°, cavum reduction often is necessary and should be preferred over ear rotation.
08
Video
https://youtu.be/tlmns7MPUwI
Videos
Otoplasty
References
[1]
Otoplasty techniques, Adamson PA, Strecker HD, Facial Plast Surg, 1995
[2]
THE GROWTH PATTERN OF THE EXTERNAL EAR, ADAMSON JKROME E., HORTOX CHARLES E., CRAWFORD HUGH H., Ovid Technologies (Wolters Kluwer Health), 1965
[3]
Technical refinement of Stenström otoplasty procedure, Hafiz R., Philandrianos C., Casanova D., Chossegros C., Bertrand B., Elsevier BV, 2016
[4]
Essentials of Plastic Surgery, Second edition , Jeffrey E. Janis, CRC Press, Taylor and Francis Group, LLC, 2014
[5]
The correction of prominent ears using simple mattress sutures, Mustardé J.C., Elsevier BV, 1963
[6]
Technical refinement of Stenström otoplasty procedure, Hafiz R., Philandrianos C., Casanova D., Chossegros C., Bertrand B., Elsevier BV, 2016
[7]
The Stenstrom otoplasty, Stenstrom SJ, Heftner J, Clin Plast Surg, 1978
[8]
TECHNICAL DETAILS IN THE SURGICAL CORRECTION OF THE LOP EAR DEFORMITY, CONVERSE JOHN MARQUIS, WOOD-SMITH DONALD, Ovid Technologies (Wolters Kluwer Health), 1963
[9]
The correction of prominent ears using simple mattress sutures, Mustardé J.C., Elsevier BV, 1963
[10]
Essentials of Plastic Surgery, Second edition , Jeffrey E. Janis, CRC Press, Taylor and Francis Group, LLC, 2014
[11]
Essentials of Plastic Surgery, Second edition , Jeffrey E. Janis, CRC Press, Taylor and Francis Group, LLC, 2014