["7e2a2f2b3b32a29179d959013e1a74ab0cb7f604","d47466d1294abb83933ea7ddb79b56d460b55e40","77ac1e3bfb9a8a4fe530e65c44c6f84df5ea6347"]
Minimally Invasive Facial Rejuvenation
facial aging
facial rejuvenation
laser therapy
botulinum toxin
soft tissue fillers
3468
3468
Chapter reads
0
0
Chapter likes
6/10
Evidence score
12
12
Images included
02
2
Videos included
01
Introduction
Introduction
The face undergoes numerous changes over the years, many of them are unwelcome and unwanted.
The appearance of fine lines and wrinkles due to repeated facial movements are often just the beginning of the natural aging process. Volume loss and shift are another significant problem that can contribute to skin sagging.
These changes are caused by skin atrophy, increased soft tissue organization, shrinkage and displacement of fat deposits, and a loss of facial bone mass.
Various treatment options are available depending on the findings and desired treatment goal.
The external appearance can be restored, for example, through the use of laser therapy, botulinum toxin and soft tissue fillers - thus turning back time a bit.
The appearance of fine lines and wrinkles due to repeated facial movements are often just the beginning of the natural aging process. Volume loss and shift are another significant problem that can contribute to skin sagging.
These changes are caused by skin atrophy, increased soft tissue organization, shrinkage and displacement of fat deposits, and a loss of facial bone mass.
Various treatment options are available depending on the findings and desired treatment goal.
The external appearance can be restored, for example, through the use of laser therapy, botulinum toxin and soft tissue fillers - thus turning back time a bit.
Definition
Facial aging is a complex biological process of skin, soft tissue, muscle and bone changes starting between the 3rd and 4th decade of life and resulting in: dyspigmentation, loss of volume, tissue laxity, volume displacement as well as static and dynamic rhytids

Signs of Facial Aging
Etiology
There are intrinsic and extrinsic factors causing facial aging:
Intrinsic factors: activity of mimic muscles, genetic or hormonal influences
Extrinsic factors: UV radiation (excessive sun exposure), chemical/ thermal/ mechanical stress/injuries, nutrition, alcohol, nicotine, psychological stress
Pathophysiology
Skin aging is a complex process resulting in a decrease of injury response, barrier function, chemical clearance, sensory perception, immune response, thermoregulation, vascular reactivity, sweat production and vitamin D production.
Epidermis:
Physiologic Aging: decrease in the organization of the stratum corneum, the height of the dermal-epidermal transition, the keratinocyte layers, the number of melanocytes and Langerhans cells, and mitotic activity
Photoaging: atrophy, loss of vertical polarity, thickening of the basal membrane, pigmentary mottling
Physiologic Aging: decrease in the organization of the stratum corneum, the height of the dermal-epidermal transition, the keratinocyte layers, the number of melanocytes and Langerhans cells, and mitotic activity
Photoaging: atrophy, loss of vertical polarity, thickening of the basal membrane, pigmentary mottling
Dermis:
Physiologic Aging: skin atrophy, decrease in the number of fibroblasts, Pacini and Meißner corpuscles, blood vessels, mitotic activity, elastic fibers, occurrence of collagen type I and increase in the occurrence of collagen type III
Photoaging: dermoelastosis, increased basic substance
Physiologic Aging: skin atrophy, decrease in the number of fibroblasts, Pacini and Meißner corpuscles, blood vessels, mitotic activity, elastic fibers, occurrence of collagen type I and increase in the occurrence of collagen type III
Photoaging: dermoelastosis, increased basic substance

Aging Skin Anatomy
Medical History
Age, gender
Comorbidities: wound healing/ scarring disorder
immunodeficiency, neuromuscular disorder (ALS, myasthenia gravis, Lambert-Eaton-syndrome), collagen vascular disease, immunologic skin condition (vitiligo)
immunodeficiency, neuromuscular disorder (ALS, myasthenia gravis, Lambert-Eaton-syndrome), collagen vascular disease, immunologic skin condition (vitiligo)
Medication: antiplatelet/ anticoagulation,
antineoplastic agents, antiinflammatory agents, antibiotics (aminoglycosides), retinoids (past 12 months), steroids
antineoplastic agents, antiinflammatory agents, antibiotics (aminoglycosides), retinoids (past 12 months), steroids
Allergies
Others: smoking, pregnancy/lactation, solarium use (past 6 months), tattoos
Prior treatments & effects
Prior surgery
Patients` preferences
Facial Analysis
Skin type (Fitzpatrick Classification)
Skin texture: normal, dry, oily, mixed, aged, sensitive
Dyspigmentation: hypopigmentation, hyperpigmentation, freckles, solar lentigines, nevi, dysplastic nevi
Vascular lesions: (spider) angiomas, rosacea, teleangiectasias
Scarring and skin lesions: acne scars, surgical scars, traumatic scar, xanthelasmas,syringomas, dermatofibroma, seborrheic keratosis, actinic keratosis, suspicious lesion
Region of facial rhytids: forehead, glabellar complex, nasal region, lateral periorbital region, perioral region, marionette lines, chin, neck
Severity of facial rhytids: superficial rhytids on animation only (dynamic), deep rhytids on animation only (dynamic), superficial rhytids at rest, deep on animation (static), deep rhytids at rest, deeper on animation (static)
Volume: deep (periorbital) upper sulcus, (lateral periorbital lines,) tear through deformity, malar volume loss, nasolabial fold, lower lid-cheek junction, lateral perioral lines, upper lip lines, philtral columns, vermilion, lips, labiomental groove, perimental hollows, chin dimpling, nasal contouring, scar filling
Fitzpatrick Skin Type Classification
Skin type
Characteristics
Tanning ability
I
Pale skin, blue/green eyes, blond/red hair
Always burns, does not tan
II
Fair skin, blue eyes
Burns easily, tans poorly
III
Darker white skin
Tans after initial burn
IV
Light brown skin
Burns minimally, tans easily
V
Brown skin
Rarely burns, tans darkly easily
VI
Dark brown or black skin
Never burns, always tans darkly
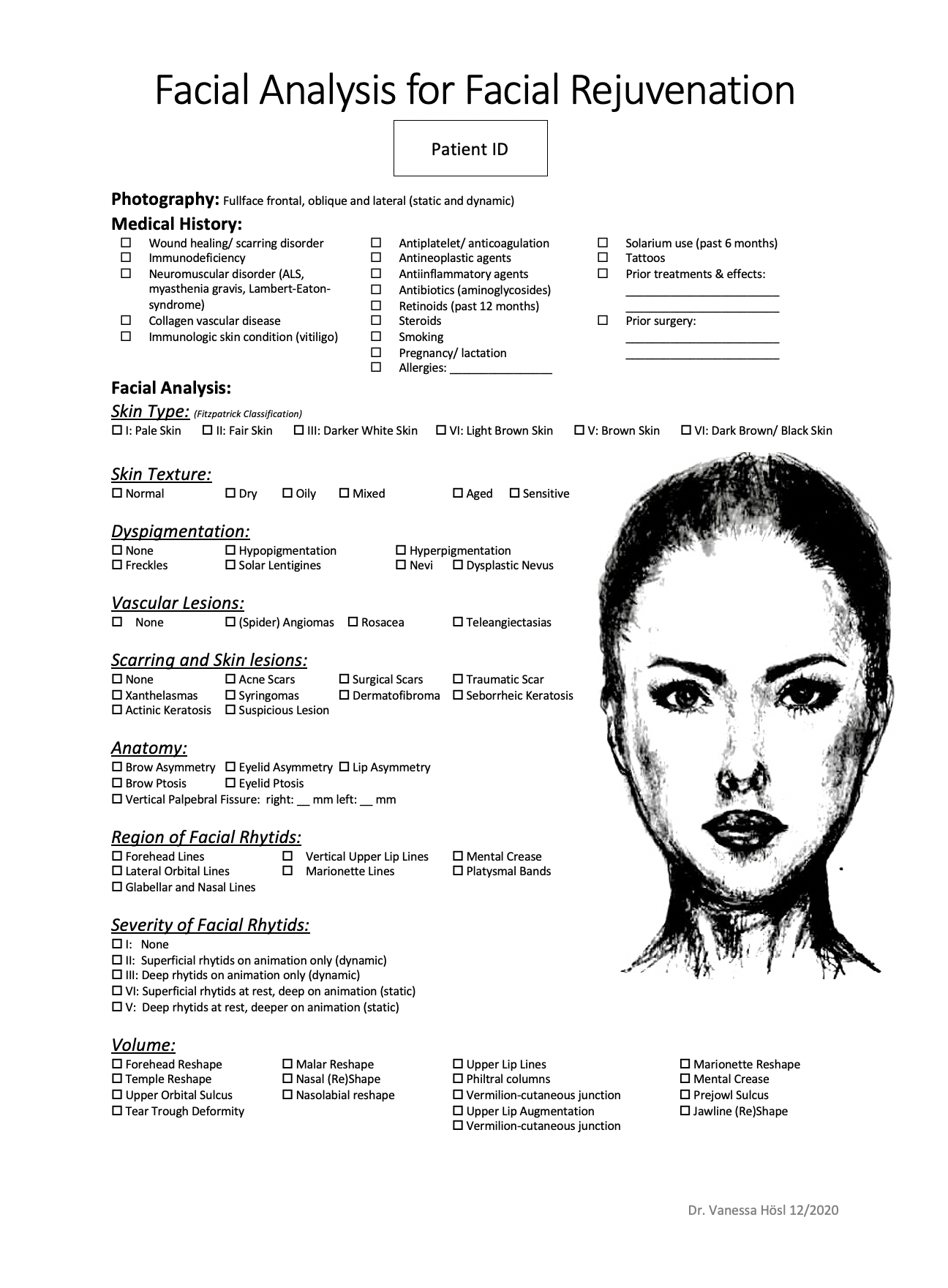
Facial Analysis for Facial Rejuvenation
02
Classification
Classification
Glogau Photoaging Scale
Grade
Description
Characteristics
I
Wrinkles not or only minimally present
(age 28-35)
(age 28-35)
Early Photoaging: Mild pigment changes, no keratosis, minimal wrinkles
II
Wrinkles present only when the skin is in motion
(age 35-50)
(age 35-50)
Early to Moderate Photoaging: Early brown spots visible, keratosis palpable but not visible, parallel smile lines begin to appear
III
Wrinkles present when the skin is at rest (age 50-65)
Advanced Photoaging: Obvious discolorations, visible capillaries (telangiectasias), visible keratosis
IV
Only wrinkles
(age 60-75)
(age 60-75)
Severe Photoaging: Yellow-gray skin color, prior skin malignancies, wrinkles throughout—no normal skin
Severity of Facial Rhytids
Grade
Characteristics
I
No rhytids at rest or on animation
II
Superficial rhytids on animation only
III
Deep rhytids on animation only
IV
Superficial rhytids at rest, deep on animation
V
Deep rhytids at rest, deeper on animation
03
Laser Therapy
Laser Therapy
LASER is an acronym for Light Amplification by Stimulated Emission of Radiation
Lasers produce heat in the target tissue that rapidly dissipates by conduction depending on wavelength, pulse duration, pulse width, spot size and beam shape
Thermal effects induce collagen remodeling which results in tightening of the skin
A suitable wavelength must be selected to target a specific chromophore in the skin
There are mainly two types of lasers for facial rejuvenation:
Ablative lasers vaporize the epidermis and parts of the dermis causing an open wound with a higher risk of scarring and pigmentation changes than nonablative lasers. They also cause thermal damage in the dermis stimulating collagen formation
Nonablative lasers spare the epidermis and cause thermal damage in the dermis stimulating collagen formation only
Ablative Laser
Ablative lasers vaporize the epidermis and parts of the dermis also causing thermal damage (with each pass, the effect of ablation decreases and thermal damage increases)
Ablative lasers leave an open wound
Ablative lasers are more effective for facial rejuvenation than nonablative lasers
The most frequently used ablative lasers are CO2-lasers and ER:YAG-lasers
Ablative Carbon Dioxide Laser (CO2-Laser)
Indication: facial rhytids, scars, benign skin lesions
Wavelength: 10 600 nm; target chromophore: water
Creates significant results at the expense of a long recovery time (1-2 weeks)
Ablative Erbium:Yttrium Aluminium Garnet Laser (ER:YAG-Laser)
Indication: facial rhytids, scars, benign skin lesions
Wavelength: 2940 nm; farget chromophore: Water
The ER:YAG-laser is very versatile; depending on the settings it can be very superficial or very aggressive and ablative
Creates variable results with variable recovery times depending on the ablation settings
Ablative Fractional Laser
Fractional lasers are e.g. CO2- or ER:YAG-lasers, which ablate areas not contiguously but in a “pixilated” pattern; they create microthermal zones
Due to the fact, that just a fraction of the skin is treated, the recovery time is low (3-4 days)
Several treatments sessions are necessary
Pretreatment, Prophylaxis & Preparations
Discontinue oral isotretinoin 6-12 months before the treatment
Evaluate antiplatelet and anticoagulation medication
Apply acyclovir 400 mg 1-1-1 or valaciclovir 500 mg 1-0-1 48 hours before the treatment and continue until the reepithelization is completed
Evaluate the application of antibacterial and antifungal prophylaxis
Cleanse and desinfect the patient`s skin properly
Apply metal eye shields for the patient
Anesthesia
The treatment with ablative lasers is more painful than with nonablative lasers
Topical anesthesia: apply e. g. lidocaine and prilocaine cream (EMLA) 30-90 minutes prior laser treatment
Local anesthesia: use e. g. 4% articain hydrochloride with 1:200.000 epinephrine for nerve blocks
Systemic anesthesia
Treatment
Ablative Carbon Dioxide Laser (CO2-Laser)
Use a nonoverlapping treatment pattern and perform two or three passes
Endpoint: yellow-brown discoloration, no further skin contraction, eradication of photodamaged area or rhytid
Ablative Erbium:Yttrium Aluminium Garnet Laser (ER:YAG-Laser)
Use an overlapping treatment pattern
Endpoint: bleeding spots (noncoagulation-mode), exposure of midreticular dermis, eradication of the rhytid
Posttreatment Care
Keep the wounds moistured using either an occlusive dressing for 1-3 days (with frequent changes) and an open wound care afterwards or providing open wound care primarily with application of e. g. dexpanthenol, Synchroline Terproline Egf cream, Cosmelan cream
Apply ice packages to cool the treated areas
Apply appropriate pain medication
Continue acyclovir 400 mg 1-1-1 or valaciclovir 500 mg 1-0-1 48 hours until the reepithelization is completed
Apply antibacterial and antifungal prophylaxis (if necessary)
Recommend sunscreen (at least SPF 30) after reepithelialization
Side effects & Complications
Dyspigmentations, erythema, edema, pruritus, flaking, acne, contact dermatitis, scarring, infections, ectropion
Conclusion
Ablative lasers can cause wounds in variable depths
The more superficial the wound, the shorter the recovery time
The deeper the wound, the better the rejuvenation effect
Several treatment sessions may be necessary
ER:YAG-lasers produce more selective tissue vaporization and less thermal coagulation than CO2-lasers
Due to the increased thermal damage CO2-lasers produce more collagen remodelling (resulting in skin tightening) than ER:YAG-lasers
The endpoints should be clearly understood before starting a laser treatment
Nonablative Laser
Nonablative lasers spare the epidermis and cause thermal damage in the dermis stimulating collagen formation only and leaving the skin surface intact
There is a great variability of nonablative lasers. The most frequently used nonablative lasers are Erbium-doped-fractional-lasers (Fraxel, Solta Medical) to treat dyschromia, fine rhytids and scars
Recovery time after nonablative laser treatment is minimal compared to an ablative laser treatment
Even if several sessions are performed, the results are very variable
04
Botulinum Toxin
Botulinum Toxin
Botulinum toxin is a neurotoxin produced by Clostridium botulinum, a gram-positive anaerobic bacterium
Botulinum toxin inhibits the synaptic transmission at the neuromuscular junction irreversibly targeting the SNAP/SNARE complex and inhibiting acetylcholine release
There are eight types of botulinum toxin, two types (type A and type B) are FDA approved for clinical use.
There are substances of different manufacturers. It should be noted that the injection units differ from manufacturer to manufacturer.
In the following, the injection units of OnabotulinumtoxinA (Vistabel®, Allergan) are shown.
It is available in 50- or 100-unit-vials, the final dilution is 2.5-4 U/0.1 ml and it is stored at 2°-8° C.
In the following, the injection units of OnabotulinumtoxinA (Vistabel®, Allergan) are shown.
It is available in 50- or 100-unit-vials, the final dilution is 2.5-4 U/0.1 ml and it is stored at 2°-8° C.
Treatment
Indication: dynamic lines, folds and furrows
Preparation:
The dose must be individualized (severity, muscle bulk, type of botulinum toxin, previous treatments)
Botulinum toxin powder is reconstituted with 0,9% sterile saline solution
Cleanse and desinfect the patient`s skin properly
Injection tools: 1 ml syringes, 30-/ 32-gauge needles
Anesthesia: possibly topical
Side effects/ complications: allergic reaction, injection site pain, bleeding, bruising, headache, brow/ eyelid ptosis, facial asymmetry, nausea, dysphagia, respiratory compromise, infection, acne
Contraindications: skin infection, allergy/ hypersensitivity to ingredients e.g. albumin (Botox®, Dysport®, Xeomin®) or lactose (Dysport®)
Use with caution: myasthenia gravis, Lambert-Eaton syndrome, coadministration of aminoglycoside antibiotics, inflammatory skin disorder, pregnancy, lactation
Use with caution: myasthenia gravis, Lambert-Eaton syndrome, coadministration of aminoglycoside antibiotics, inflammatory skin disorder, pregnancy, lactation
Posttreatment care: no massage of treated area, cold packs, limited activity for 1 d, next visit 2 weeks after application
Effect: 1-4 days after application
Longevity: 3-6 months
Forehead Lines
Goal: m. frontalis
Technique:
5-10 injection points
Inject 2 cm above the eyebrows to prevent brow ptosis
Inject even higher laterally to prevent drooping of lateral brow
Consider brow position (horizontal in men, arched in women)
Avoid complete paralysis (to prevent brow ptosis)
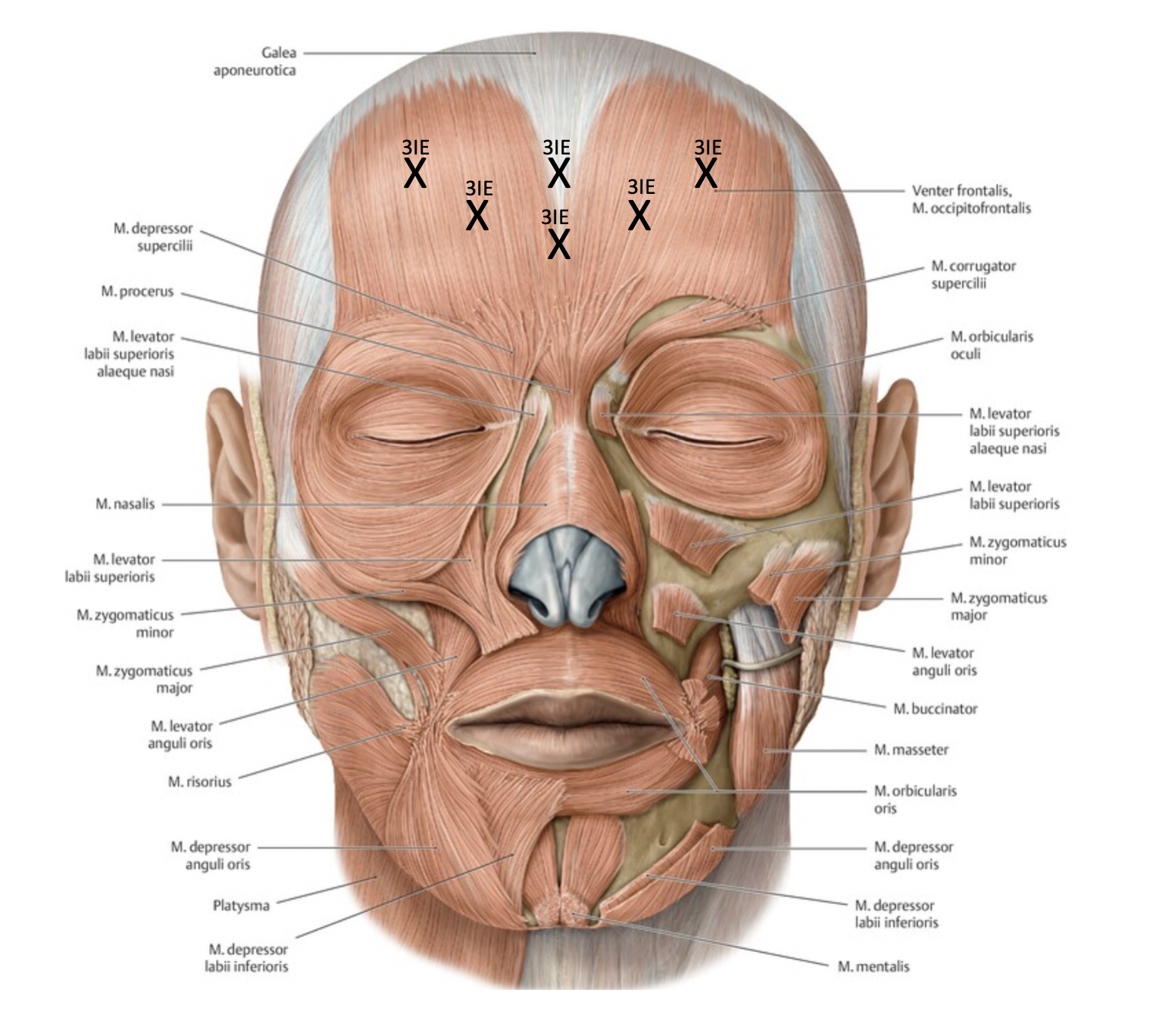
Forehead Lines
Glabellar and Nasal Lines (Bunny Lines)
Goal: m. corrugator supercilii, m. depressor supercilii, m. procerus, m. nasalis
Technique:
5-11 injection points
Inject only above orbital rim (to prevent eyelid ptosis)
Inject through the eyebrow (a hematoma remains hidden)
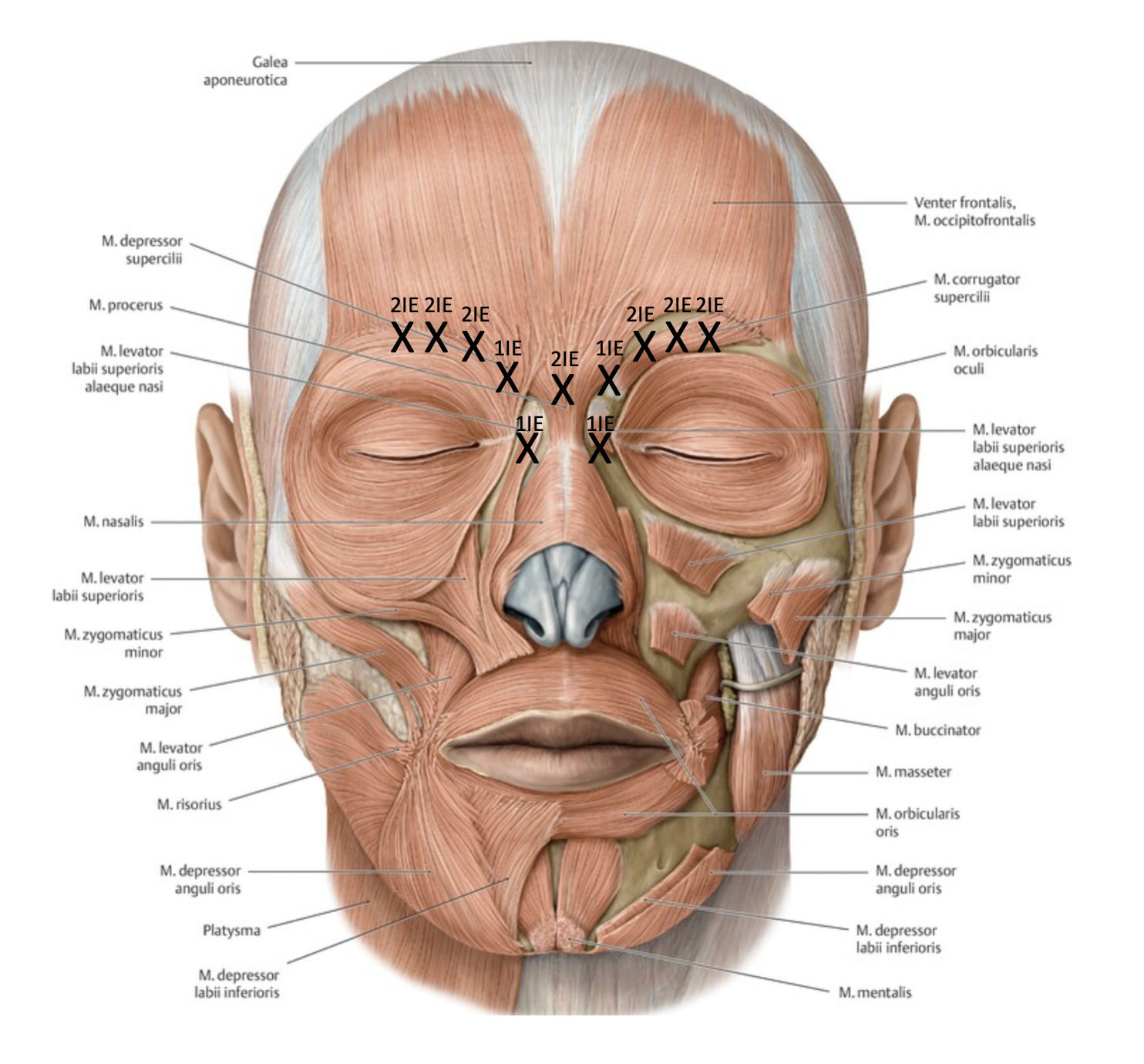
Glabellar Lines and Nasal Lines (Bunny Lines)
Lateral Orbital Lines (Crow's feet)
Goal: m. orbicularis oculi
Technique:
6-12 injection points
Inject superficially
Do not inject below zygomatic arch (to prevent injections in M. zygomaticus major)
Consider lower lid laxity (to prevent postinjective scleral show, lower lid retraction)
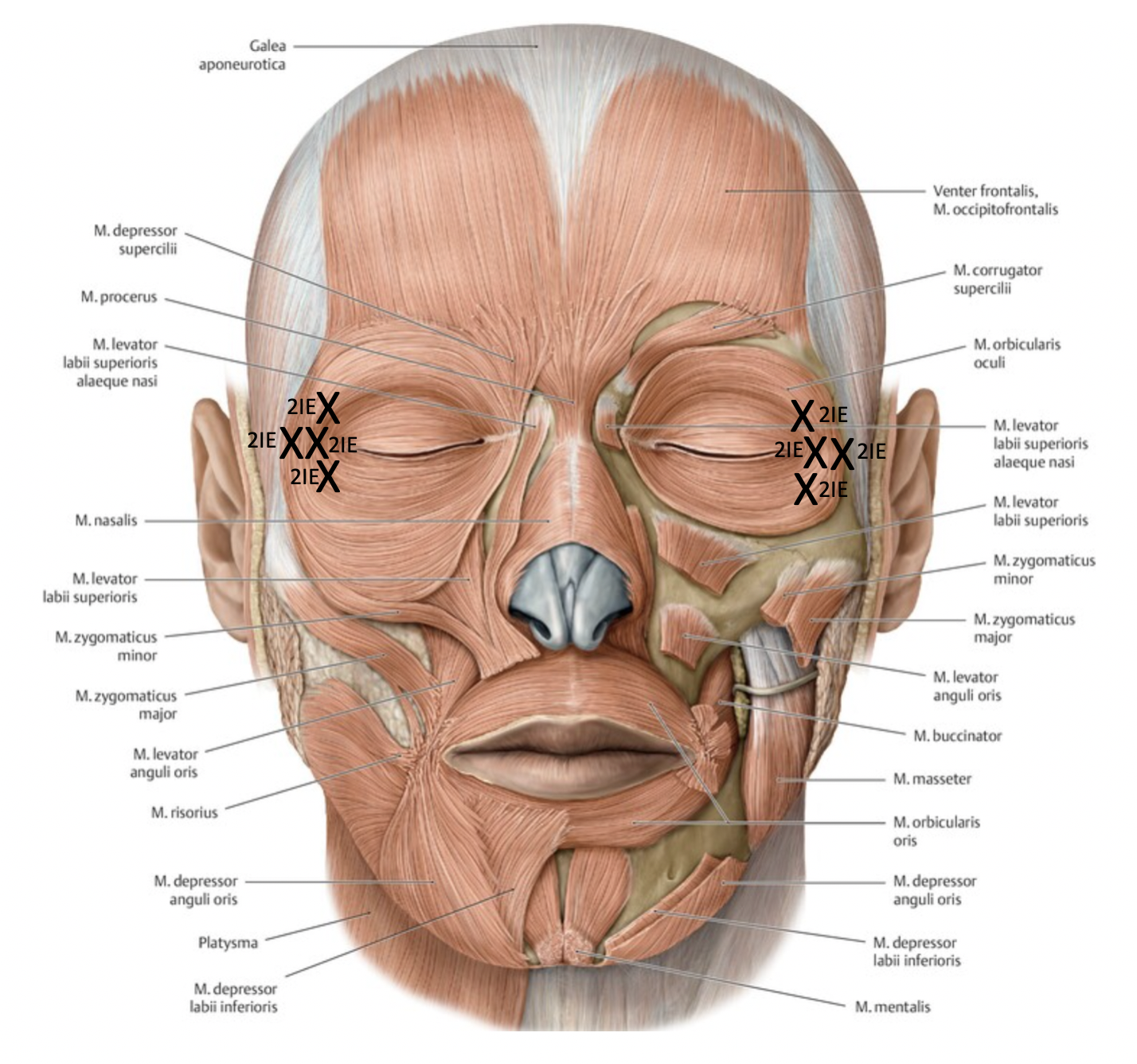
Lateral Orbital Lines (Crow's feet)
Vertical Upper Lip Lines
Goal: m. orbicularis oris
Technique:
2-4 injection points
Inject superficially
Inject within 5 mm of the vermilion border
Inexperienced injectors should avoid the lower lip
Possibly use local anesthetics
Be especially careful with patients, who have speaking confessions
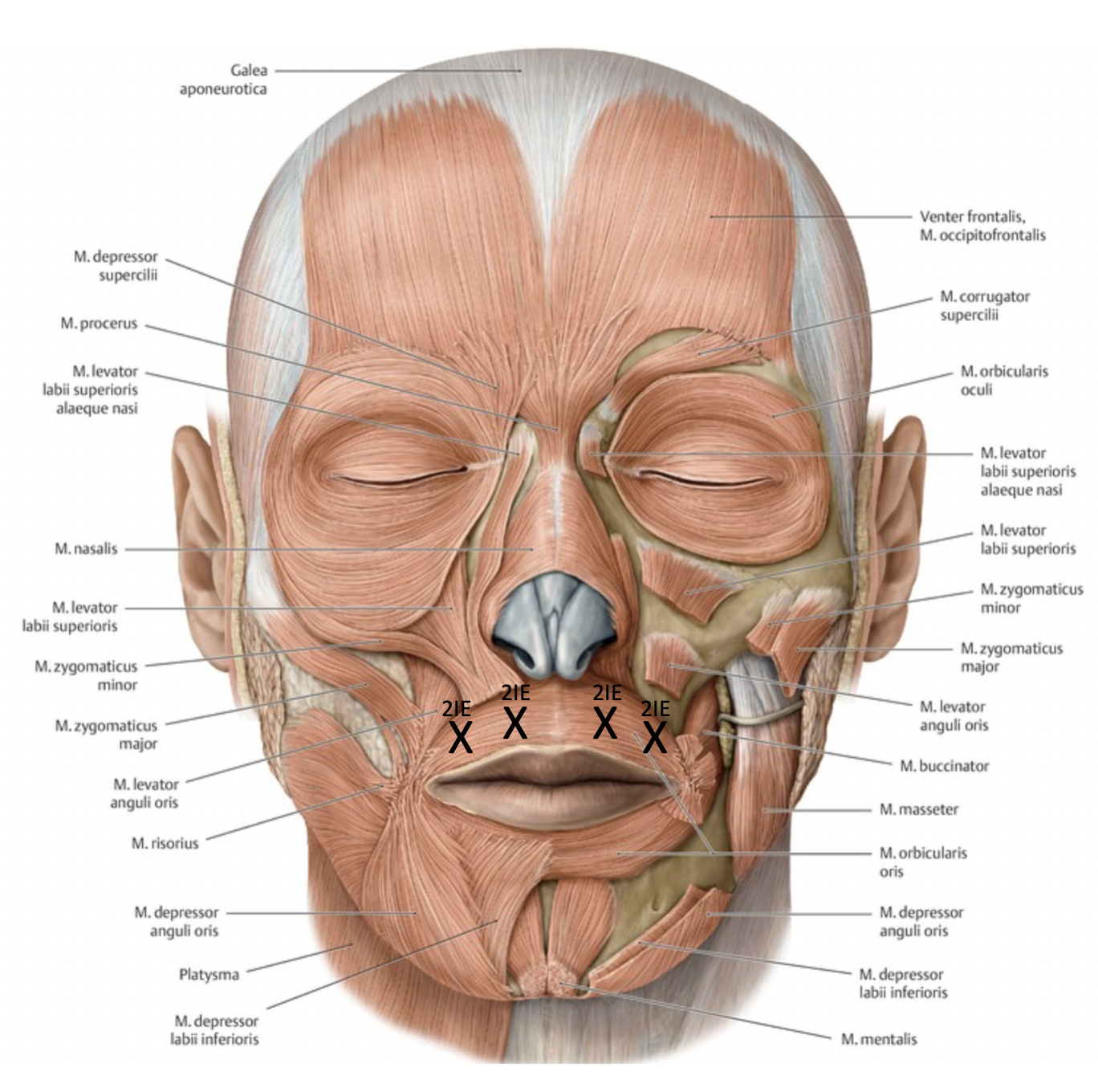
Vertical Upper Lip Lines
Marionette Lines (Bitterness Fold)
Goal: m. depressor anguli oris
Technique:
2-4 injection points
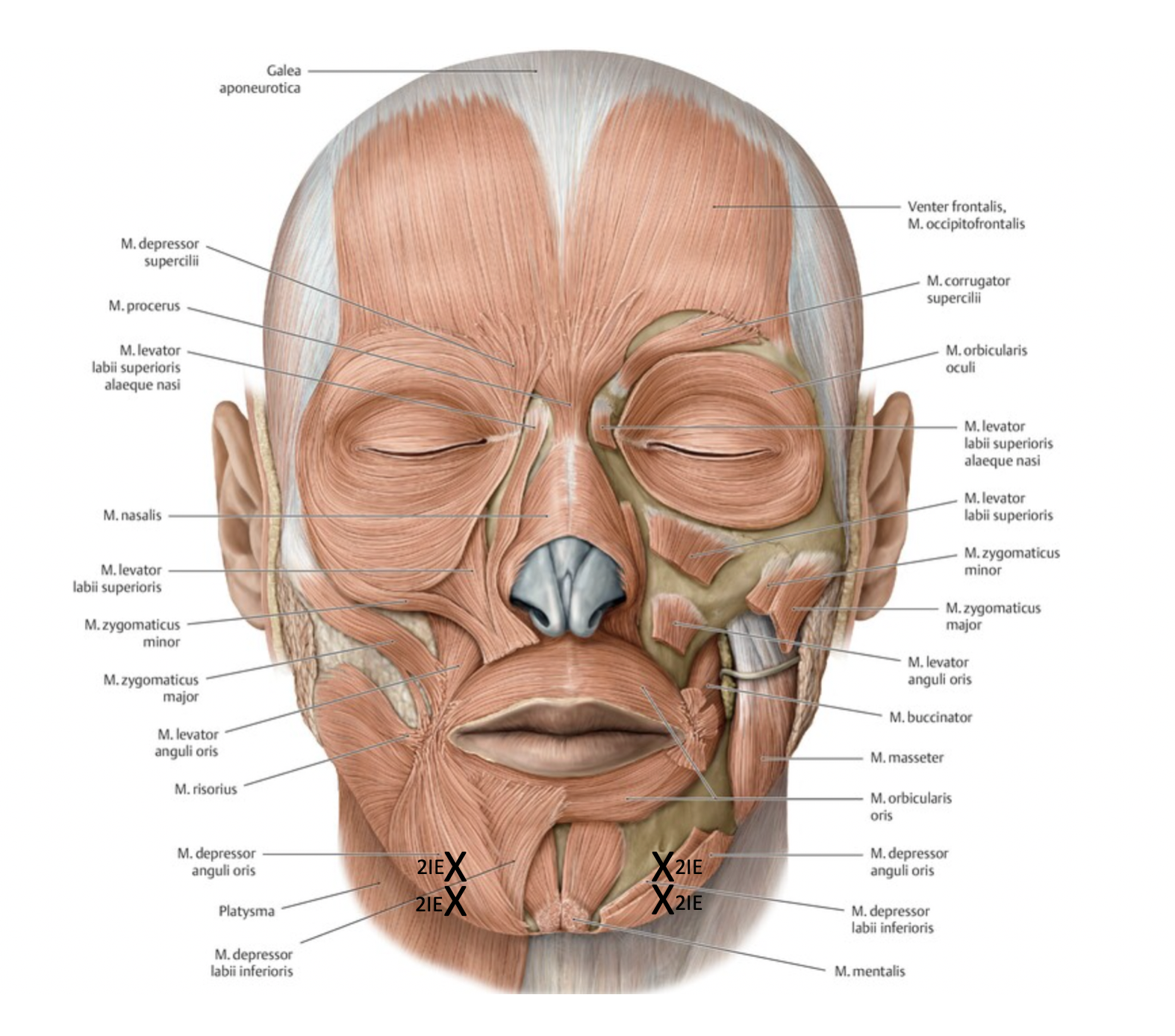
Marionette Lines (Bitterness Fold)
Mental Crease
Goal: m. mentalis
Technique:
2-4 injection points
Inject with needle angled superiorly
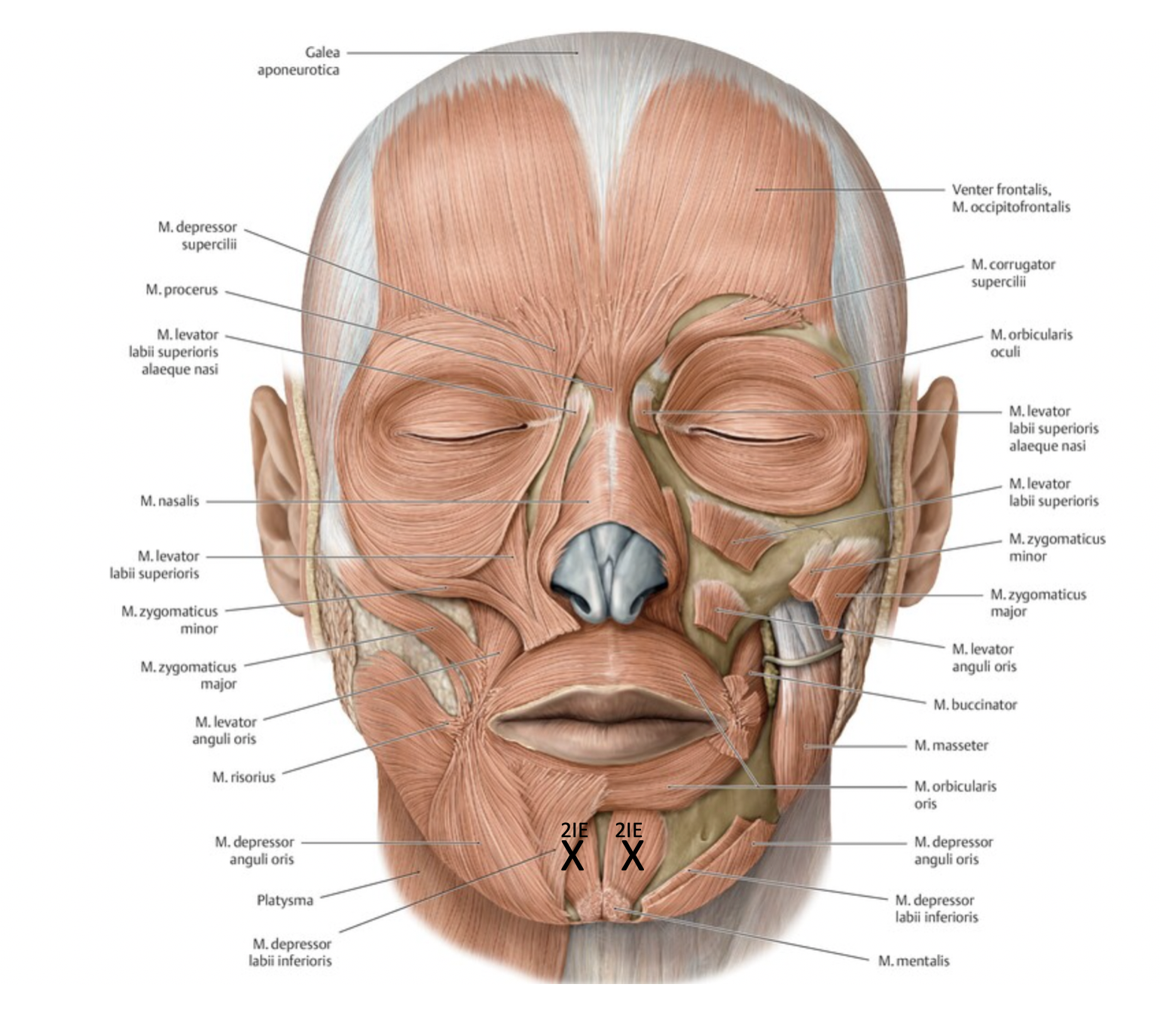
Mental Crease
Platysmal Bands
Goal: platysma
Technique:
3-6 injection points (per band) á 2IE
Treat only patients with preserved skin elasticity and paucity of submental fat
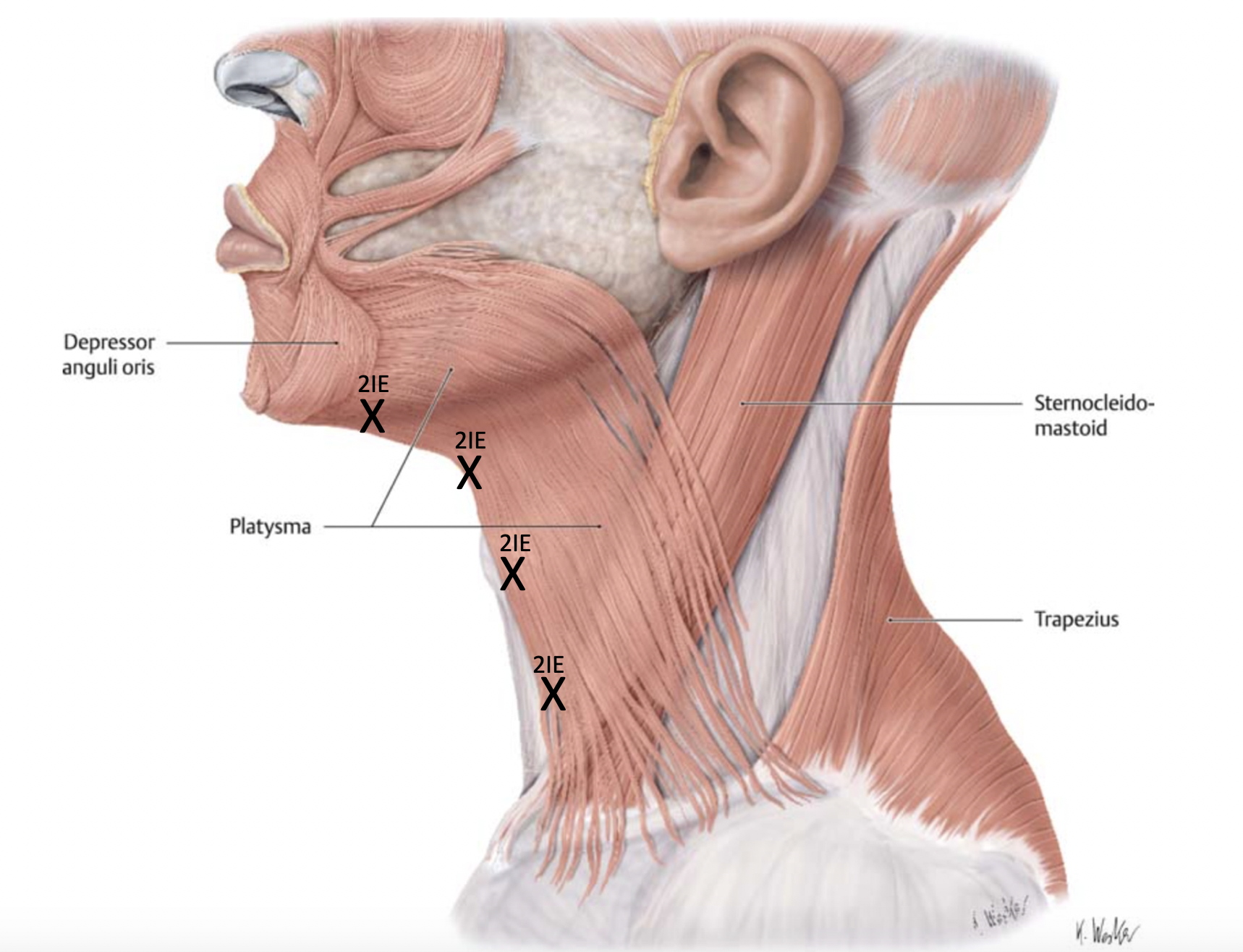
Platysmal Bands
The Face Recurve® Concept
Face Recurve® is a concept developed by Le Louarn, Buthiau and Buis to counteract the cutaneous and structural aging of the face in a preventive and curative way.The Face Recurve® concept is based on studies which have shown that certain parts of certain mimic muscles (so-called Age Marker Fascicles) lead to an increased redistribution of deep fat deposits towards the surface through their contraction (facial expression). The ability of the mimic muscles to relax completely also decreases with increasing age. This leads, for example, to the formation of glabellar fold, tear trough, naso-labial fold, bitterness fold and cervical bands.To counteract this process, partial chemical denervation is performed first, followed by combined application with tissue fillers. In the case of progressive aging, surgical separation of the Age Marker Fascicles is performed, if necessary in combination with further tightening interventions.
Conclusion
Botulinum toxin inhibits the synaptic transmission at the neuromuscular junction irreversibly
There are substances of different manufacturers. Note that the injection units differ between the manufacturers
Knowledge of anatomic structures is fundamental
Facial analysis is required before every treatment
Consider asymmetries and pretreatment brow/ lid ptosis
Create a harmonic appearance of the whole face
Avoid complete paralysis
Overtreatment should be avoided due to the non-antagonizable effect of botulinum toxin
Effect occurs 1-4 days after application
Repeat treatment after 3-6 months
05
Soft Tissue Fillers
Soft Tissue Fillers
The ideal soft tissue filler has not been created yet.
Currently available fillers are compromises aiming for the following characteristics:
Currently available fillers are compromises aiming for the following characteristics:
biocompatible
no side effects causing
nonpalpable
ready to use
easy to applicate
potentially reversible
minimal downtime
Nonautologous Biologic Soft Tissue Fillers
Hyaluronic Acid (HA)
Glycosaminoglycan biopolymer of disaccarids
Physiologic, hydrophilic component of the skin restoring dermal hydration as well as improving skin structure and elasticity
Mostly nonanimal based
Expands after injection while absorbing water
Available in different viscosities (form stability), with different crosslinking (longevity) and also with lidocaine
Effect: Immediately
Longevity: 4-12 months depending on crosslinking of HAs
Reversal correction: use hyaluronidase to treat irregularities or solve perfusion problems
Synthetic Soft Tissue Fillers
Calcium Hydroxyapatite (Radiesse, Merz)
Calcium hydroxyapatite microspheres suspended in aquaous gel
Biodegradable in calcium and phosphate ions
Gel is replaced by collagen
Not easy to mold
Used to treat medium-to-deep creases
Avoid perioral/ periorbital region (do not apply to superficial)
Effect: immediately
Longevity: 9-12 months
Poly-L-Lactic Acid (PLLA, Sculptra, Valeant Aesthetics)
PLLA is metabolized to carbondioxide or glucose and replaced by collagen
The initial effect results from inflammatory processes
Biodegradable, very viscous
Reconstitute at least three hours before injections (better overnight)
Used to treat medium-to-deep rhytids
Avoid perioral/ periorbital region (do not apply to superficial)
Effect: after 8-12 weeks
Longevity: 18-24 months
Polymethylmethacrylate (PMMA, Artefill, Suneva Medical)
PMMA beads are covered with bovine collagen
The collagen is resorbed and replaced by connective tissue
Needs skin testing prior to use
Used to treat medium-to-deep rhytids
Avoid perioral/ periorbital region (do not apply to superficial)
There are several treatments necessary to create volume
Effect: 6-8 weeks after application
Longevity: (semi-)permanent
Reversal correction: use triamcinolone to treat irregularities
Autologous Biologic Soft Tissue Fillers –> s. Lipofilling
Treatment
Indication: filling of rhytids (creases, furrows and lines), volume restoration, reshaping
Preparation: choose substance individually (especially depending on area to treat), cleanse and desinfect the patient’s skin properly Injection tools: 1 ml syringes, 25-/27-/30-gauge needles or canulas depending on the filler’s viscosity
Anesthetics: possibly topical or nerve blocks
Side effects/ complications: injection site pain/ discomfort, bleeding, ecchymosis, edema/swelling, allergic reaction/ hypersensitivity, infection, intravasal injection, skin necrosis/ ulcerations, vision loss, irregularities, nodule formation, over-/ undercorrection, asymmetries
Contraindications: allergy to ingredients, collagen (vascular) disease (for some fillers)
Application techniques: serial puncture (droplet technique), linear threading, fanning, cross-radial technique (cross-hatching); aspirate before injection, especially in “danger zones”; the thinner the skin and the more superficial the injection is required, the smaller the molecule size of the filler should be
Dr. Mauricio de Maio's MD Codes help to define the area to treat and how much volume to apply
Posttreatment care: digital molding and massage of the treated area, cold packs, limited facial expression for 48 hours, consider steroids application after great volume injections, limited activity for 1 d
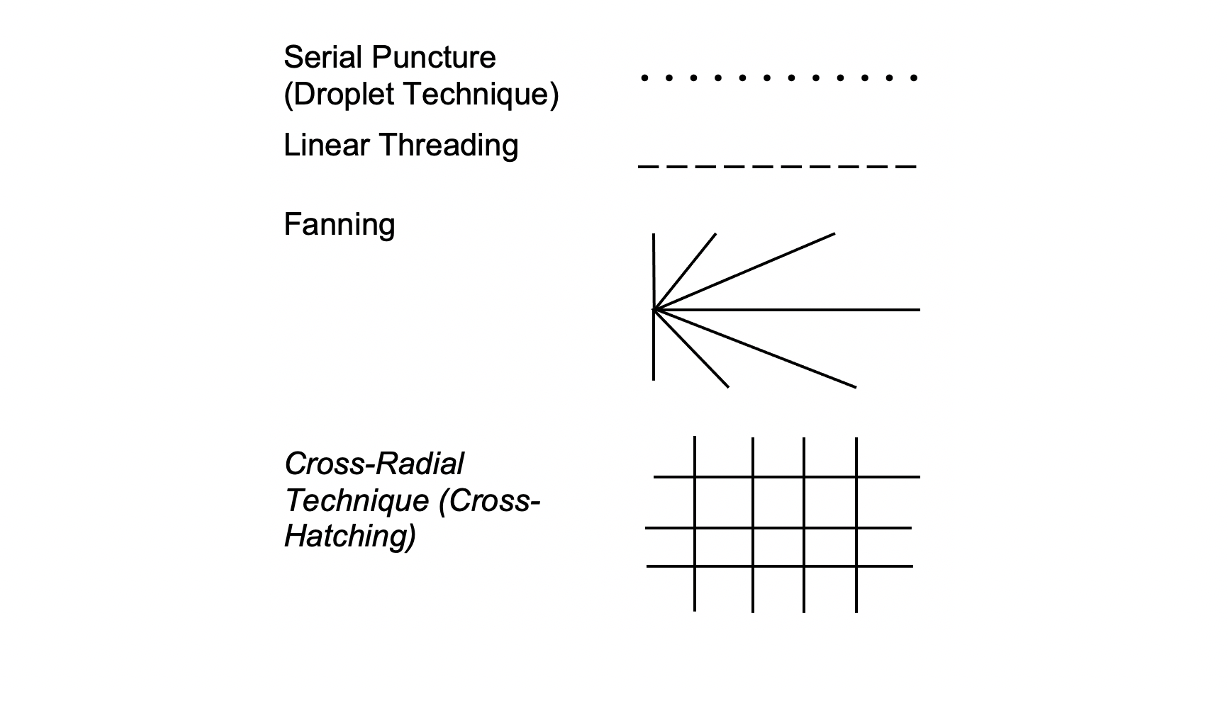
Application Techniques
Upper Face
Forehead reshape: deep injection, serial puncture (several injection points), combinate with botulinumtoxin
Temple reshape: deep injection, serial puncture (few injection points)
Periorbital reshape:
Filling of upper orbital sulcus: deep injection, serial puncture (few injection points)
Filling of tear trough deformity: superficial injection, linear threading
Filling of upper orbital sulcus: deep injection, serial puncture (few injection points)
Filling of tear trough deformity: superficial injection, linear threading
Mid Face
Malar reshape: multilevel injection, fanning or cross-radial
Nasal (re)shape: deep injection, serial puncture (few injection points)
Lower Face
Nasolabial reshape: multilevel injection, fanning or cross-radial, possibly combinate products with different viscosities
Lip reshape:
Filling of upper lip lines: superficial injection, linear threading, combinate with skin resurfacing and/ or botulinumtoxin
Filling of philtral columns: superficial injection, linear threading
Definition of vermilion-cutaneous junction: superficial injection, linear threading
Upper lip augmentation: superficial injection, linear threading
Filling of upper lip lines: superficial injection, linear threading, combinate with skin resurfacing and/ or botulinumtoxin
Filling of philtral columns: superficial injection, linear threading
Definition of vermilion-cutaneous junction: superficial injection, linear threading
Upper lip augmentation: superficial injection, linear threading
Marionette reshape: multilevel injection, fanning or cross-radial, possibly combinate products with different viscosities
Chin reshape:
Filling of mental crease: subcutaneous injection, linear threading, combinate with botulinumtoxin
Filling of prejowl sulcus: subcutaneous injection, fanning
Filling of mental crease: subcutaneous injection, linear threading, combinate with botulinumtoxin
Filling of prejowl sulcus: subcutaneous injection, fanning
Jawline (re)shape: subcutaneous injection, linear threading
Danger Zones
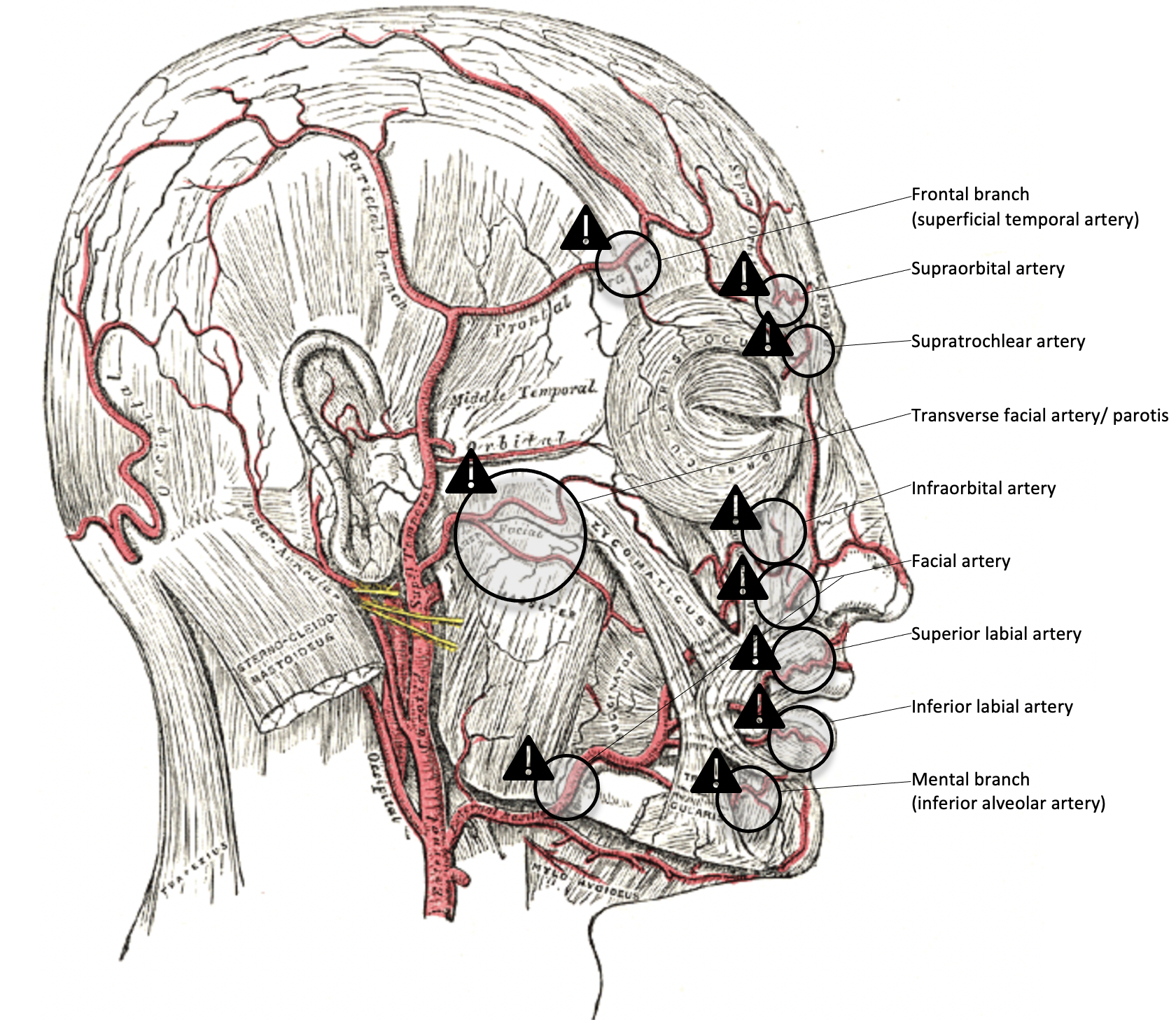
Danger Zones
Conclusion
There is a great variety of fillers with different profiles regarding sensitivity, usability and longevity
The thinner the skin and the more superficial the injection is required, the smaller the molecule size of the filler should be
Consider multilevel filling or the usage of fillers with different viscosities to treat deep rhytids
06
Conclusion
Conclusion
Essential for a successful facial rejuvenation treatment is a solid knowledge of the anatomy of the face
Find out what bothers the patient most (e.g. single lines or "angry"/ "tired" look)
Facial analysis is a very important step to evaluate skin conditions (e.g. thickness, Fitzpatrick type, dyspigmentation) as well as static and dynamic rhytids
Discuss and balance realistic treatment goals also in terms of recovery time
Define the treatment strategy individually by possibly combining laser resurfacing, muscle chemodenervation and application of soft tissue fillers
Dynamic rhytids can be treated well with botulinum toxin
Static rhytids can be treated well with skin resurfacing, soft tissue fillers or surgery
Images
Aging Skin Anatomy
Glabellar Lines and Nasal Lines (Bunny Lines)
Lateral Orbital Lines (Crow's feet)
Forehead Lines
Vertical Upper Lip Lines
Mental Crease
Marionette Lines (Bitterness Fold)
Facial Analysis for Facial Rejuvenation
Platysmal Bands
Signs of Facial Aging
Danger Zones
Application Techniques
References
[1]
Anatomy and pathophysiology of facial aging, Zimbler MS, Kokoska MS, Thomas JR, Facial Plast Surg Clin North Am, 2001
[2]
Numerical modeling of facial aging, Pitanguy I, Pamplona D, Weber HI, Leta F, Salgado F, Radwanski HN, Plast Reconstr Surg, 1998
[3]
Changes in the Facial Skeleton with Aging: Implications and Clinical Applications in Facial Rejuvenation, Mendelson BC, Wong CH, Aesthetic Plast Surg, 2020
[4]
Models of facial aging and implications for treatment, Lambros V, Clin Plast Surg, 2008
[5]
Aging Skin: Histology, Physiology, and Pathology, Khavkin Jeannie, Ellis David A.F., Elsevier BV, 2011
[6]
Update on Facial Aging, Fitzgerald Rebecca, Graivier Miles H., Kane Michael, Lorenc Z. Paul, Vleggaar Danny, Werschler Wm. Philip, Kenkel Jeffrey M., Oxford University Press (OUP), 2010
[7]
The aging face, Ko Audrey C., Korn Bobby S., Kikkawa Don O., Elsevier BV, 2017
[8]
The Anatomy of the Aging Face: A Review, Fratila Alina, Schenck Thilo, Redka-Swoboda Wolfgang, Zilinsky Isaac, Pavicic Tatjana, Cotofana Sebastian, Georg Thieme Verlag KG,
[9]
Aging Skin: Histology, Physiology, and Pathology, Khavkin Jeannie, Ellis David A.F., Elsevier BV, 2011
[10]
Aging in the Male Face, Keaney Terrence C., Ovid Technologies (Wolters Kluwer Health), 2016
[11]
Aging Skin: Histology, Physiology, and Pathology, Khavkin Jeannie, Ellis David A.F., Elsevier BV, 2011
[12]
Update on Facial Aging, Fitzgerald Rebecca, Graivier Miles H., Kane Michael, Lorenc Z. Paul, Vleggaar Danny, Werschler Wm. Philip, Kenkel Jeffrey M., Oxford University Press (OUP), 2010
[13]
Aging in the Male Face, Keaney Terrence C., Ovid Technologies (Wolters Kluwer Health), 2016
[14]
Aging Skin: Histology, Physiology, and Pathology, Khavkin Jeannie, Ellis David A.F., Elsevier BV, 2011
[15]
Update on Facial Aging, Fitzgerald Rebecca, Graivier Miles H., Kane Michael, Lorenc Z. Paul, Vleggaar Danny, Werschler Wm. Philip, Kenkel Jeffrey M., Oxford University Press (OUP), 2010
[16]
The aging face, Ko Audrey C., Korn Bobby S., Kikkawa Don O., Elsevier BV, 2017
[17]
The Anatomy of the Aging Face: A Review, Fratila Alina, Schenck Thilo, Redka-Swoboda Wolfgang, Zilinsky Isaac, Pavicic Tatjana, Cotofana Sebastian, Georg Thieme Verlag KG,
[18]
Models of facial aging and implications for treatment, Lambros V, Clin Plast Surg, 2008
[19]
Changes in the Facial Skeleton with Aging: Implications and Clinical Applications in Facial Rejuvenation, Mendelson BC, Wong CH, Aesthetic Plast Surg, 2020
[20]
Numerical modeling of facial aging, Pitanguy I, Pamplona D, Weber HI, Leta F, Salgado F, Radwanski HN, Plast Reconstr Surg, 1998
[21]
Anatomy and pathophysiology of facial aging, Zimbler MS, Kokoska MS, Thomas JR, Facial Plast Surg Clin North Am, 2001
[22]
The validity and practicality of sun-reactive skin types I through VI, Fitzpatrick T. B., American Medical Association (AMA), 1988
[23]
The validity and practicality of sun-reactive skin types I through VI, Fitzpatrick T. B., American Medical Association (AMA), 1988
[24]
Aesthetic and anatomic analysis of the aging skin, Glogau Richard G., Frontline Medical Communications, Inc., 1996
[25]
Essentials of Aesthetic Surgery, Jeffrey E. Janis, Thieme, 2018
[26]
Lasers for facial rejuvenation, Goldberg DJ, Am J Clin Dermatol, 2003
[27]
Lasers for facial rejuvenation: a review, Papadavid E, Katsambas A, Int J Dermatol, 2003
[28]
Essentials of Aesthetic Surgery, Jeffrey E. Janis, Thieme, 2018
[29]
Botulinum toxin: expanding role in medicine, Rohrich RJ, Janis JE, Fagien S, Stuzin JM, Plast Reconstr Surg, 2003
[30]
The cosmetic use of botulinum toxin, Rohrich RJ, Janis JE, Fagien S, Stuzin JM, Plast Reconstr Surg, 2003
[31]
MD Codes™: A Methodological Approach to Facial Aesthetic Treatment with Injectable Hyaluronic Acid Fillers, de Maio M, Aesthetic Plast Surg, 2020
[32]
Facial rejuvenation and concentric malar lift: the FACE RECURVE concept, Le Louarn C, Buthiau D, Buis J, Ann Chir Plast Esthet, 2006
[33]
Essentials of Aesthetic Surgery, Jeffrey E. Janis, Thieme, 2018
[34]
Injectable soft-tissue fillers: clinical overview, Eppley BL, Dadvand B, Plast Reconstr Surg, 2006
[35]
Soft tissue fillers: an overview, Kinney BM, Hughes CE 3rd, Aesthet Surg J, 2001
[36]
The role of hyaluronic acid fillers (Restylane) in facial cosmetic surgery: review and technical considerations, Rohrich RJ, Ghavami A, Crosby MA, Plast Reconstr Surg, 2007
[37]
Advances in facial rejuvenation: botulinum toxin type a, hyaluronic acid dermal fillers, and combination therapies--consensus recommendations, Carruthers JD, Glogau RG, Blitzer A, Facial Aesthetics Consensus Group Faculty., Plast Reconstr Surg, 2008
[38]
Essentials of Aesthetic Surgery, Jeffrey E. Janis, Thieme, 2018
[39]
Injectable soft-tissue fillers: clinical overview, Eppley BL, Dadvand B, Plast Reconstr Surg, 2006
[40]
Soft tissue fillers: an overview, Kinney BM, Hughes CE 3rd, Aesthet Surg J, 2001
[41]
The role of hyaluronic acid fillers (Restylane) in facial cosmetic surgery: review and technical considerations, Rohrich RJ, Ghavami A, Crosby MA, Plast Reconstr Surg, 2007
[42]
MD Codes™: A Methodological Approach to Facial Aesthetic Treatment with Injectable Hyaluronic Acid Fillers, de Maio M, Aesthetic Plast Surg, 2020