["d47466d1294abb83933ea7ddb79b56d460b55e40","b88bd93f2ab8bc3f1442e3ddc88a5a91b747774e"]
Indications for Breast Reconstruction
breast cancer
breast reconstruction
mastectomy
breast cancer therapy
3167
3167
Chapter reads
0
0
Chapter likes
7/10
Evidence score
09
9
Images included
00
0
Videos included
01
Indications for Breast Reconstruction
Indications
Breast Cancer Diagnosis
Before talking about indications for breast reconstruction, we need to take a step back and have a deeper look in indications for different techniques of oncological breast surgery.
Therefore, we will give an overview of breast cancer treatment in general following the actual S3- guidelines S3 Guideline of German Cancer Society, the MSD Mannual for Breast cancer MSD Mannual the Mannual for Breast Cancer of TU and LMU Munich Mannual for Breast Cancer of TU and LMU Munich 18. Auflage 2021, Tumorzentrum München, ISBN: 978-3-86371-373-7 and the national clinic guideline for Diagnosis, staging and treatment of patients with breast cancer National clinic guideline for Diagnosis, staging and treatment of patients with breast cancer no. 7. 2015.
When diagnosed with breast cancer or it`s precancerous stages (LIN, DCIS) women need to undergo a certain path of diagnostic investigation and clinical examinations. After checking the medical history of the patient, the most important questions are:
1. What does the breast and it`s skin look like? Are there any palpable nodes? The clinical examination consisting of visualizing the patient and her breast especially concerning ulceration, inflammation, retraction of the NAC or skin above the tumor, Peaux d’orange, discharge of the nipple and palpation of both breasts in a certain manner as well as both lymphatic pathways, is essential.
2. What does the tumor look like using mammography and ultrasound? Is there one node or more?
The most important factors are the size and the location of the tumor, the distance to the skin and to the nipple-areola-complex. Furthermore, the axillary lymphatic nodes need to be checked for metastases. In some cases (e.g. higher density of the breast, implants, young patients) an MRI is needed.
3. What kind of breast cancer are we dealing with?
The majority is either from a ductal origin (DCIS/NST) or lobular (LIN/invasive lobular). There are also rare cases of non-epithelial tumors such as angio-/sarcoma or phylloidestumors. Additionally, information about hormone receptor expression, Her2 status, proliferation rate (marker Ki67) and grading (G1-G3) of the tumor is needed. Therefore, we need a histopathological result. A biopsy of the tumor and of suspect lymph nodes is taken under ultrasound or mammographic control.
4. Are there any distant metastases?
In particular we need a CT Thorax/Abdomen to check the liver and lung and a szintigraphy of the skeleton. Cerebral metastases should only be checked via cCT if we have any suspicion concerning cerebral failures
Therefore, we will give an overview of breast cancer treatment in general following the actual S3- guidelines S3 Guideline of German Cancer Society, the MSD Mannual for Breast cancer MSD Mannual the Mannual for Breast Cancer of TU and LMU Munich Mannual for Breast Cancer of TU and LMU Munich 18. Auflage 2021, Tumorzentrum München, ISBN: 978-3-86371-373-7 and the national clinic guideline for Diagnosis, staging and treatment of patients with breast cancer National clinic guideline for Diagnosis, staging and treatment of patients with breast cancer no. 7. 2015.
When diagnosed with breast cancer or it`s precancerous stages (LIN, DCIS) women need to undergo a certain path of diagnostic investigation and clinical examinations. After checking the medical history of the patient, the most important questions are:
1. What does the breast and it`s skin look like? Are there any palpable nodes? The clinical examination consisting of visualizing the patient and her breast especially concerning ulceration, inflammation, retraction of the NAC or skin above the tumor, Peaux d’orange, discharge of the nipple and palpation of both breasts in a certain manner as well as both lymphatic pathways, is essential.
2. What does the tumor look like using mammography and ultrasound? Is there one node or more?
The most important factors are the size and the location of the tumor, the distance to the skin and to the nipple-areola-complex. Furthermore, the axillary lymphatic nodes need to be checked for metastases. In some cases (e.g. higher density of the breast, implants, young patients) an MRI is needed.
3. What kind of breast cancer are we dealing with?
The majority is either from a ductal origin (DCIS/NST) or lobular (LIN/invasive lobular). There are also rare cases of non-epithelial tumors such as angio-/sarcoma or phylloidestumors. Additionally, information about hormone receptor expression, Her2 status, proliferation rate (marker Ki67) and grading (G1-G3) of the tumor is needed. Therefore, we need a histopathological result. A biopsy of the tumor and of suspect lymph nodes is taken under ultrasound or mammographic control.
4. Are there any distant metastases?
In particular we need a CT Thorax/Abdomen to check the liver and lung and a szintigraphy of the skeleton. Cerebral metastases should only be checked via cCT if we have any suspicion concerning cerebral failures
Breast cancer treatment in general and surgical S3 Guideline of German Cancer SocietyMSD Mannual Mannual for Breast Cancer of TU and LMU Munich 18. Auflage 2021, Tumorzentrum München, ISBN: 978-3-86371-373-7National clinic guideline for Diagnosis, staging and treatment of patients with breast cancer no. 7. 2015
With all the information together, a plan of treatment must be drawn up. In case of distant metastases, a systemic tumor therapy is indicated. In this chapter we want to have a deeper look in therapy of local breast cancer.
Considering the characteristics of the tumor we have different options to treat locally restricted cancer. For cancer with high proliferation rates (Ki67>25%) or medium proliferation rates (10-25%) plus poorly differented (G3) or aggressive tumor cells (triple negative), chemotherapy can be an option to improve the prognosis. If indicated, chemotherapy should be given in a neoadjuvant regime, first to shrink down the size of the node to improve the conditions for later planned surgery, second to check the tumor for response to chemotherapy. Best case taken, there are no tumorcells left after chemo (complete regression, °4 a. Sinn).
Further medicamentous therapies could be an antihormone therapy (adjuvant or primary in case of metastases) or antibodies (neo- and adjuvant, primary in case of metastases) in case of Her2 overexpression.
A lower proliferation rate given, surgery is the first choice in treating breast cancer. The aim of removing the cancer via surgery should always be an in-sano resection, meaning cancer-free resection margins in the histopathological examination. We will therefore have a deeper look in different techniques in the field of breast surgery.
Before we get into those, the surgical treatment of the axillary lymph nodes should be mentioned shortly. In every case of invasive cancer and as well in case of aggressive precancerous stages (e.g. high-risk DCIS) without clinical signs of lymph node metastases, the sentinel node should be removed and checked for tumorcells. If positive, an axillary dissection is indicated, unless there are only micro-metastases found in the sentinel node and radiotherapy is planned after surgery. An axillary dissection is indicated as well, if there were positive lymphnodes (diagnosed with biopsy) in the first place. Depending on how many lymph nodes (>3) are affected, a radiotherapy of the axillary lymphatic pathway is indicated, no matter if the breast needs radiation or not. To reduce the risk of local recurrence, irradiation can be discussed as well for 0-3 lymph nodes infiltrated, especially when radiotherapy is planned anyway after BCT.
Considering the characteristics of the tumor we have different options to treat locally restricted cancer. For cancer with high proliferation rates (Ki67>25%) or medium proliferation rates (10-25%) plus poorly differented (G3) or aggressive tumor cells (triple negative), chemotherapy can be an option to improve the prognosis. If indicated, chemotherapy should be given in a neoadjuvant regime, first to shrink down the size of the node to improve the conditions for later planned surgery, second to check the tumor for response to chemotherapy. Best case taken, there are no tumorcells left after chemo (complete regression, °4 a. Sinn).
Further medicamentous therapies could be an antihormone therapy (adjuvant or primary in case of metastases) or antibodies (neo- and adjuvant, primary in case of metastases) in case of Her2 overexpression.
A lower proliferation rate given, surgery is the first choice in treating breast cancer. The aim of removing the cancer via surgery should always be an in-sano resection, meaning cancer-free resection margins in the histopathological examination. We will therefore have a deeper look in different techniques in the field of breast surgery.
Before we get into those, the surgical treatment of the axillary lymph nodes should be mentioned shortly. In every case of invasive cancer and as well in case of aggressive precancerous stages (e.g. high-risk DCIS) without clinical signs of lymph node metastases, the sentinel node should be removed and checked for tumorcells. If positive, an axillary dissection is indicated, unless there are only micro-metastases found in the sentinel node and radiotherapy is planned after surgery. An axillary dissection is indicated as well, if there were positive lymphnodes (diagnosed with biopsy) in the first place. Depending on how many lymph nodes (>3) are affected, a radiotherapy of the axillary lymphatic pathway is indicated, no matter if the breast needs radiation or not. To reduce the risk of local recurrence, irradiation can be discussed as well for 0-3 lymph nodes infiltrated, especially when radiotherapy is planned anyway after BCT.
Breast Conserving Therapy (BCT)S3 Guideline of German Cancer SocietyMSD Mannual Mannual for Breast Cancer of TU and LMU Munich 18. Auflage 2021, Tumorzentrum München, ISBN: 978-3-86371-373-7National clinic guideline for Diagnosis, staging and treatment of patients with breast cancer no. 7. 2015
This leads us to the -in these days- most common technique to remove breast cancer surgically: Breast-conserving therapy (BCT). Most women are diagnosed in an early stage, when the tumor is small and hasn`t spread in other organs yet. The BCT is a good option for preserving the breast as an important part of a woman`s body. The cancer, if not palpable through the skin, needs to be marked by a needle under ultrasound or mammographic control right before surgery. The incision can be either made directly in the region of the cancer or – which is more aesthetically pleasing- around the NAC, inframammary or laterocaudal where the scar is almost invisible. The local lack of breast tissue after removing the tumor can be closed by mobilizing surrounding tissue and form local flaps to compensate the defect. This technique requires radiotherapy after surgery to reduce the risk of local cancer recurrence. The indication for BCT should be discussed with the patient and can be offered for all local invasive cancers and its prestages when it seems to be completely removable. The relation between the size of the tumor and the size of the breast plays a key role for the decision whether a BCT is able to remove the cancer completely and if the aesthetic result will be satisfying. Otherwise a mastectomy with or without reconstruction is the better and safer way to go.
Mastectomy
The Indication for mastectomy is given under the following circumstances:S3 Guideline of German Cancer SocietyMSD Mannual Mannual for Breast Cancer of TU and LMU Munich 18. Auflage 2021, Tumorzentrum München, ISBN: 978-3-86371-373-7National clinic guideline for Diagnosis, staging and treatment of patients with breast cancer no. 7. 2015
A patient`s request
, rejection/inability of radiotherapy, multifocal/multicentric carcinoma, which can’t be removed completely by BCT, adverse breast/tumor size-ratioMannual for Breast Cancer of TU and LMU Munich 18. Auflage 2021, Tumorzentrum München, ISBN: 978-3-86371-373-7inflammatory breast cancer, ulcerated breast carcinoma, genetic mutations like BRCA1/2 with or without breast cancer already occurred (relative contraindication for BCT, high risk of recurrence or second carcinoma). In 1882 Dr. William Stewart Halsted performed the first Radical Mastectomies and published his experiences and results in New York. This technique included removing the breast, the major and minor pectoralis muscle, the axillary and parasternal lymphnodes. A large wound with a high rate for complications (e.g. wound infections, impairment of wound healing chronic pain, lymphedema) was the result. Often a primary closure was not possible because of lacking skin left. Vacuum dressings, a second surgery or full thickness skin grafts were needed. This technique was mainly performed until the 1970s. Evolution of radical mastectomy for breast cancer. J Med Life 2016;9(2):183–6, The changing face of mastectomy (from muti- lation to aid to breast reconstruction). Int J Surg Oncol 2011:980158
Other surgeons tried to modify this aggressive method by perceiving the pectoralis muscle and by performing an axillary dissection only including level I and II. Level III could be left in situ if not clinically involved. Modified radical mastectomy. Annals of Surgery, 1972;175(5):624–34
In 1979 modified radical mastectomy became the new standard in treating breast cancer. This technique includes the removal of the breast with NAC and overlaying skin, pectoralis fascia, lymphnodes of level I and II. These days, the Sentinel-Method is mainly used before removing level I and II. Performing a modified radical mastectomy either combined with a sentinel node biopsy or even without operating on lymphnodes at all is also known as “Ablatio simplex” or simple mastectomy.
So far, all techniques had an elliptical, vertical incision around the NAC and the tumor in common, which makes it difficult to reconstruct the breast or sometimes even to close the wound in the first surgery.
1991 Toth and Lappert first developed a skin-sparing technique. The incision is made around the NAC or inframammary with modifications depending on the tumor location. This method is contraindicated for skin-infiltrating tumors, inflammatory or exulcerating breast cancer. Furthermore, adjuvant irradiation causing bad skin quality can be a contraindication. (Gerber et all published a study in 2003 showing that Nipple-sparing mastectomy is an option in breast cancer surgery, too. The Incision can be made- depending on tumor location and size of the breast- either inframammary, vertical or inferolateral or around the NAC with extension of the incision (CAVE: risk of necrosis).
For large ptotic breasts a Wise pattern technique can be used. The mastectomy is then performed using an incision around the NAC or vertical in the Wise pattern area. To reconstruct the breast in its new form, an expander is used, placed under the pectoralis muscle. The Wise pattern cut can also be used for breast conserving therapy in large breasts. What is left from the outside is only a scar inframammary and if necessary, around the NAC.
Increased satisfaction is shown in patients with Nippel-sparing mastectomy. They seem to have a superior well-being in general, mainly because of the superior aesthetic result after reconstruction and the less invasive method compared to radical modified mastectomy.
Contraindications are the same as for skin sparing mastectomies in addition of NAC infiltrating cancer, included Morbus Paget of the Nipple. The location of the tumor seems not to be that relevant as long as it’s not right behind the NAC and as the histopathological results show tumor-free resection margins.
Many studies discuss the oncological safety of nipple sparing mastectomy until today. Long time data is still missing. As written before, there is a general agreement about when to remove the NAC (infiltrating tumor, tumor reaching the NAC margin, positive nipple discharge, sometimes other illnesses like diabetes mellitus, constant smoking e.g.). So far, there is no evidence that the oncological safety is compromised when these contraindications are respected.
The decision must be made individually and in close consultation between the patient, the gynecologist and the plastic surgeon. Long time data must be generated, before the nipple sparing mastectomy can become a new, well established standard in breast surgery.
A patient`s request
, rejection/inability of radiotherapy, multifocal/multicentric carcinoma, which can’t be removed completely by BCT, adverse breast/tumor size-ratioMannual for Breast Cancer of TU and LMU Munich 18. Auflage 2021, Tumorzentrum München, ISBN: 978-3-86371-373-7inflammatory breast cancer, ulcerated breast carcinoma, genetic mutations like BRCA1/2 with or without breast cancer already occurred (relative contraindication for BCT, high risk of recurrence or second carcinoma). In 1882 Dr. William Stewart Halsted performed the first Radical Mastectomies and published his experiences and results in New York. This technique included removing the breast, the major and minor pectoralis muscle, the axillary and parasternal lymphnodes. A large wound with a high rate for complications (e.g. wound infections, impairment of wound healing chronic pain, lymphedema) was the result. Often a primary closure was not possible because of lacking skin left. Vacuum dressings, a second surgery or full thickness skin grafts were needed. This technique was mainly performed until the 1970s. Evolution of radical mastectomy for breast cancer. J Med Life 2016;9(2):183–6, The changing face of mastectomy (from muti- lation to aid to breast reconstruction). Int J Surg Oncol 2011:980158
Other surgeons tried to modify this aggressive method by perceiving the pectoralis muscle and by performing an axillary dissection only including level I and II. Level III could be left in situ if not clinically involved. Modified radical mastectomy. Annals of Surgery, 1972;175(5):624–34
In 1979 modified radical mastectomy became the new standard in treating breast cancer. This technique includes the removal of the breast with NAC and overlaying skin, pectoralis fascia, lymphnodes of level I and II. These days, the Sentinel-Method is mainly used before removing level I and II. Performing a modified radical mastectomy either combined with a sentinel node biopsy or even without operating on lymphnodes at all is also known as “Ablatio simplex” or simple mastectomy.
So far, all techniques had an elliptical, vertical incision around the NAC and the tumor in common, which makes it difficult to reconstruct the breast or sometimes even to close the wound in the first surgery.
1991 Toth and Lappert first developed a skin-sparing technique. The incision is made around the NAC or inframammary with modifications depending on the tumor location. This method is contraindicated for skin-infiltrating tumors, inflammatory or exulcerating breast cancer. Furthermore, adjuvant irradiation causing bad skin quality can be a contraindication. (Gerber et all published a study in 2003 showing that Nipple-sparing mastectomy is an option in breast cancer surgery, too. The Incision can be made- depending on tumor location and size of the breast- either inframammary, vertical or inferolateral or around the NAC with extension of the incision (CAVE: risk of necrosis).
For large ptotic breasts a Wise pattern technique can be used. The mastectomy is then performed using an incision around the NAC or vertical in the Wise pattern area. To reconstruct the breast in its new form, an expander is used, placed under the pectoralis muscle. The Wise pattern cut can also be used for breast conserving therapy in large breasts. What is left from the outside is only a scar inframammary and if necessary, around the NAC.
Increased satisfaction is shown in patients with Nippel-sparing mastectomy. They seem to have a superior well-being in general, mainly because of the superior aesthetic result after reconstruction and the less invasive method compared to radical modified mastectomy.
Contraindications are the same as for skin sparing mastectomies in addition of NAC infiltrating cancer, included Morbus Paget of the Nipple. The location of the tumor seems not to be that relevant as long as it’s not right behind the NAC and as the histopathological results show tumor-free resection margins.
Many studies discuss the oncological safety of nipple sparing mastectomy until today. Long time data is still missing. As written before, there is a general agreement about when to remove the NAC (infiltrating tumor, tumor reaching the NAC margin, positive nipple discharge, sometimes other illnesses like diabetes mellitus, constant smoking e.g.). So far, there is no evidence that the oncological safety is compromised when these contraindications are respected.
The decision must be made individually and in close consultation between the patient, the gynecologist and the plastic surgeon. Long time data must be generated, before the nipple sparing mastectomy can become a new, well established standard in breast surgery.
Prophylactic Mastectomy
A prophylactic mastectomy can be indicated for risk reduction in case of genetic mutation (e.g. BRCA1/2), for women with high-density breasts and the risk for occult cancer (hard to diagnose via clinical and imaging techniques) and to reduce the risk of contralateral cancer. Contralateral mastectomy can be helpful for reconstructive results, as well. In most cases, a pleasing symmetry of both sides can only be generated by using the same technique on both breasts (e.g. implants on both sides). The incision can be made around the NAC (nipple-sparing mastectomy), inframammary or latero-caudal. Either way, the skin and NAC can be conserved.
Prophylactic mastectomy can lower the risk of breast cancer up to 90%. Nevertheless, every patient needs to be informed about the risk for carcinoma, that is still left and to be primed for the necessary precautions .
Various studies have proven that there is no evidence for a difference in overall survival and recurrence rates between BCT followed by radiotherapy and mastectomy.
Example given, a study from 2005 from Muggendorfer et al. included n=1574 women who underwent breast surgery between 1963 and 1998 after being diagnosed with invasive breast cancer. N=787 had a mastectomy, the same amount of n=787 BCT followed by irradiation. The publisher retrospectively matched pairs of patients of each group regarding their tumor state, size, nodal state, grading and tumor biology. The first interesting findings were non-significant results when comparing the sizes of the tumors between both groups and when comparing the lymph node status. We can therefore presume that both groups had equal preconditions and that the results compare well. Results concerning the 5-year-survival did not show a significant difference, neither in the group of pT1b carcinomas (96,9% (BET) and 96,6% (ME), p=0,77), nor in the group of pT2 carcinomas (89,3% (BET) und 85,4% (ME), p=0,64). Free from locoregional cancer recurrence in 5 years after surgery were 92,9% (BET) and 92,4% (ME), as well no significant difference.
Prophylactic mastectomy can lower the risk of breast cancer up to 90%. Nevertheless, every patient needs to be informed about the risk for carcinoma, that is still left and to be primed for the necessary precautions .
Various studies have proven that there is no evidence for a difference in overall survival and recurrence rates between BCT followed by radiotherapy and mastectomy.
Example given, a study from 2005 from Muggendorfer et al. included n=1574 women who underwent breast surgery between 1963 and 1998 after being diagnosed with invasive breast cancer. N=787 had a mastectomy, the same amount of n=787 BCT followed by irradiation. The publisher retrospectively matched pairs of patients of each group regarding their tumor state, size, nodal state, grading and tumor biology. The first interesting findings were non-significant results when comparing the sizes of the tumors between both groups and when comparing the lymph node status. We can therefore presume that both groups had equal preconditions and that the results compare well. Results concerning the 5-year-survival did not show a significant difference, neither in the group of pT1b carcinomas (96,9% (BET) and 96,6% (ME), p=0,77), nor in the group of pT2 carcinomas (89,3% (BET) und 85,4% (ME), p=0,64). Free from locoregional cancer recurrence in 5 years after surgery were 92,9% (BET) and 92,4% (ME), as well no significant difference.
Irradiation
Adjuvant irradiation of the breast is strongly indicated in any case of invasive cancer removed breast conserving. Further indications for radiotherapy are a pT4 stadium and a R1/R2 situation after mastectomy without any surgical possibilities.
The indication can be discussed with patients when dealing with a high risk DCIS for risk reduction.
Radiotherapy including the breast and the lymphatic pathway (axillary, supra- and infraclavicular), regardless of which operation method was used, is indicated for over 3 affected lymph nodes after axillary dissection. When 1-3 lymph nodes are affected, radiotherapy is also indicated for high risk cancer types (G3, triple negative, high Ki67% S3 Guideline of German Cancer Society
A meta-analysis about the “effect of radiotherapy after breast conserving surgery” describes an absolute risk reduction for breast-cancer caused mortality from 3,3% for pN0 and 8.5% for pN+ carcinoma after 15 years.
Furthermore, the patients would have a much higher risk of local recurrence after BCT without radiotherapy. It is even discussed, if radiotherapy can reduce the risk of new carcinomas.
The general side-effects of radiotherapy are low, only a few get irradiation inducted pneumonitis. Negative impacts on the heart are not a problem anymore with modern techniques and accurate planning of the irradiation field. What’s left -and not to be left beside- is the severe damage of the skin. Radiotherapy causes often a change of color of the skin, bad skin quality (thin or rigid, stiff skin), pain and sensible deficits and therefore restricted mobility in the chest-arm-area.
Because of impaired skin quality and wound healing combined with higher complication risks after irradiation, the reconstruction-technique has to be adjusted. Therefore it doesn’t matter, when the radiotherapy was performed. Especially concerning implant-based reconstruction, the complication rate is much higher. While implant reconstruction after radiotherapy often causes fibrosis, capsular contraction, malpositioning of the implant, autologous flaps may present necrosis, atrophy and contracture.
Chemotherapy does not seem to have significant influence on reconstructive results, even though it can cause impaired and elongated wound healing. (30)
In conclusion, the right choice for breast reconstruction is about timing, technique, a patients` medical history and condition and has to be made after interdisciplinary consultation.
The indication can be discussed with patients when dealing with a high risk DCIS for risk reduction.
Radiotherapy including the breast and the lymphatic pathway (axillary, supra- and infraclavicular), regardless of which operation method was used, is indicated for over 3 affected lymph nodes after axillary dissection. When 1-3 lymph nodes are affected, radiotherapy is also indicated for high risk cancer types (G3, triple negative, high Ki67% S3 Guideline of German Cancer Society
A meta-analysis about the “effect of radiotherapy after breast conserving surgery” describes an absolute risk reduction for breast-cancer caused mortality from 3,3% for pN0 and 8.5% for pN+ carcinoma after 15 years.
Furthermore, the patients would have a much higher risk of local recurrence after BCT without radiotherapy. It is even discussed, if radiotherapy can reduce the risk of new carcinomas.
The general side-effects of radiotherapy are low, only a few get irradiation inducted pneumonitis. Negative impacts on the heart are not a problem anymore with modern techniques and accurate planning of the irradiation field. What’s left -and not to be left beside- is the severe damage of the skin. Radiotherapy causes often a change of color of the skin, bad skin quality (thin or rigid, stiff skin), pain and sensible deficits and therefore restricted mobility in the chest-arm-area.
Because of impaired skin quality and wound healing combined with higher complication risks after irradiation, the reconstruction-technique has to be adjusted. Therefore it doesn’t matter, when the radiotherapy was performed. Especially concerning implant-based reconstruction, the complication rate is much higher. While implant reconstruction after radiotherapy often causes fibrosis, capsular contraction, malpositioning of the implant, autologous flaps may present necrosis, atrophy and contracture.
Chemotherapy does not seem to have significant influence on reconstructive results, even though it can cause impaired and elongated wound healing. (30)
In conclusion, the right choice for breast reconstruction is about timing, technique, a patients` medical history and condition and has to be made after interdisciplinary consultation.
02
Quality Management
Quality Assurance of Oncological Treatment S3 Guideline of German Cancer Society
To manage the quality of cancer treatment, every case of breast cancer gets registered in a national data bank. The information is supposed to be used for quality assurance. Every certified breast center gets a yearly report of their success and failures and an evaluation of general results from the data base. National and international comparison helps to enhance the quality of treatment and to detect gaps, faults and new insights.
The quality of the oncological therapy is mainly managed by tumor boards, where every case has to be presented and discussed interdisciplinary. The next step is to evaluate the success of each therapy. If it comes to any complications like unbearable side-effects, growth of the tumor or metastases under therapy, the regime has to be adjusted. As soon as one part of the therapy is done, the next part has to be planned and discussed. Each of these decisions is made within a tumor conference. Hence a patient is not only attended to by only one expert, but also specialists for different areas of expertise consult about the best therapy for each case.
After completion of the treatment, most patients are seen by their family doctor, gynecologist or oncologist for tumor after-care. Every patient gets a calendar when to go to clinical examination, ultrasound, mammography and so on. This concept aims to prevent second carcinoma, recurrence of the tumor, local or distant metastases or at least to detect them early. Adjuvant therapy like radiotherapy, antihormone therapy, chemo or antibodies can be evaluated and adjusted if necessary. Further on, the patient should be supported to improve their life-style and quality of life in general. The tumor after-care should be proceeded for at least 10 years.
There are some recommendations found in the newest S3 guideline S3 Guideline of German Cancer Society, which should help the patents during the healing process and to prevent recurrence or new cancer. They suggest for the patient to move a lot, do sports and to keep or get a normal weight. Of course, a well-balanced nutrition without alcohol or smoking should be a part of the process. It is known that obesity with an BMI > 25 and inactivity cause high risks for recurrence, metastases and of course overall morbidity. The risk of dying from cancer when overweight is also proven to be higher. Further on, side effects of systemic therapy and symptoms related to the disease like chronic fatigue, polyneuropathy and lymphedema can be improved by training, movement and physio-therapy.
[48]
The quality of the oncological therapy is mainly managed by tumor boards, where every case has to be presented and discussed interdisciplinary. The next step is to evaluate the success of each therapy. If it comes to any complications like unbearable side-effects, growth of the tumor or metastases under therapy, the regime has to be adjusted. As soon as one part of the therapy is done, the next part has to be planned and discussed. Each of these decisions is made within a tumor conference. Hence a patient is not only attended to by only one expert, but also specialists for different areas of expertise consult about the best therapy for each case.
After completion of the treatment, most patients are seen by their family doctor, gynecologist or oncologist for tumor after-care. Every patient gets a calendar when to go to clinical examination, ultrasound, mammography and so on. This concept aims to prevent second carcinoma, recurrence of the tumor, local or distant metastases or at least to detect them early. Adjuvant therapy like radiotherapy, antihormone therapy, chemo or antibodies can be evaluated and adjusted if necessary. Further on, the patient should be supported to improve their life-style and quality of life in general. The tumor after-care should be proceeded for at least 10 years.
There are some recommendations found in the newest S3 guideline S3 Guideline of German Cancer Society, which should help the patents during the healing process and to prevent recurrence or new cancer. They suggest for the patient to move a lot, do sports and to keep or get a normal weight. Of course, a well-balanced nutrition without alcohol or smoking should be a part of the process. It is known that obesity with an BMI > 25 and inactivity cause high risks for recurrence, metastases and of course overall morbidity. The risk of dying from cancer when overweight is also proven to be higher. Further on, side effects of systemic therapy and symptoms related to the disease like chronic fatigue, polyneuropathy and lymphedema can be improved by training, movement and physio-therapy.
[48]
Quality Assurance of Breast Reconstruction
Introduction
Reconstructive surgery after mastectomy has become the standard of care for postmastectomy patients. The symbolic loss of the breast is considered by many patients as an abandonment of sexual identity. In addition to functional advantages in everyday life, the restoration of the breast is a fundamental coping module for many patients in dealing with their disease. QM1 This makes it all the more important to develope standardized evidencebased procedures as part of quality management in the follow‐up of surgical breast reconstruction. The S3 guideline for the treatment of breast carcinoma recommends the following: "Every patient undergoing mastectomy should be informed about the possibility of immediate or subsequent breast reconstruction or foregoing reconstructive procedures." S3 Guideline of German Cancer Society. Nonetheless, no quality indicators on breast reconstruction are collected as part of breast cancer center certification. QM3 This represents a substantial gap in the quality assurance of patient care.
Objective quality indicators
According to the S3 guideline on breast reconstruction, the only established methods of objective evaluation of a surgical result in breast surgery include complication rates. 12 A study after breast reconstruction was able to show that both patients and the treating surgeons strive for symmetry of the breast.13Previous studies have already demonstrated the decisive psychosocial importance of visual breast symmetry for patients 1415. The objective symmetry assessment of the breast in the context of reconstructive breast surgery is often
performed using anthropomorphic measurements. In clinical practice, these are usually obtained manually with the aid of a measuring tape directly on the patient. The necessary measurement points (so‐called landmarks) are typically determined by palpation. This method is easy to use; however, the measured values obtained are subject to measurement errors and are difficult to reproduce. The determination of landmarks is subjective and
dependent on the experience of the examiner. Last but not least, this method is time consuming and can be uncomfortable for the patient. Due to rapid technological advances, three‐dimensional (3D) evaluation of optical symmetry results using digital anthropometry has become possible16 17. However, most of the software programs provided for digital anthropometry are either custom‐made and their use is often product specific or very time‐consuming due to lack of automatical process. See PlastiCademy chapter "Three-dimensional imaging of the breast"
performed using anthropomorphic measurements. In clinical practice, these are usually obtained manually with the aid of a measuring tape directly on the patient. The necessary measurement points (so‐called landmarks) are typically determined by palpation. This method is easy to use; however, the measured values obtained are subject to measurement errors and are difficult to reproduce. The determination of landmarks is subjective and
dependent on the experience of the examiner. Last but not least, this method is time consuming and can be uncomfortable for the patient. Due to rapid technological advances, three‐dimensional (3D) evaluation of optical symmetry results using digital anthropometry has become possible16 17. However, most of the software programs provided for digital anthropometry are either custom‐made and their use is often product specific or very time‐consuming due to lack of automatical process. See PlastiCademy chapter "Three-dimensional imaging of the breast"
Many studies evaluate the shape of the reconstructed breast but neglect the skin sensitivity. Claim of one of our studies was to compare this important part of reconstruction on two different techniques of mastectomy.sens
Ten patients underwent breast reconstruction with free abdominal perforator flap between 2011 and 2015 after conventional mastectomy (CM) and were compared with ten patients, who had a skin sparing mastectomy (SSM) with immediate reconstruction by DIEAP-flap during the same time interval. These two groups were matched by age, height, weight and the time between reconstruction and examination. The sensitivity of the skin was measured by Semmes-Weinstein-Filaments in the strength beginning from 0,07 g till 300 g for deep sensation. The skin sparing mastectomy combined with immediate reconstruction by DIEAP-flap provides an excellent therapeutic option for patients, who are suitable for this technique, which takes into account not only the form but also the sensitivity of the breast.
Ten patients underwent breast reconstruction with free abdominal perforator flap between 2011 and 2015 after conventional mastectomy (CM) and were compared with ten patients, who had a skin sparing mastectomy (SSM) with immediate reconstruction by DIEAP-flap during the same time interval. These two groups were matched by age, height, weight and the time between reconstruction and examination. The sensitivity of the skin was measured by Semmes-Weinstein-Filaments in the strength beginning from 0,07 g till 300 g for deep sensation. The skin sparing mastectomy combined with immediate reconstruction by DIEAP-flap provides an excellent therapeutic option for patients, who are suitable for this technique, which takes into account not only the form but also the sensitivity of the breast.
Subjective Quality Indicators
According to the S3 guideline on breast reconstruction, quality-of-life assesments are among the established methods of subjective evaluation of a surgical outcome in breast surgery.12 Validated general and specifdic quality-of -life examination questionnaires are used 81819
Anthropometry and the foundation of the "Digital Plastic Surgery Research Group"
Anthropometry (from Greek "anthropos", human, and "metron", measure) is the study of the determination and application of measurements on the human body. Measurements of the human body are a central part of our everyday clinical practice. By digitalizing the measurements, we expect more accuracy, reproducibility and objectifiability in plastic surgery.The "Digital Plastic Surgery Research Group", DPS for short, is a multidisciplinary researchgroup working on digitalization in plastic surgery technology. In a first project, members of ReMic (Regensburg Medical Image Computing) from the East Bavarian Technical Universityin cooperation with the University Center for Plastic Surgery Regensburg have set themselves the goal of using a 3D scan of the breast to automate anthropometric measurements in the future and to collect them completely digitally. The aim of this projectis therefore in particular the automatic detection of landmarks using a 3D model. Furthermore, new methods for objective symmetry assessment are to be developed andevaluated in the clinical environment.
Definition of a breast symmetry index 20
We defined the symmetry index for outcome assessment in breast reconstruction surgery. The idea behind the SI is to provide a robust analysis of breast symmetry. The described standardized protocol for anthropometric measurements combines N measurements into a benchmark when there are N measurements for the left and right mamma, where dLi (dRi) denotes the ith measurement of the left/right mamma ( i∈{1,2,...,n}). The SI is then defined as the mean of the ratios of N anthropometric measurements of both breasts. The SI is metrically scored with values ranging from 0 (worst) to 1 (best). It can be represented as a percentage by multiplying it by 100. In our study, seven anthropomorphicmeasures were compared with the SI (N = 7). The Landmarks were verified using another patient collective. This resulted in an improvement of the symmetry index.21
Validation of breast volumetry with 3D scans
To validate the volumetry software, we designed a study in which patients planning breast removal for oncological reasons are scanned preoperatively in three dimensions. We compare the volume and weight of the resected tissue after mastectomy with the preoperatively digitally calculated breast volume. Using 3D surface image to evaluate breast shape and volume is a quick, effective, and convenient method. The accuracy, reproducibility, and reliability of 3D surface imaging were comparable with MRI in our study. (in Print)
Our study takes us one step closer to the long‐term goal of establishing robust instruments to plan breast reconstructive surgery, achieve better surgical results and contribute to the quality assurance of breast surgery . This study would not have been possible without the support of OTH. We have established a multidisciplinary research group with medical informaticists and gynecologists, the Digital Plastic Surgery Research Group.
This year, in addition to clinical research, we were able to publish open source the world's first statistical model of the breast , the Shape Model of the Breast.16
Our study takes us one step closer to the long‐term goal of establishing robust instruments to plan breast reconstructive surgery, achieve better surgical results and contribute to the quality assurance of breast surgery . This study would not have been possible without the support of OTH. We have established a multidisciplinary research group with medical informaticists and gynecologists, the Digital Plastic Surgery Research Group.
This year, in addition to clinical research, we were able to publish open source the world's first statistical model of the breast , the Shape Model of the Breast.16
03
Algorithms of Breast Reconstruction after Mastectomy
Introduction
Following the indication for mastectomy, the indication for breast reconstruction can be given. Breast reconstruction provides psychological, social, emotional, and functional improvements and an opportunity to rebuild the natural shape of the body after breast cancer treatment. Breast reconstruction should be offered to every woman following a unilateral or bilateral mastectomy, or after breast conserving therapy that has had a less-than-ideal cosmetic result. Patients who choose breast reconstruction are presented with complex decisions, including the type and timing of reconstruction. We created some algorithms to give a better overview of the different pathways. The different surgical techniques of reconstructing the breast are discussed in separate chapters.
Algorithms
The current S3 guideline for the treatment of breast carcinoma S3contains little information on breast reconstruction. The proposed treatment algorithm dates from 2004 and has not considered recent quality‐of‐life outcomes. Particularly in adjuvant radiotherapy, autologous breast reconstruction has become the treatment of choicealgo 1 . Due to the natural feel and physiologic aging process, patients satisfaction has been shown to be higher with autologous breast reconstructionalgo 2. The guideline algorithm withholds the option of autologous reconstruction from patients without radiation or tissue defect. This approach no longer reflects current practice. Critical analysis of pre‐ and postoperative digital anthropometry data has allowed us to develope new treatment algorithms. Here is a newly developed treatment algorithm for breast reconstruction after
mastectomy:
mastectomy:
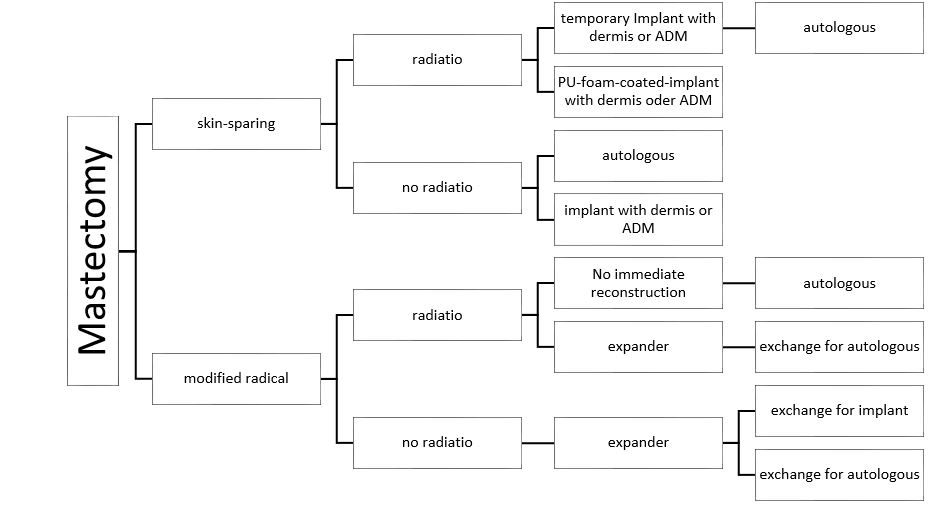
General algorithm for breast reconstruction after mastectomy
Whether the skin of the breast can be preserved depends on the tumor location: If the tumor is close to the skin, a modified radical mastectomy must be performed due to potential tumor infiltration of the skin. This decision is made by the oncological surgeon and corresponds to the first decision criterion in our algorithm. If the mastectomy can be performed skin‐sparingly, it is often possible to reconstruct the breast one time, so this has a
great advantage for the patient. Due to the repeatedly described complications of implant reconstruction and irradiation, radiotherapy has become a relative contraindication to allogenetic reconstruction.algo3 The planning of adjuvant radiotherapy or the status after irradiation of the breast significantly influences the strategy of breast reconstruction. For this reason, we decided to use irradiation (pre‐existing or planned) as a second decision criterion. In case of irradiation, we aim for autologous tissue reconstruction, two‐sided with insertion of a temporary prosthesis. If no radiotherapy has been or will be performed, both reconstruction techniques are possible, autologous and allogenic. This treatment algorithm forms the basis of our daily clinical actvities. Thanks to standardization, surgical results can be better compared with each other. Quality‐enhancing
measures can be taken accordingly.
great advantage for the patient. Due to the repeatedly described complications of implant reconstruction and irradiation, radiotherapy has become a relative contraindication to allogenetic reconstruction.algo3 The planning of adjuvant radiotherapy or the status after irradiation of the breast significantly influences the strategy of breast reconstruction. For this reason, we decided to use irradiation (pre‐existing or planned) as a second decision criterion. In case of irradiation, we aim for autologous tissue reconstruction, two‐sided with insertion of a temporary prosthesis. If no radiotherapy has been or will be performed, both reconstruction techniques are possible, autologous and allogenic. This treatment algorithm forms the basis of our daily clinical actvities. Thanks to standardization, surgical results can be better compared with each other. Quality‐enhancing
measures can be taken accordingly.
We noticed special needs in patients with breast carcinoma and micro- and macromastia
For these special cases we us two different algorithms:
For these special cases we us two different algorithms:
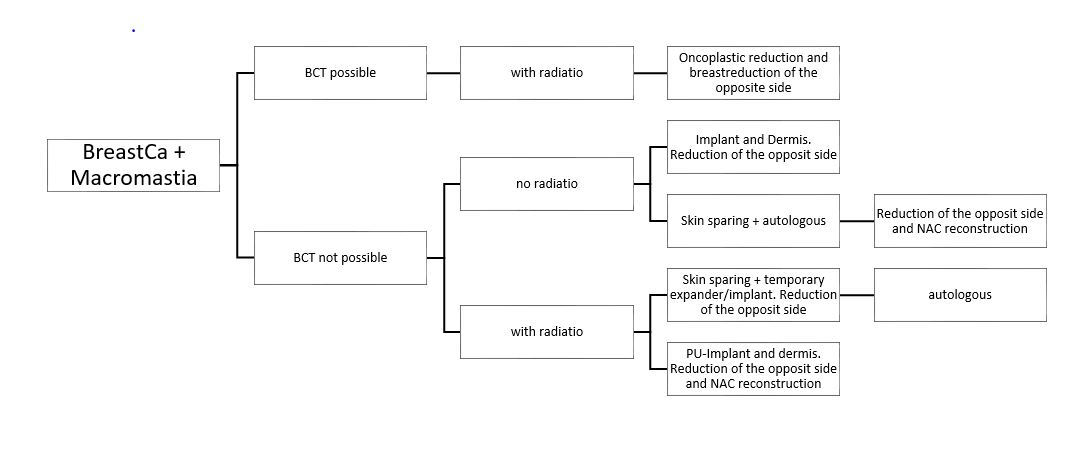
Algorithm Macromastia
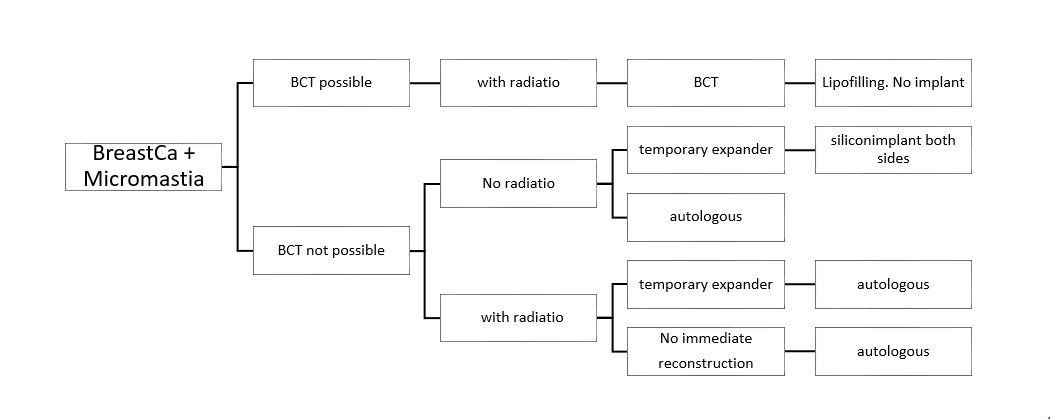
Algorithm Micromastia
04
Clinical Cases
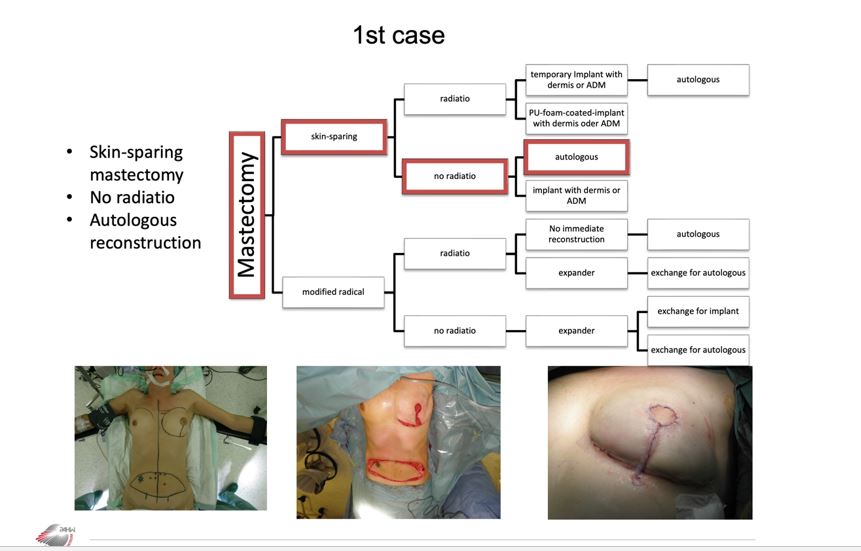
Case 1
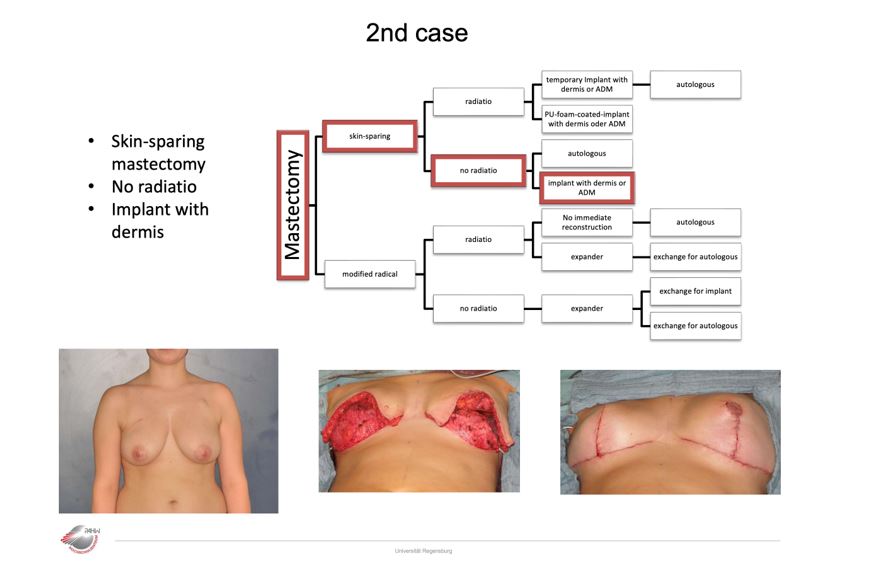
Case 2, 1
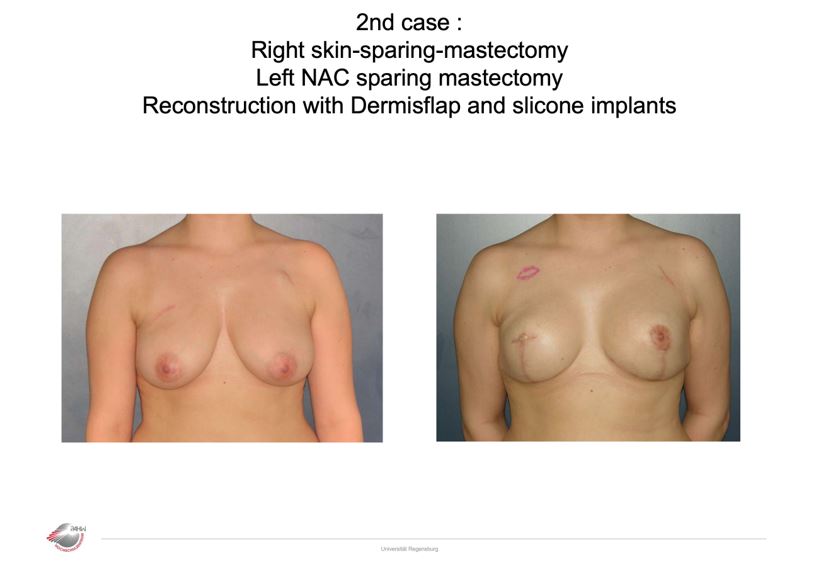
Case 2, 2
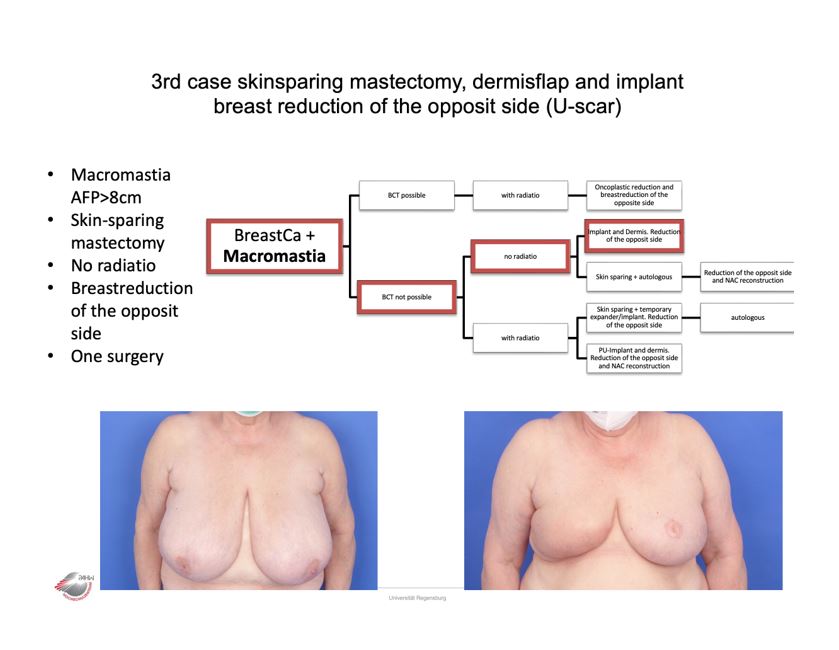
Case 3
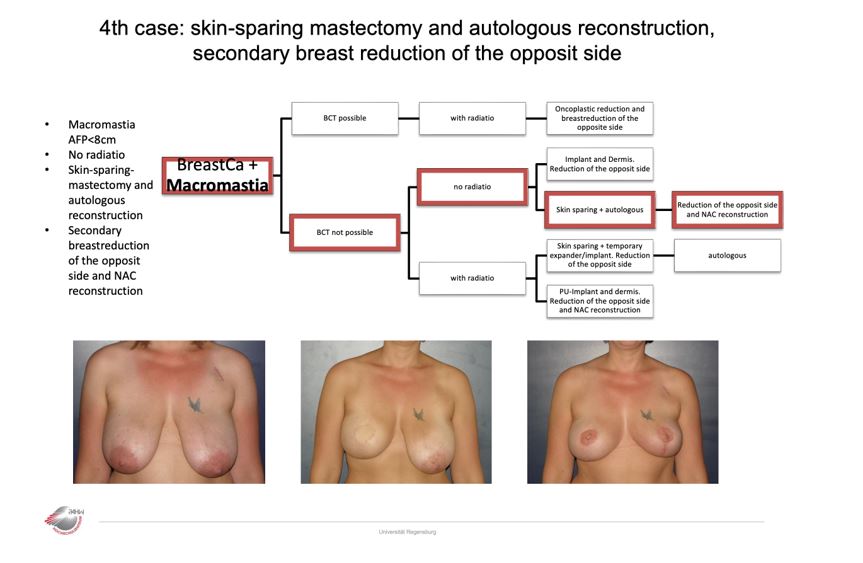
Case 4
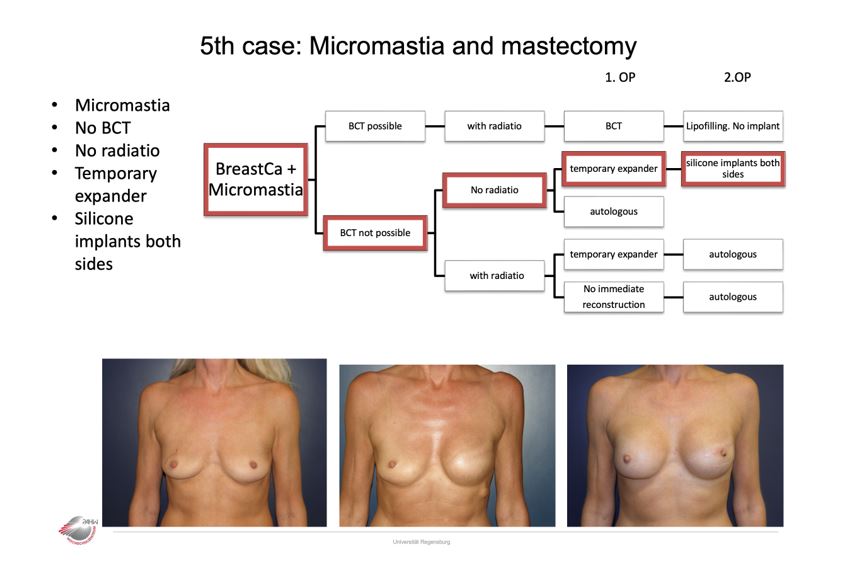
Case 5
05
Conclusion
Thanks to standardization, surgical results can be better compared with each other. Quality‐enhancing actions can be taken accordingly.
patients related outcome measures need to be completed by objective outcome parameters.
Perform skin- or nipple-sparing mastectomy if it is oncologically safe.
in case of planed postmastectomy radiatio, then discuss secondary reconstruction.
to achieve symmetry of texture, pay attention to the contralateral breast: both sides autolog, or both sides alloplastic
be aware of special needs of your patients: Macomastia, micromastia, obesity, diabetes...
Images
General algorithm for breast reconstruction after mastectomy
Algorithm Macromastia
Algorithm Micromastia
Videos
References
[1]
S3 Leitlinie Mammakarzinom , Leitlinienprogramm Onkologie der Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften e.V. (AWMF), Deutschen Krebsgesellschaft e.V. (DKG) und Deutschen Krebshilfe (DKH), AWMF Online , 2021
[2]
MSD Mannual for Breast cancer , Mary Ann Kosir, MD, Wayne State University School of Medicine, 2019
[3]
Manual Mammakarzinome , PD. Dr.med.J.Ettl et al. , Tumorzentrum München, 2021
[4]
National clinic guideline for Diagnosis, staging and treatment of patients with breast cancer, Department of Health., Committee, N.C.E., 2015
[5]
S3 Leitlinie Mammakarzinom , Leitlinienprogramm Onkologie der Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften e.V. (AWMF), Deutschen Krebsgesellschaft e.V. (DKG) und Deutschen Krebshilfe (DKH), AWMF Online , 2021
[6]
MSD Mannual for Breast cancer , Mary Ann Kosir, MD, Wayne State University School of Medicine, 2019
[7]
Manual Mammakarzinome , PD. Dr.med.J.Ettl et al. , Tumorzentrum München, 2021
[8]
National clinic guideline for Diagnosis, staging and treatment of patients with breast cancer, Department of Health., Committee, N.C.E., 2015
[9]
S3 Leitlinie Mammakarzinom , Leitlinienprogramm Onkologie der Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften e.V. (AWMF), Deutschen Krebsgesellschaft e.V. (DKG) und Deutschen Krebshilfe (DKH), AWMF Online , 2021
[10]
MSD Mannual for Breast cancer , Mary Ann Kosir, MD, Wayne State University School of Medicine, 2019
[11]
Manual Mammakarzinome , PD. Dr.med.J.Ettl et al. , Tumorzentrum München, 2021
[12]
National clinic guideline for Diagnosis, staging and treatment of patients with breast cancer, Department of Health., Committee, N.C.E., 2015
[13]
S3 Leitlinie Mammakarzinom , Leitlinienprogramm Onkologie der Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften e.V. (AWMF), Deutschen Krebsgesellschaft e.V. (DKG) und Deutschen Krebshilfe (DKH), AWMF Online , 2021
[14]
MSD Mannual for Breast cancer , Mary Ann Kosir, MD, Wayne State University School of Medicine, 2019
[15]
Manual Mammakarzinome , PD. Dr.med.J.Ettl et al. , Tumorzentrum München, 2021
[16]
National clinic guideline for Diagnosis, staging and treatment of patients with breast cancer, Department of Health., Committee, N.C.E., 2015
[17]
Manual Mammakarzinome , PD. Dr.med.J.Ettl et al. , Tumorzentrum München, 2021
[18]
Evolution of radical mastectomy for breast cancer, Plesca M, Bordea C, El Houcheimi B, et al., Journal of Medical Life , 2016
[19]
The changing face of mastectomy (from muti- lation to aid to breast reconstruction), Zurrida S, Bassi F, Arnone P, et al., International Journal of Surgical Oncology, 2011
[20]
Modified radical mastectomy, Madden JL, Kandalaft S, Bourque RA, Annals of Surgery, 1972
[21]
The Breast: Comprehensive Management of Benign and Malignant Disorders, Sainsbury R, Springer Science and Business Media LLC, 2004
[22]
The Breast: Comprehensive Management of Benign and Malignant Disorders, Sainsbury R, Springer Science and Business Media LLC, 2004
[23]
The Breast: Comprehensive Management of Benign and Malignant Disorders, Sainsbury R, Springer Science and Business Media LLC, 2004
[24]
Modified skin incisions for mastectomy: the need for plastic surgical input in preoperative planning, Toth BA, Lappert P, Plast Reconstr Surg, 1991
[25]
Skin-Sparing Mastectomy, Carlson Grant W., Bostwick John, Styblo Toncred M., Moore Bridgett, Bried Jean T., Murray Douglas R., Wood William C., Ovid Technologies (Wolters Kluwer Health), 1997
[26]
Skin-Sparing Mastectomy with Conservation of the Nipple–Areola Complex and Autologous Reconstruction is an Oncologically Safe Procedure, Gerber Bernd, Krause Annette, Reimer Toralf, Müller Heiner, Küchenmeister Ingrid, Makovitzky Joseph, Kundt Günther, Friese Klaus, Annals of Plastic Surgery , 2003
[27]
Reconstruction of the Ptotic Breast Using Wise Pattern Skin Deepithelialization, Newman Michael K., Ovid Technologies (Wolters Kluwer Health), Plast Reconstr Surg Glob Open ., 2016
[28]
Reconstruction of the Ptotic Breast Using Wise Pattern Skin Deepithelialization, Newman Michael K., Ovid Technologies (Wolters Kluwer Health), Plast Reconstr Surg Glob Open ., 2016
[29]
Nipple-Areola Reconstruction: Satisfaction and Clinical Determinants, Jabor Mark A., Shayani Payam, Collins Donald R., Karas Tomer, Cohen Benjamin E., Ovid Technologies (Wolters Kluwer Health), Plastic Reconstructive Surgery, 2002
[30]
Psychosocial and Sexual Well-Being Following Nipple-Sparing Mastectomy and Reconstruction, Wei Cindy H., Scott Amie M., Price Alison N., Miller Helen Catherine, Klassen Anne F., Jhanwar Sabrina M., Mehrara Babak J., Disa Joseph J., McCarthy Colleen, Matros Evan, Cordeiro Peter G., Sacchini Virgilio, Pusic Andrea L., Hindawi Limited, Breast Journal , 2016
[31]
Increasing Eligibility for Nipple-Sparing Mastectomy, Coopey Suzanne B., Tang Rong, Lei Lan, Freer Phoebe E., Kansal Kari, Colwell Amy S., Gadd Michele A., Specht Michelle C., Austen William G., Smith Barbara L., Springer Science and Business Media LLC, Annals of Surgical Oncology , 2013
[32]
Total Skin-Sparing Mastectomy and Immediate Breast Reconstruction: An Evolution of Technique and Assessment of Outcomes, Wang Frederick, Peled Anne Warren, Garwood Elisabeth, Fiscalini Allison Stover, Sbitany Hani, Foster Robert D., Alvarado Michael, Ewing Cheryl, Hwang E. Shelley, Esserman Laura J., Springer Science and Business Media LLC, Annals of Surgical Oncology , 2014
[33]
Outcomes after Total Skin-sparing Mastectomy and Immediate Reconstruction in 657 Breasts, Peled Anne Warren, Foster Robert D., Stover Allison C., Itakura Kaoru, Ewing Cheryl A., Alvarado Michael, Hwang E. Shelley, Esserman Laura J., Springer Science and Business Media LLC, Annals of Surgical Oncology , 2012
[34]
Oncologic Safety of Prophylactic Nipple-Sparing Mastectomy in a Population With BRCA Mutations, Jakub James W., Peled Anne Warren, Gray Richard J., Greenup Rachel A., Kiluk John V., Sacchini Virgilio, McLaughlin Sarah A., Tchou Julia C., Vierkant Robert A., Degnim Amy C., Willey Shawna, American Medical Association (AMA), JAMA Surg. , 2018
[35]
Total Skin-Sparing Mastectomy, Piper Merisa, Peled Anne Warren, Foster Robert D., Moore Dan H., Esserman Laura J., Ovid Technologies (Wolters Kluwer Health), Annals of Plastic Surgery , 2013
[36]
Position Statement on Prophylactic Mastectomy. Approved by the Society of Surgical Oncology Executive Council, March 2007, Giuliano Armando E., Boolbol Susan, Degnim Amy, Kuerer Henry, Leitch A. Marilyn, Morrow Monica, Springer Science and Business Media LLC, Annals of Surgical Oncology , 2007
[37]
Nipple-sparing mastectomy in patients with BRCA1/2 mutations and variants of uncertain significance, Manning A T, Wood C, Eaton A, Stempel M, Capko D, Pusic A, Morrow M, Sacchini V, Oxford University Press (OUP), The British Journal of Surgery, 2015
[38]
Prophylactic mastectomy: Who needs it, when and why, Burke Erin E., Portschy Pamela R., Tuttle Todd M., Wiley, Journal of surgical Oncology , 2015
[39]
Brusterhaltende Therapie versus Mastektomie beim Mammakarzinom: Langzeitergebnisse einer Matched-Pair-Analyse, LMU München, MD Muggendorfer, R., et al, Universitätsbibliothek LMU München , 2005
[40]
S3 Leitlinie Mammakarzinom , Leitlinienprogramm Onkologie der Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften e.V. (AWMF), Deutschen Krebsgesellschaft e.V. (DKG) und Deutschen Krebshilfe (DKH), AWMF Online , 2021
[41]
Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10 801 women in 17 randomised trials, S Darby, P McGale, C Correa, C Taylor, R Arriagada, M Clarke, D Cutter, C Davies, M Ewertz, J Godwin, R Gray, L Pierce, T Whelan, Y Wang, R Peto, Elsevier BV, Lancet , 2011
[42]
Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10 801 women in 17 randomised trials, S Darby, P McGale, C Correa, C Taylor, R Arriagada, M Clarke, D Cutter, C Davies, M Ewertz, J Godwin, R Gray, L Pierce, T Whelan, Y Wang, R Peto, Elsevier BV, Lancet , 2011
[43]
Five year outcomes of hypofractionated simultaneous integrated boost irradiation in breast conserving therapy; patterns of recurrence, Bantema-Joppe Enja J., Vredeveld Eline J., de Bock Geertruida H., Busz Dianne M., Woltman-van Iersel Marleen, Dolsma Wil V., van der Laan Hans Paul, Langendijk Johannes A., Maduro John H., Elsevier BV,Journal of Radiotherapy and Oncology , 2013
[44]
SKIN AND SUBCUTANEOUS ADIPOSE TISSUE DAMAGE AFTER RADIATION THERAPY IN BREAST CANCER PATIENTS, Bazyka D., , Litvinenko O., Bugaytsov S., Shakhrai G., National Research Center for Radiation Medicine of the NAMS of Ukraine, 2021
[45]
Impact of Radiotherapy on Complications and Patient-Reported Outcomes After Breast Reconstruction, Jagsi Reshma, Momoh Adeyiza O., Qi Ji, Hamill Jennifer B., Billig Jessica, Kim Hyungjin M., Pusic Andrea L., Wilkins Edwin G., Oxford University Press (OUP), Journal of the National Cancer Institute , 2018
[46]
A Systematic Review of Morbidity Associated with Autologous Breast Reconstruction Before and After Exposure to Radiotherapy: Are Current Practices Ideal?, Kelley Brian P., Ahmed Raouf, Kidwell Kelley M., Kozlow Jeffrey H., Chung Kevin C., Momoh Adeyiza O., Springer Science and Business Media LLC, Annals of Surgical Oncology , 2014
[47]
S3 Leitlinie Mammakarzinom , Leitlinienprogramm Onkologie der Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften e.V. (AWMF), Deutschen Krebsgesellschaft e.V. (DKG) und Deutschen Krebshilfe (DKH), AWMF Online , 2021
[48]
S3 Leitlinie Mammakarzinom , Leitlinienprogramm Onkologie der Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften e.V. (AWMF), Deutschen Krebsgesellschaft e.V. (DKG) und Deutschen Krebshilfe (DKH), AWMF Online , 2021
[49]
Effect of Obesity on Prognosis After Early-Stage Breast Cancer, Ewertz Marianne, Jensen Maj-Britt, Gunnarsdóttir Katrín Á., Højris Inger, Jakobsen Erik H., Nielsen Dorte, Stenbygaard Lars E., Tange Ulla B., Cold Søren, American Society of Clinical Oncology (ASCO), Journal of Clinical Oncology , 2011
[50]
Differences between women who have and have not undergone breast reconstruction after mastectomy due to breast cancer, Fallbjörk Ulrika, Karlsson Stig, Salander Pär, Rasmussen Birgit H., Informa UK Limited, 2010
[51]
S3 Leitlinie Mammakarzinom , Leitlinienprogramm Onkologie der Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften e.V. (AWMF), Deutschen Krebsgesellschaft e.V. (DKG) und Deutschen Krebshilfe (DKH), AWMF Online , 2021
[52]
Deutsche Krebsgesellschaft Kennzahlenauswertung 2020 - Jahresbericht der zertifizierten Brustkrebszentren, , ,
[53]
Brodkorb T 015/075 Leitlinie für Brustrekonstruktion mit Eigengewebe. 93, , ,
[54]
Symmetrical Breast Reconstruction: Is There a Role for Three-Dimensional Digital Photography?, Nahabedian Maurice Y., Galdino Gregory, Ovid Technologies (Wolters Kluwer Health), 2003
[55]
The Impact of Surgical Treatment on the Self-Esteem of Patients with Breast Hypertrophy, Hypomastia, or Breast Asymmetry, Neto Miguel Sabino, Abla Luiz Eduardo Felipe, Lemos Ana Lucia, Garcia Élvio Bueno, Enout Mariana Junqueira Reis, Cabral Nádia Canale, Ferreira Lydia Masako, Springer Science and Business Media LLC, 2012
[56]
A novel method to assess breast shape and breast asymmetry, Pei Jie, Fan Jintu, Ashdown Susan P., Informa UK Limited, 2019
[57]
The Role of Three-Dimensional Scanning Technique in Evaluation of Breast Asymmetry in Breast Augmentation: A 100-Case Study, Liu Chunjun, Luan Jie, Mu Lanhua, Ji Kai, Ovid Technologies (Wolters Kluwer Health), 2010
[58]
Is Unilateral Implant or Autologous Breast Reconstruction Better in Obtaining Breast Symmetry?, Cohen Oriana, Small Kevin, Lee Christina, Petruolo Oriana, Karp Nolan, Choi Mihye, Hindawi Limited, 2016
[59]
Breast sensitivity after mastectomy and autologous reconstruction, Heine Norbert, Koch Christoph, Brebant Vanessa, Kehrer Andreas, Anker Alexandra, Prantl Lukas, IOS Press, 2017
[60]
Brodkorb T 015/075 Leitlinie für Brustrekonstruktion mit Eigengewebe. 93, , ,
[61]
The BREAST-Q in surgical research: A review of the literature 2009–2015, Cohen Wess A., Mundy Lily R., Ballard Tiffany N.S., Klassen Anne, Cano Stefan J., Browne John, Pusic Andrea L., Elsevier BV, 2016
[62]
Development of a New Patient-Reported Outcome Measure for Breast Surgery: The BREAST-Q, Pusic Andrea L., Klassen Anne F., Scott Amie M., Klok Jennifer A., Cordeiro Peter G., Cano Stefan J., Ovid Technologies (Wolters Kluwer Health), 2009
[63]
Use of the BREAST-Q in Clinical Outcomes Research, Pusic Andrea L., Klassen Anne F., Cano Stefan J., Ovid Technologies (Wolters Kluwer Health), 2012
[64]
A Novel Method of Outcome Assessment in Breast Reconstruction Surgery: Comparison of Autologous and Alloplastic Techniques Using Three-Dimensional Surface Imaging, Hartmann Robin, Weiherer Maximilian, Schiltz Daniel, Seitz Stephan, Lotter Luisa, Anker Alexandra, Palm Christoph, Prantl Lukas, Brébant Vanessa, Springer Science and Business Media LLC, 2020
[65]
New aspects in digital breast assessment: further refinement of a method for automated digital anthropometry, Hartmann Robin, Weiherer Maximilian, Schiltz Daniel, Baringer Magnus, Noisser Vivien, Hösl Vanessa, Eigenberger Andreas, Seitz Stephan, Palm Christoph, Prantl Lukas, Brébant Vanessa, Springer Science and Business Media LLC, 2021
[66]
The Role of Three-Dimensional Scanning Technique in Evaluation of Breast Asymmetry in Breast Augmentation: A 100-Case Study, Liu Chunjun, Luan Jie, Mu Lanhua, Ji Kai, Ovid Technologies (Wolters Kluwer Health), 2010
[67]
S3 Leitlinie Mammakarzinom. AWMF (2021), , ,
[68]
, , ,
[69]
Breast Reconstruction in Previously Irradiated Patients Using Tissue Expanders and Implants: A Potentially Unfavorable Result, Forman Douglas L., Chiu Jennifer, Restifo Richard J., ward Barbara A., Haffty Bruce, Ariyan Stephen, Ovid Technologies (Wolters Kluwer Health), 1998
[70]
Outcome of Quality of Life for Women Undergoing Autologous versus Alloplastic Breast Reconstruction following Mastectomy: A Systematic Review and Meta-Analysis, Eltahir Yassir, Krabbe-Timmerman Irene S., Sadok Nadia, Werker Paul M. N., de Bock Geertruida H., Ovid Technologies (Wolters Kluwer Health), 2020
[71]
The Impact of Postmastectomy Radiotherapy on Two-Stage Implant Breast Reconstruction, Cordeiro Peter G., Albornoz Claudia R., McCormick Beryl, Hu Qunying, Van Zee Kimberly, Ovid Technologies (Wolters Kluwer Health), 2014